Translate this page into:
When bones deceive: Beyond skeletal dysplasia
*Corresponding author: Harshitha Harish Shetty, Department of Radiology, Seth GS Medical College and King Edward Memorial (KEM) Hospital, Mumbai, Maharashtra, India. harshitha.radiology@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kale SV, Khan SA, Shetty HH. When bones deceive: Beyond skeletal dysplasia. Case Rep Clin Radiol. doi: 10.25259/CRCR_174_2023
Abstract
Congenital hypothyroidism results from a partial or complete loss of thyroid function. It is the most common treatable cause of mental retardation. Thyroid hormone facilitates the growth and development of the skeleton through its direct effects on chondrocyte proliferation and differentiation and its permissive effects on the growth hormone. Due to the congenital hypothyroidism screening programs, congenital hypothyroidism is rare, and hence, other differential diagnoses are often considered in children presenting later in life with short stature and coarse facies such as storage disorders, genetic disorders, and skeletal dysplasia. This article aims to assess and discuss the value of radiology, especially plain radiography and ultrasonography in the diagnosis of congenital hypothyroidism and prevent long-term mental retardation and neurological dysfunction.
Keywords
Short stature
Skeletal survey
Delayed bone age
Thyroid dysgenesis
Epiphyseal dysplasia
INTRODUCTION
Congenital hypothyroidism can be caused either by a problem with the development of the thyroid gland (dysgenesis) or the synthesis of thyroid hormones (dyshormonogenesis). As clinical symptoms in neonates are minimal or absent, screening of all the neonates is important by a dried blood spot screening test. A heel stick is performed to evaluate the levels of thyroid stimulating hormone (TSH) and all the patients with a high value of TSH are assumed to have congenital hypothyroidism unless proven otherwise.[1] The most common cause of congenital hypothyroidism in underdeveloped countries is iodine deficiency but in the developed world, most cases are caused by thyroid dysgenesis – aplasia, hypoplasia, or ectopia.
CASE REPORT
A 5-year-old girl born out of a third-degree consanguineous marriage was brought by her parents with complaints of developmental delay, failure to thrive, chronic constipation, and progressive abdominal distension for the past 3 years. On examination, she had a short stature, coarse dull facies, a protruding tongue, and a distended abdomen with generalized hypotonia and global developmental delay [Figure 1]. She could sit with support but not stand or walk. Weight for height was <3rd centile for her age.

- (a) Clinical photograph of the 5-year-old girl brought by her parents shows dull, myxedematous facies with a broad nose. (b) Same child after 6 weeks of initiation of treatment with levothyroxine.
Clinically, a storage disorder like mucopolysaccharidosis or mucolipidosis was suspected and the child underwent a skeletal survey for the same. Radiographs of the skull, spine, and upper and lower limbs were taken.
On frontal and lateral views of the skull, there are persistent large fontanelles with widened sutures. There is nonpneumatization of the paranasal sinuses. Obtuse mandibular angles are seen [Figure 2a]. A Wormian bone is seen along the lambdoid suture [Figure 2b]. The density of the bones is normal. A frontal radiograph of the abdomen reveals colonic fecal burden. The disc gaps and spine’s curvature are both normal [Figure 2c]. With delayed bone age, rhizomelic shortening of the upper and lower limbs is observed. Both the femoral capital epiphysis and the head of the humerus are not ossified. The proximal tibial epiphyses as well as the distal femoral epiphyses are asymmetrical and tiny. There is a metaphyseal abnormality in the proximal humerus. The carpal bones are not ossified. There is no proximal metacarpal pointing sign. There is a thickening of the cortex with a narrowing of the medullary canal [Figure 3].
