Translate this page into:
Unveiling the nerve bumps in Hansen’s arm and forearm
*Corresponding author: Seetharaman Cannane, Department of Radiology, Kovai Medical Center and Hospitals, Coimbatore, Tamil Nadu, India. drcseetharaman@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sugumar R, Gomathy B, Cannane S. Unveiling the nerve bumps in Hansen’s arm and forearm. Case Rep Clin Radiol. doi: 10.25259/CRCR_55_2024
Abstract
Leprosy is a chronic granulomatous disease caused by Mycobacterium leprae. Intraneural abscess is the rare presentation of leprosy, which poses a diagnostic challenge to the clinician as well as the radiologist. Early identification, diagnosis, and treatment are imperative to reduce the disability. We wish to highlight the features of this rare entity in a 14-year-old male child who presented with painless swelling in arm and forearm.
Keywords
Leprosy
Intraneural abscess
Lepra reaction
INTRODUCTION
Leprosy is also called as Hansen’s disease, a non-fatal, slowly progressing chronic infection caused by Mycobacterium leprae. It affects the skin, peripheral nerves, upper respiratory tract mucosa, and eyes, often presenting as hypopigmented patches with loss of sensation and nerve thickening. The eyes and testes are also highly susceptible due to their lower temperatures compared to the core body temperature.[1,2]
CASE REPORT
A 14-year-old male child presented with complaints of painless swelling in medial aspect of the right arm and forearm. He was a known case of tuberculoid (TT) leprosy on multi-drug treatment. The initial work-up showed normal laboratory parameters. No other complaints were reported. The patient was evaluated with magnetic resonance imaging (MRI) of the right upper extremity.
