Translate this page into:
Breast cysticercosis mimicking malignancy: A case report from Nepal
*Corresponding author: Anamika Jha, Department of Radiology, Institute of Medicine, Kathmandu, Nepal. dranamikakasyap@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ghimire P, Jha A, Sharma N, Shrestha M. Breast cysticercosis mimicking malignancy: A case report from Nepal. Case Rep Clin Radiol. 2024;2:57-60. doi: 10.25259/CRCR_153_2023
Abstract
Cysticercosis, caused by the larval stage of Taenia solium, is an uncommon parasitic infection typically associated with the central nervous system. Despite its relatively common occurrence in Nepal due to agricultural practices and pig farming, breast involvement in cysticercosis remains an exceptional clinical phenomenon, which we elucidate through a distinctive case report, highlighting the complexities it introduces in diagnosis. A 62-year-old woman presented with a painful lump in her left breast, which raised concerns of malignancy on clinical examination. Mammography and ultrasound further supported this suspicion, revealing an irregular, high-density mass without calcification, and an echogenic rind. To confirm the diagnosis, an ultrasound-guided biopsy was performed, leading to the conclusive identification of cysticercosis through histopathological analysis. This case underscores the importance of considering cysticercosis as a potential diagnosis for solitary soft-tissue lesions, even in regions with a high prevalence of breast cancer. While imaging findings can provide valuable hints, histopathological examination remains the definitive confirmation method. A multidisciplinary approach is crucial, involving clinical, radiological, and histopathological assessments to accurately diagnose and manage such cases. Raising awareness of atypical presentations of cysticercosis is essential for prompt and effective treatment, ultimately leading to improved patient outcomes.
Keywords
Cysticercosis
Breast mass
Larva
INTRODUCTION
Cysticercosis is a parasitic infection caused by the larval stage of Taenia solium, commonly known as pork tapeworm. Although cysticercosis most commonly affects the central nervous system, it can also manifest in extra-neural tissues, leading to a wide range of clinical presentations. While cysticercosis is prevalent in many regions worldwide, including Nepal, cases involving the breast are uncommon.[1] With its population heavily reliant on agriculture and livestock farming, the risk of cysticercosis infections in Nepal is relatively high.[2]
Breast cancer is the second most common cancer in females in Nepal, after cervical cancer.[3] Due to its high prevalence, new breast mass, especially in older women is often considered to be malignant, until proven otherwise. This case report presents an interesting case where a new breast mass in an elderly woman was ultimately diagnosed as cysticercosis, rather than cancer.
CASE REPORT
A 62-year-old female presented with a painful lump in her medial left breast for the last 2 weeks. The patient had no other significant personal, medical, or surgical history. There was no family history of breast or any other cancer. On clinical examination, a mass measuring approximately 3 × 2 cm was palpated in the medial left breast. The mass appeared fixed to the underlying muscle. The diagnostic mammogram revealed an irregularly shaped high-density mass without calcification at the 9 o’clock position in the posterior third of the left breast, about 8 cm from the nipple [Figure 1]. Subsequent ultrasound evaluation showed an irregular hypoechoic mass with indistinct margins, no posterior acoustic features, internal calcifications, or vascularity [Figure 2]. Notably, the mass had an echogenic rind, an echogenic focus within, and was involved in the underlying pectoralis muscles. The ultrasound findings further raised the suspicion of a neoplasm.