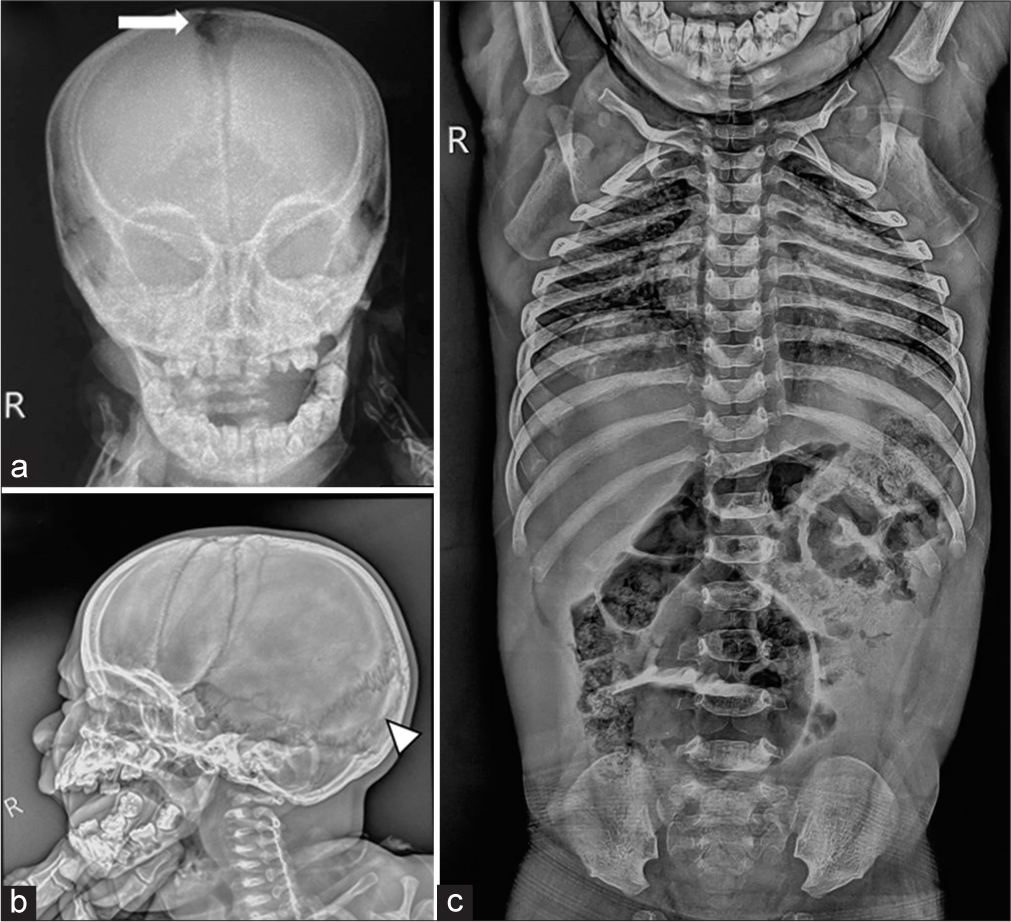
- (a) Frontal radiograph of the skull shows persistent large anterior fontanelle (white arrow). There is non-pneumatisation of the paranasal sinuses with hypoplastic facial bones. (b) Lateral radiograph of the skull shows a Wormian bone seen along the lambdoid suture (white arrowhead). There is obtuse mandibular angle. (c) Frontal radiograph of the abdomen shows faecal loading of the colon with normal disc spaces and curvature of the spine.