MRI revealed thickening of subcutaneous nerve [Figure 1] with multiple oval-shaped lesions, at least 4 in number, with thin rim of peripheral enhancement and central diffusion restriction, which were seen along the thickened median nerve in subcutaneous plane of arm and proximal forearm. The largest lesion measures 3.3 × 2.7 × 1.4 cm in the arm. The medial cutaneous nerve was thickened and shows increased short tau inversion recovery (STIR) signal intensity and post-contrast enhancement, suggestive of neuritis [Figure 2]. Based on these imaging features, a diagnosis of neuritis with multiple nerve abscesses in the subcutaneous planes of the arm and proximal forearm was made. The patient evaluated further with punch biopsy from the skin. Histopathological examination (HPE) images [Figure 3] revealed features of granulomatous reaction consistent with TT leprosy. The patient was treated with surgical decompression of the abscess.
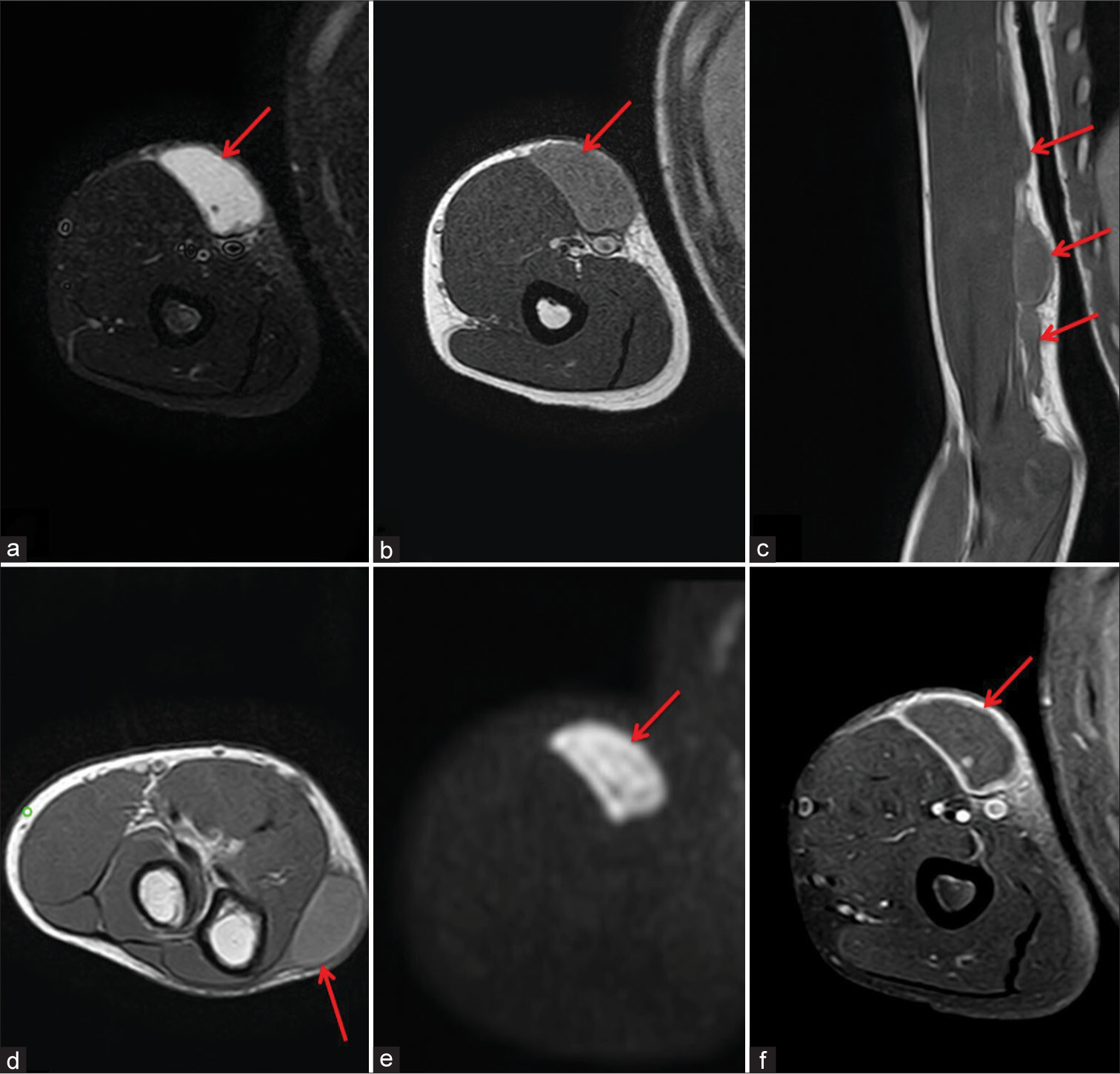
- A 14-year-old male with borderline tuberculoid leprosy who presented with painless swelling in the right upper arm and proximal forearm, magnetic resonance imaging axial short-tau inversion recovery image (a) shows well-defined IR hyperintense mass in the mid arm (red arrow), (b) intermediate signal intensity on T2-weighted (T2W) image (red arrow), and (c) T1-weighted coronal image shows three well-defined lesion along the median nerve (red arrows), (d) T2W image shows similar well-defined lesion in the proximal forearm (red arrow). (e) shows restriction on diffusion-weighted image (red arrow), and (f) shows smooth peripheral enhancement on post contrast fat saturated images (red arrow).
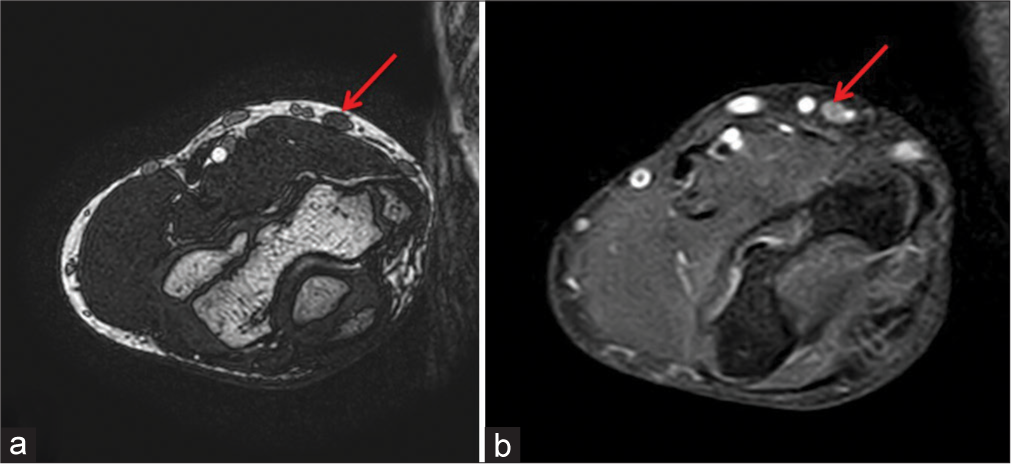
- A 14-year-old male with borderline tuberculoid leprosy who presented with painless swelling in the right upper arm and proximal forearm, magnetic resonance imaging axial T2 space images (a) shows thickened medial cutaneous nerve in arm (red arrow), (b) shows enhancement in T1 post-contrast fat-saturated image (red arrow).