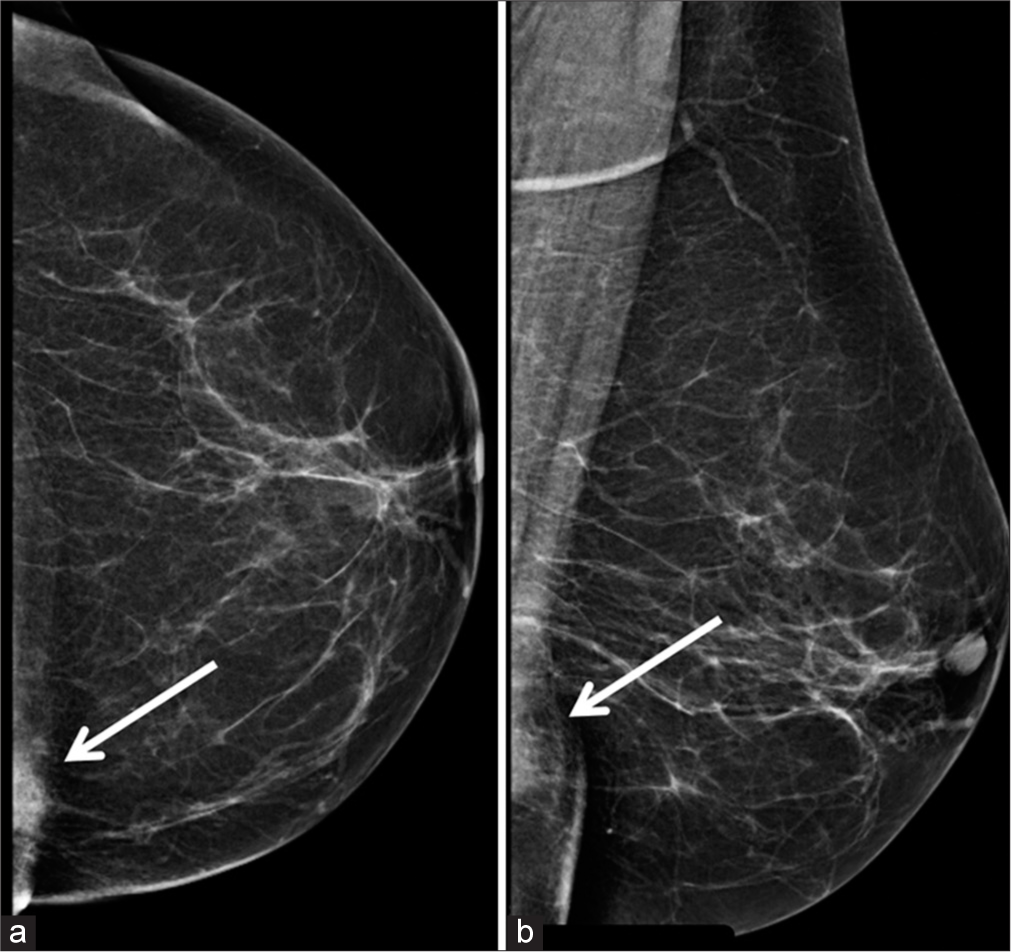
- A 62-year-old woman with breast cysticercosis presented with a painful breast mass. (a) Craniocaudal, and (b) mediolateral oblique view of the left breast shows an irregularly shaped high-density mass without calcification at 9 o’clock position in the posterior third of the left breast (shown by the white arrows in a and b).

- A 62-year-old woman with breast cysticercosis presented with a painful breast mass. A grayscale ultrasound of the left breast mass at 9 o’clock, 5 cm from the nipple shows an irregular hypoechoic mass with indistinct margins (shown by the white arrow), no posterior acoustic features, or vascularity.
An ultrasound-guided biopsy of the mass was performed. The biopsy showed an edematous, myxoid matrix surrounded by an eosinophilic, ciliated, and undulated membrane. In addition, the adjacent area exhibited granulomatous tissue, accompanied by multinucleated giant cells [Figure 3]. These observations conclusively confirmed the diagnosis of cysticercosis. The patient was managed with excision of the mass followed by antiparasitic medication and she recovered well.