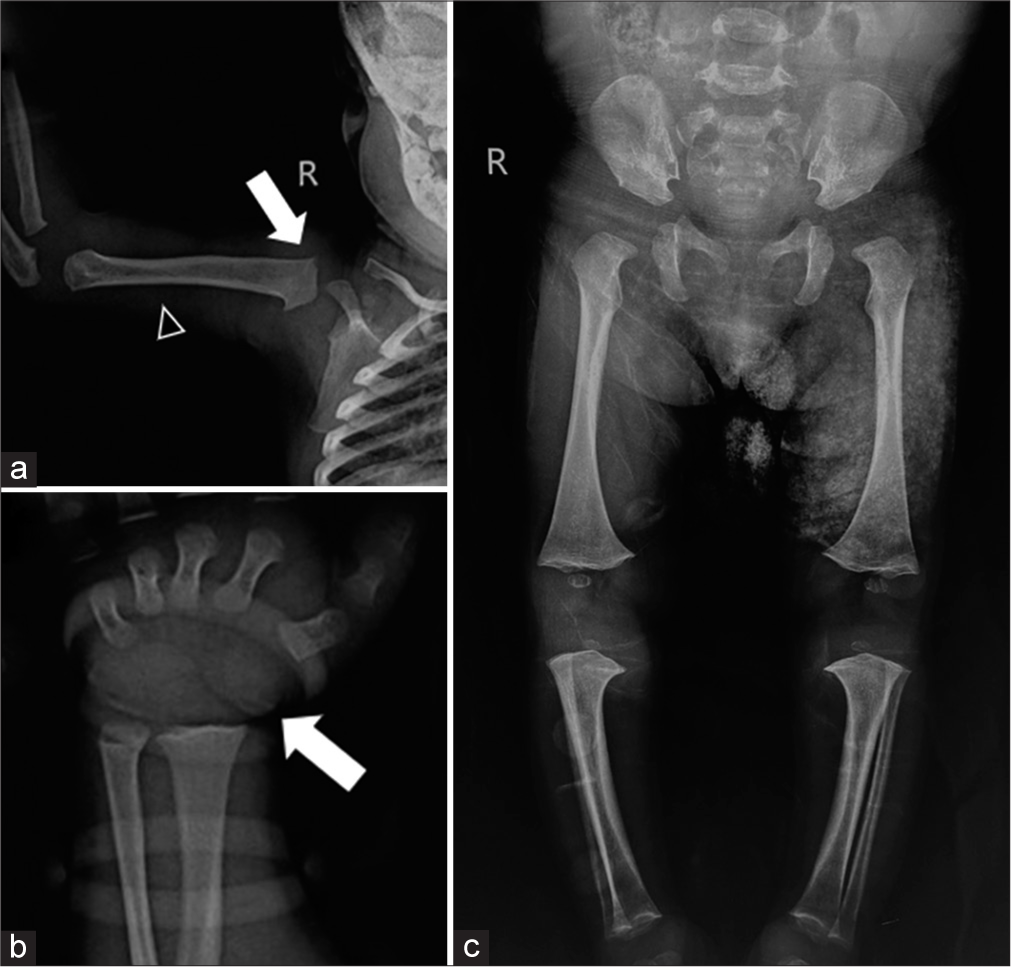
- (a) Radiograph of the upper limb shows non-ossification of the head of the humerus (white arrow). There is thickening of the cortex with narrowing of the medullary canal (black arrow heads). (b) Radiograph of the wrist shows non- ossification of the carpal bones (white arrow). (c) Radiograph of the lower limb shows non-ossification of the femoral capital epiphysis with small and dysplastic distal femoral and proximal tibial epiphysis.
Congenital hypothyroidism was suspected based on the clinical features combined with the radiographic findings. An ultrasound of the neck was performed to look for the status of the thyroid gland. The thyroid gland was absent in the neck and the sublingual location [Figure 4]. Thyroid gland agenesis was suspected and a thyroid profile of the child was done.
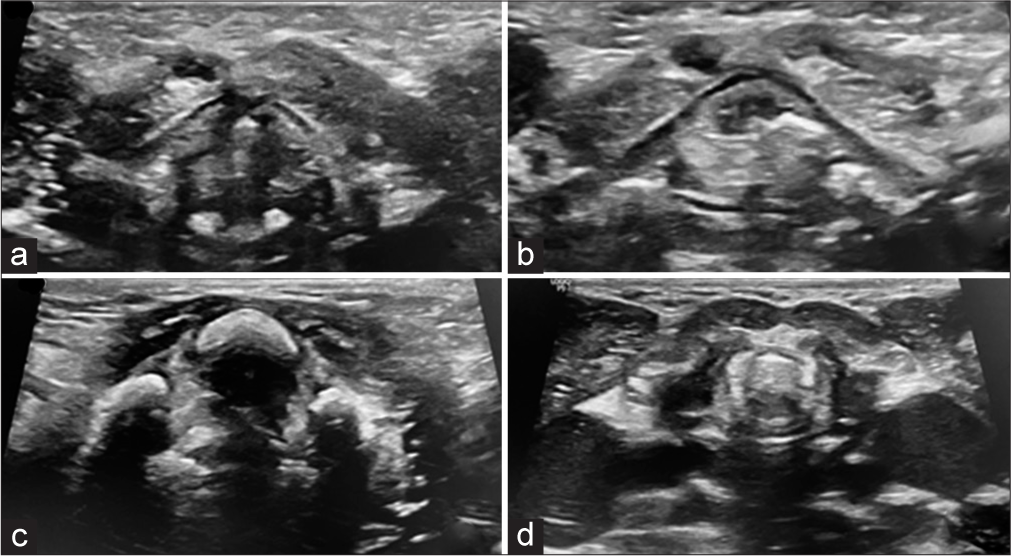
- Ultrasound examination of the neck at the level of the (a) vocal cords, (b) thyroid cartilage, (c) hyoid bone and (d) cricoid cartilage shows absence of the thyroid gland.