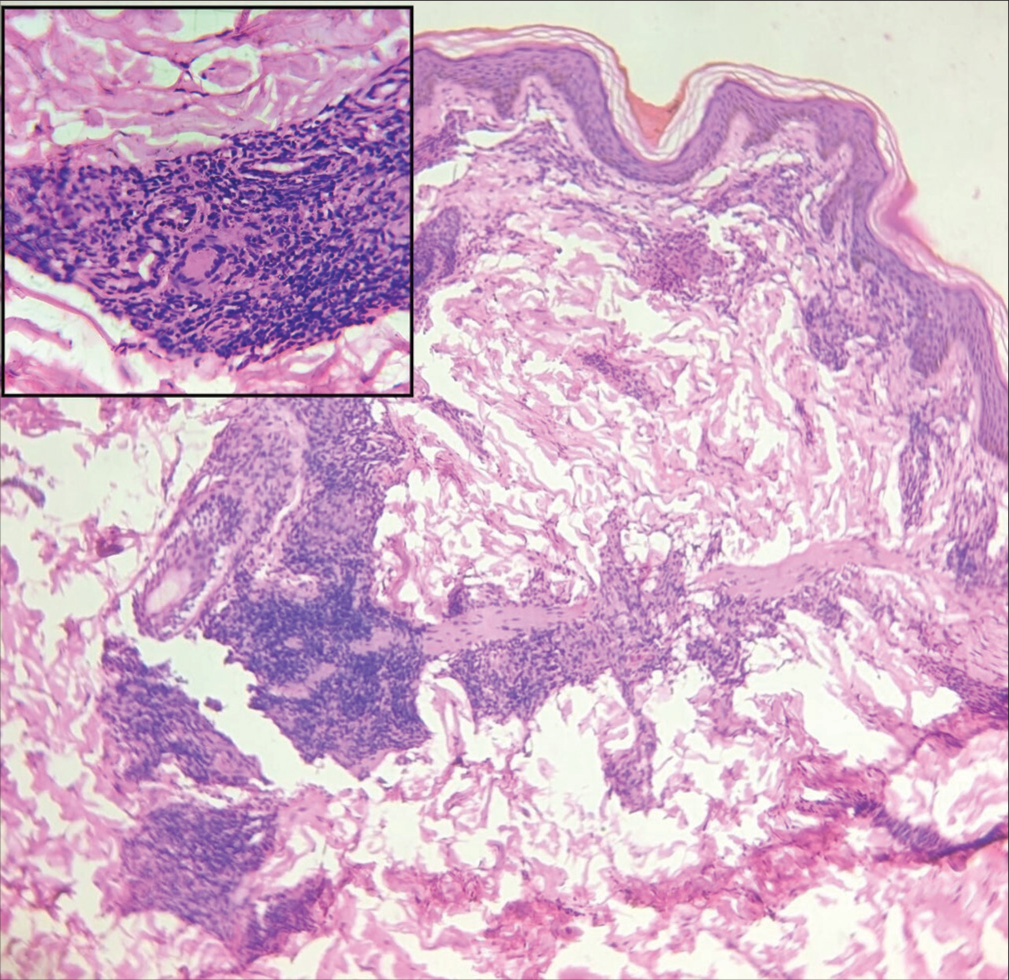
- Histopathology image shows normal epidermis and dermis with multiple granulomas, epitheloid cells, and abundant lymphocytes around the nerves. Inset image (right upper corner) shows granuloma with multinucleate giant cell – Features suggestive of borderline tuberculoid leprosy.
DISCUSSION
Leprosy is a chronic granulomatous disease caused by M. leprae and is characterized by three cardinal features: Hypoesthetic skin lesions, thickened peripheral nerves, and a positive skin smear for Lepra bacilli.[3] This bacterium primarily targets the peripheral nerves, leading to extensive nerve damage. It affects sensory, motor, and autonomic fibers, which can result in a broad spectrum of symptoms, including loss of sensation, muscle weakness, and impaired autonomic functions. As the disease progresses, nerve damage can lead to significant disabilities and deformities, such as clawed hands, foot drops, and facial disfigurement. Based on host immune response Ridley-Jopling classification system classifies leprosy into tuberculoid (TT), borderline tuberculoid (BT), borderline boderline (BB), borderline lepromatous (BL), and lepromatous leprosy (LL).[2,3]
Due to its unique tropism for nerves, patients with all forms of leprosy, especially those with the BT form, may develop nerve abscesses, most commonly affecting the ulnar nerve. The superficial branches of the upper limb nerves are also commonly affected. Typically, the neural lesion is a granuloma; however, it can occasionally form an abscess, particularly in patients with BT leprosy. It is hypothesized that tissue anoxia, resulting from pressure exerted by inflamed and swollen neuronal fascicles, leads to avascular necrosis and subsequent abscess formation.[4,5] Leprosy can also cause eye problems due to involvement of cranial nerves, which result in corneal insensitivity, leading to trauma, infection, corneal ulcers, and blindness. Neuropathy in the extremities leads to insensitivity to touch, pain, and heat, potentially causing the loss of distal digits.[6,7]
BT leprosy is characterized by three to ten skin lesions of varying sizes. Nerve damage is an important characteristic feature of BT leprosy. One of the most striking features of BT leprosy is the type I lepra reaction which is due to increased cell-mediated immunity. Type I lepra reactions cause acute inflammation of existing lesions, resulting in neuritis, ulcers, loss of neurological function, nerve thickening, abscesses, high fever, and can lead to permanent nerve damage, deformity, and disability.[4]
Ultrasonography helps to visualize peripheral nerves and detect more nerve thickening than clinical assessment. It is the preferred initial imaging modality for evaluating peripheral neuropathy because it is cost-effective, accessible, and non-invasive. It is also used to identify the extent of neuropathy and helps in image guided biopsy. The nodular thickening of the ulnar nerve, showing vascularity on color Doppler, is characteristic and represents LL granulomas. Asymmetrical nerve thickening, fascicular abnormalities, and focal or diffuse nerve hypo- or hyperechogenicity are the features of LL involvement of nerve.[4]
MRI is used to evaluate nerve roots and peripheral nerves if ultrasound findings are inconclusive. Affected nerves appear thick, edematous, and show an increased signal on T2-weighted images and short-tau inversion recovery (STIR). Enlargement is usually fusiform and secondary to inflammatory infiltrate, granulomatous reaction, and repetitive microtrauma. In early cases, the fascicular architecture may be intact but as the disease progresses, the nerve fascicles become disrupted, leading to liquefied areas that are bright on T2 and dark on T1 with peripheral enhancement. These microabscesses can merge into larger abscesses, extending beyond the epineurium into nearby soft tissues. MRI shows not only nerve changes but also denervation changes, indicating nerve involvement. STIR hyperintensity in the hand and forearm muscles suggests acute denervation due to the involvement of all three forearm nerves.[2,4,8]