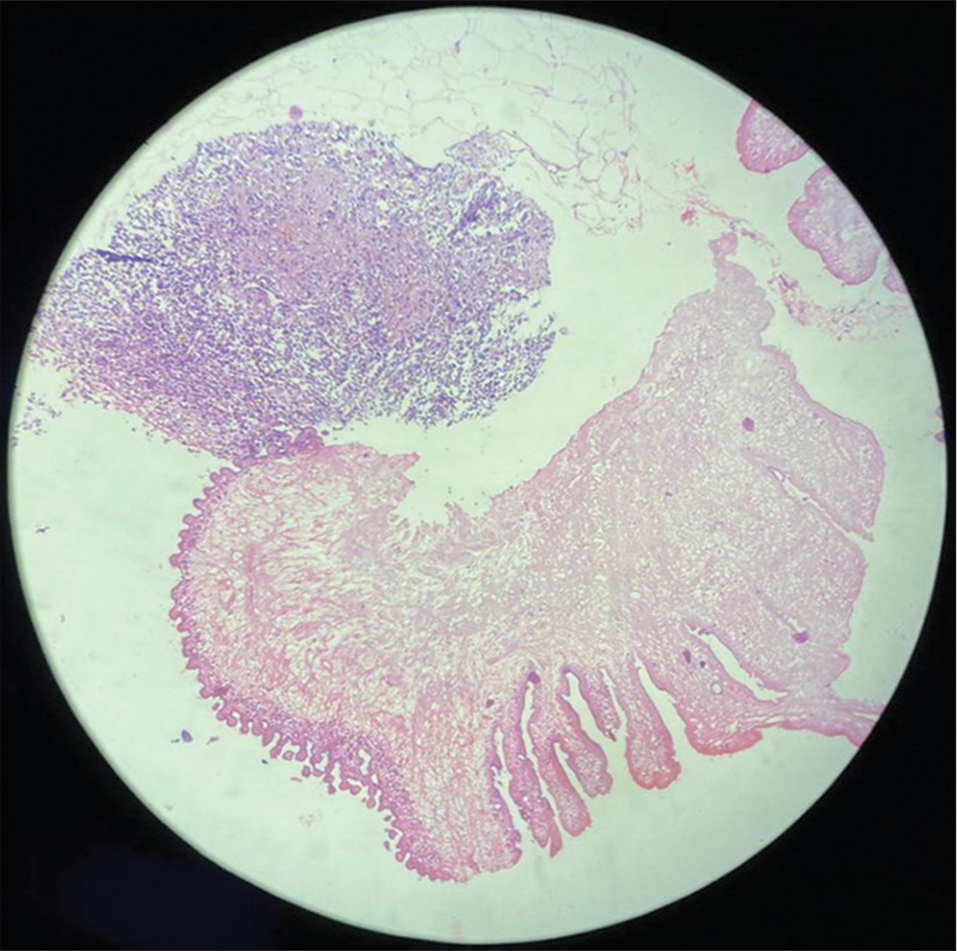
- A 62-year-old woman with breast cysticercosis presented with a painful breast mass. Histopathological image revealing a parasite with irregularly shaped membranous folding and an adjacent area showing a granulomatous reaction.
DISCUSSION
Cysticercosis usually involves the central nervous system, ocular, muscular, and subcutaneous tissues.[1] Only a few case reports and a series of breast cysticercosis have been reported. This report presents an interesting case of breast cysticercosis in Nepal.
The tapeworm lifecycle begins with humans ingesting raw or undercooked pork with Tinea larvae in cysts. Larvae become adult tapeworms in the human gut, releasing eggs in the stool. Pigs consuming these eggs develop cysts in muscles, completing the cycle. Ingesting contaminated food, water, or touching surfaces and mouth can lead to soft tissue cysticercosis in humans. Poor hygiene increases the risk for those living with infected individuals.[4] Cysticercosis occurs worldwide, more prevalent where pig cysticercosis is common. Developing countries with inadequate sanitation have higher frequencies. In Nepal, small-scale pig farming by lower socioeconomic classes facilitates transmission to humans.[5]
The high prevalence of breast cancer and the relatively low occurrence of breast cysticercosis can present a diagnostic challenge for making a provisional diagnosis of cysticercosis. Our patient’s age, and presentation with a new mass which was fixed to the underlying muscle on clinical examination raised suspicion for it being malignant. Imaging findings such as irregular shape on mammogram, and indistinct margins with echogenic rind on ultrasound further pointed toward malignancy. The most common sonography findings of soft-tissue cysticercosis is a cyst with a nodule (scolex), followed by a cyst without a scolex.[6] Surrounding inflammatory reactions can lead to edema or abscess. Solitary soft-tissue cysticercosis lesion is more common than multiple lesions.[7] In our solitary breast lesion, the absence of cyst and scolex added to the diagnostic dilemma, which prompted a biopsy. Retrospectively, the intramuscular location and the echogenic rind due to inflammation are also consistent with cysticercosis. This would, however, not have averted biopsy which would be needed to confirm diagnosis.