The thyroid profile showed T3 and T4 values to be zero. TSH was 100 uIU/mL (normal 0.4–4 uIU/mL). The parathyroid hormone was within normal limits. This confirmed the diagnosis of thyroid agenesis.
The child started treatment with levothyroxine and was on regular follow-up for optimal levels of T3, T4, and TSH. Six weeks after the initiation of treatment, there was a gain in milestones with the child walking with support. Abdominal distension subsided with normal passage of stools. The child became more active and cheerful and also started vocalizing [Figure 1b]. The child is on regular follow-up.
DISCUSSION
Thyroid hormone mediates the growth, development, and maturation of the skeleton by regulating chondrocyte proliferation and promoting differentiation of bone progenitor cells, mineralization, and angiogenesis.[2,3] It also has a permissive role in the action of growth hormone (GH) by promoting GH secretion from the pituitary, as well as GH-dependent insulin-like growth factor 1 (IGF 1) production in the bone.
The paired domain transcription factor PAX8 is expressed in the kidney, thyroid, and many parts of the central nervous system during development. Thyroid hypoplasia is known to be caused by loss of function mutations in the PAX8 gene since PAX8 is essential for TPO production during thyroid development. While thyroid dysgenesis has been induced by the majority of these mutations, some patients with PAX8 mutations have thyroid glands that are normal in size.[4]
When thyroid hormone is absent since birth, it causes short stature with growth arrest and delayed bone age. There is an irregular appearance of the ossification centers leading to a fragmented appearance known as stippled epiphyseal dysgenesis. This is seen predominantly in large cartilaginous centers such as the head of the femur and the head of the humerus.[5] The neck of the femur may be broad and short with a decrease in the neck shaft angle (coxa vara). Acetabulum margins may be irregular. Long bones show a narrowed medullary cavity with a thickened cortex. The spine shows platyspondyly, bullet-shaped vertebral bodies, widened disc spaces, and thoracolumbar kyphosis.[6,7]
In congenital primary hypothyroidism, the skull can be brachycephalic due to enchondral growth retardation at the base of the skull. Intrasutural or Wormian bones can be seen along the coronal or lambdoid sutures. These bones may also be seen in cleidocranial dysplasia, pyknodysostosis, osteogenesis imperfecta, and acro-osteolysis. There can be increased thickness of the bones of the cranial vault with narrowing of the diploic spaces. There is underdevelopment of the paranasal air sinuses with hypoplastic facial bones. The sella is small in young children and larger and rounded in older children due to rebound hypertrophy of the pituitary gland. There is delayed dental development. The poorly developed jaw shows gross dental crowding.[8]
Ultrasound can be used to differentiate thyroid agenesis or dysgenesis from other causes of congenital hypothyroidism in which the thyroid gland has a normal morphologic appearance. It, however, has a lower sensitivity than 99mTc pertechnetate scintigraphy in the detection of sublingual thyroid.