MRI is very good at detecting early nerve-related joint changes in asymptomatic patients. It can spot degradation and interruption of subcutaneous fat, as well as effusion and synovitis in the metatarsophalangeal joints.
Treatment of leprosy usually involves multiple drug therapy to ensure no microbial resistance. Medications used include dapsone, rifampin, and clofazimine are used. The abscess due to reversal reactions can be treated with corticosteroids; however, large nerve abscess requires immediate surgical intervention to prevent irreversible sequelae. During surgical exploration of the ulnar nerve, the primary goals are to drain the pus, remove necrotic tissue, external neurolysis, and decompress the nerve to alleviate pressure. These steps are crucial to minimize long-term damage and restore as much function as possible.
DIFFERENTIALS DIAGNOSIS
The closest differential diagnosis and their salient imaging features are mentioned in Table 1.
| Neurofibroma |
|
| Schwannoma |
|
| IgG4-related disease |
|
| Amyloid neuropathy |
|
CT: Computed tomography, Ig: Immunoglobulin.
CONCLUSION
Leprosy remains the most common preventable neuropathy in endemic regions and neuroimaging in Hansen’s disease has unveiled several new insights. Advances in imaging technology, particularly ultrasound and MRI, combined with clinical and pathological correlations, significantly aid in diagnosis and prompt treatment.
TEACHING POINTS
Nerve damage, including nerve abscess formation and skin lesions, is a key characteristic of BT leprosy and type I lepra reactions
Nodular thickening and edematous nerves with abscesses formation on MRI/ultrasound imaging are characteristics of LL involvement.
MCQs
-
Which one of the following sentences is false regarding leprosy?
It is caused by Mycobacterium leprae
Hypoesthetic skin lesions and thickened peripheral nerves are present
Leprosy involves peripheral nerves
Leprosy spares the cranial nerves
Answer Key: d
-
What are the standard modalities for imaging leprosy nerve involvement?
Ultrasound
Tc99m-sestamibi
Computed tomography
MRI
All of the above
Answer Key: b
-
Which one of the following is false regarding peripheral nerve involvement in leprosy?
Neurofibroma is one of the differential diagnoses
Nerve abscess are seen with lepra reactions
Nerve abscess are treated with immediate surgical decompression
Peripheral always associated with skin lesions
Answer Key: d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Insight into the evolution and origin of leprosy bacilli from the genome sequence of Mycobacterium lepromatosis. Proc Natl Acad Sci. 2015;112:4459-64.
- [CrossRef] [PubMed] [Google Scholar]
- Neuroimaging in leprosy: The nerves and beyond. Radiol Infect Dis. 2020;7:12-21.
- [CrossRef] [Google Scholar]
- A case of borderline tuberculoid leprosy with type one lepra reaction. Cureus. 2023;15:e38081.
- [CrossRef] [Google Scholar]
- Ultrasonography and magnetic resonance imaging of ulnar nerve abscess in leprosy. Med J Armed Forces India. 2016;72:78-81.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral corneal perforation caused by neurotrophic keratopathy associated with leprosy: A case report. BMC Ophthalmol. 2022;22:42.
- [CrossRef] [PubMed] [Google Scholar]
- US and MR imaging of peripheral nerves in leprosy. Skeletal Radiol. 2000;29:142-50.
- [CrossRef] [PubMed] [Google Scholar]