Histopathological analysis remains the gold standard for confirming the diagnosis of soft-tissue cysticercosis which provides definitive evidence of cysticercosis.[8] The management of cysticercosis in soft tissue includes antiparasitic medications and surgical excision for symptomatic cases or when the cysts are of significant size.[8-10]
CONCLUSION
The intramuscular location and the echogenic rind due to inflammation are consistent with cysticercosis in our patient. The presence of a cystic lesion with an echogenic dot suggesting scolex may suggest cysticercosis. This would, however, not avert pathological diagnosis which would be needed to confirm diagnosis.
TEACHING POINTS
In regions where cysticercosis is prevalent, health-care providers should include breast cysticercosis as a potential differential diagnosis when evaluating breast carcinoma.
When assessing breast lesions, particularly those located within the muscle tissue, the presence of an echogenic rind caused by inflammation and the detection of an echogenic dot resembling scolex are indicative signs that may lead to a diagnosis of breast cysticercosis.
MCQs
-
What is the definitive host of Taenia solium?
Pigs
Cattle
Human
Dogs
Answer Key: c
-
What is the appropriate next step in a 60-year-old woman with a mass on a mammogram?
Sonography
Fine needle aspiration cytology
Core needle biopsy
CE-MRI breasts
Answer Key: a
-
A cystic breast mass with the central echogenic area, peripheral echogenicity, and no vascularity is best categorized into which of the following breast imaging reporting and data system (BIRADS) categories?
BIRADS 2
BIRADS 3
BIRADS 4
BIRADS 5
Answer Key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cysticercosis in Nepal: A histopathologic study of sixty-two cases. Am J Surg Pathol. 1999;23:1276-9.
- [CrossRef] [PubMed] [Google Scholar]
- Socio-economic and health costs of porcine/human cysticercosis, neurocysticercosis and epilepsy to small-scale pig producers in Tanzania. Bull Natl Res Cent. 2021;45:217.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant neoplasm burden in Nepal-data from the seven major cancer service hospitals for 2012. Asian Pac J Cancer Prev. 2015;16:8659-63.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of taeniasis, cysticercosis and trichinellosis in Vietnam. Parasit Vectors. 2017;10:150.
- [CrossRef] [PubMed] [Google Scholar]
- Human cysticercosis and Indian scenario: A review. J Biosci. 2008;33:571-82.
- [CrossRef] [PubMed] [Google Scholar]
- Soft tissue cysticercosis-Ultrasonographic spectrum of the disease. Indian J Radiol Imaging. 2011;21:60-2.
- [CrossRef] [PubMed] [Google Scholar]
- Soft tissue cysticercosis: Study of 21 cases. J Clin Diagn Res. 2012;6:1669-71.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated intramuscular cysticercosis: Clinicopathological features, diagnosis and management-A review. J Clin Orthop Trauma. 2016;7:243-9.
- [CrossRef] [PubMed] [Google Scholar]
- Role of ultrasonography and magnetic resonance imaging in the diagnosis of intramuscular cysticercosis. Skeletal Radiol. 2012;41:1061-6.
- [CrossRef] [PubMed] [Google Scholar]