Thus, congenital hypothyroidism causes profound effects on the skeletal system. The radiological features of congenital hypothyroidism should be known especially in children presenting later in life and for differentiating it from other epiphyseal dysplasia or storage disorders. This is especially important in resource-poor countries where screening for congenital hypothyroidism is not routinely done.
Table 1 provides a simplified approach to common skeletal dysplasia and its differentiation from congenital hypothyroidism.[9]
| Common Skeletal Dysplasias | |||||
|---|---|---|---|---|---|
| Congenital hypothyroidism | Mucopolysaccharidosis | Spondyloepiphyseal dysplasia | Achondroplasia | Pseudoachondroplasia | |
| Delayed bone age |
+ | - | - | - | - |
| Platyspondyly | + | + | + | - | + |
| Disc height | Increased | Normal | Reduced | Increased | Increased |
| Abnormality in the spine | Bullet shaped vertebra Thoracolumbar kyphosis |
Anteroinferior beaking→ Hurler syndrome Central beaking→ Morquio’s syndrome |
SED congenita→ Pear-shaped vertebra SED Tarda→ Heaped-up vertebra |
- Bullet-shaped vertebra - Reduced interpedicular distance - Short and thick pedicles |
Central anterior tongue-like projection. |
| Abnormal epiphysis | + | + | + | Abnormal metaphysis only | + |
CONCLUSION
Congenital hypothyroidism should be considered in children with short stature if skeletal survey done to rule out skeletal dysplasia or storage disorders shows significantly delayed bone age.
TEACHING POINTS
Congenital hypothyroidism presenting later in childhood is rare, however possible, especially in resource-poor settings where routine neonatal screening is not done
The radiological features of delayed bone age with other features in the skull, spine, and limbs help differentiate congenital hypothyroidism from other causes presenting with coarse facies and short stature including metabolic and storage disorders and epiphyseal dysplasia
Early initiation of treatment is very essential to prevent permanent neurological and skeletal dysfunction.
MCQs
-
Which of the following is the most common cause of congenital hypothyroidism in underdeveloped countries?
Thyroid agenesis
Thyroid hypoplasia
Iodine deficiency
Thyroid dysplasia
Answer Key: c
-
Which of the following is not a radiographic feature of congenital hypothyroidism?
Proximal pointing of metacarpals
Stippled epiphysis
Persistent large fontanelles
Cortical thickening of long bones
Answer Key: a
-
What effect does thyroid hormone have on the skeleton?
Controlling the growth of chondrocytes and promoting the differentiation of bone precursor cells.
Promotion of GH secretion from the pituitary.
Promotion of the bone production of IGF 1
All of the above
Answer Key: d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Effects of neonatal screening for hypothyroidism. Prevention of mental retardation by treatment before clinical manifestations. Lancet. 1981;2:1095-8.
- [CrossRef] [Google Scholar]
- The effect of hypothyroidism on growth, serum growth hormone, the growth hormone-dependent somatomedin, insulin-like growth factor, and its carrier protein in rats. Endocrinology. 1979;104:1107-11.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid hormone inhibits growth and stimulates terminal differentiation of epiphyseal growth plate chondrocytes. J Bone Miner Res. 1998;13:1398-411.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital hypothyroidism caused by a PAX8 gene mutation manifested as sodium/iodide symporter gene defect. J Thyroid Res. 2010;2010:619013.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal manifestations of juvenile hypothyroidism and the impact of treatment on skeletal system. Indian J Endocrinol Metab. 2013;17:S181-3.
- [CrossRef] [PubMed] [Google Scholar]
- Severe skeletal dysplasia caused by undiagnosed hypothyroidism. Eur J Med Genet. 2007;50:209-15.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic and endocrine disorders affecting bone In: Textbook of radiology and imaging Vol 1. (6th ed). New York: Churchill Livingstone; 1998. p. :241.
- [Google Scholar]
- Abnormal skull X-ray in a child with growth retardation. Postgrad Med J. 1999;75:751-3.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal dysplasias: A radiographic approach and review of common non-lethal skeletal dysplasias. World J Radiol. 2014;6:808-25.
- [CrossRef] [PubMed] [Google Scholar]







