Translate this page into:
Unusual case of mononeuropathy in child: Intraneural perineurioma of sciatic nerve
*Corresponding author: Abhijeet Taori, Department of Radiology, Suyash Hospital, Indore, Madhya Pradesh, India. abhijittaori@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Taori A, Malpani D. Unusual case of mononeuropathy in child: Intraneural perineurioma of sciatic nerve. Case Rep Clin Radiol. 2024;2:8-10. doi: 10.25259/CRCR_21_2023
Abstract
Intraneural perineurioma is a benign nerve sheath tumor of the perineurium characterized by focal perineural cell proliferation. It is primarily seen in young adults. Early childhood presentation is uncommon. We present this interesting case in a child with overall clinical assessment, nerve conduction tests, and magnetic resonance findings in keeping with intraneural perineurioma of the sciatic nerve. It is essential to recognize this potentially treatable disease entity in the early childhood and exclude other causes of nerve palsy.
Keywords
Intraneural perineurioma
Magnetic Resonance Imaging
Child
Pediatrics
INTRODUCTION
Intraneural perineurioma is a benign tumor of the perineurium of nerve sheaths characterized by focal perineural cell proliferation first described in 1964.[1] It presents as a slowly progressive neuropathy with loss of motor function of the affected nerve. Most common age of presentation is in young adults. We present an interesting case presenting with symptoms in the first decade.
CASE REPORT
An 8-year-old boy came to emergency department with a 6 month history of weakness in the left lower foot. He initially noticed symptoms predominantly while playing football which then progressed to abnormal gait. He had no history of recent illness or trauma. An initial neurological exam revealed weak left foot eversion and dorsiflexion of ankle. Ankle plantar flexion, knee, and hip function in both limbs were within normal limits. Deep tendon reflexes and touch sensation were preserved.
Radiographs of both knee and ankle were not significant. A concurrent nerve conduction study suggested a partial left sciatic neuropathy. In view of these findings, further workup on magnetic resonance (MR) examination was thought to be pertinent. Examination was tailored to include lumbosacral trunk, sacral plexus, and the sciatic nerve in the field of view.
MR examination [Figure 1a and b] demonstrated significant fusiform hypertrophy of the left lumbosacral trunk and sciatic nerve appearing hyperintense on short-tau inversion recovery acquisition. The fascicular structure of the nerve was preserved. The bulk of gluteal muscles were mildly decreased. A presumptive diagnosis of intraneural perineurioma predominantly involving sciatic nerve was thus established.
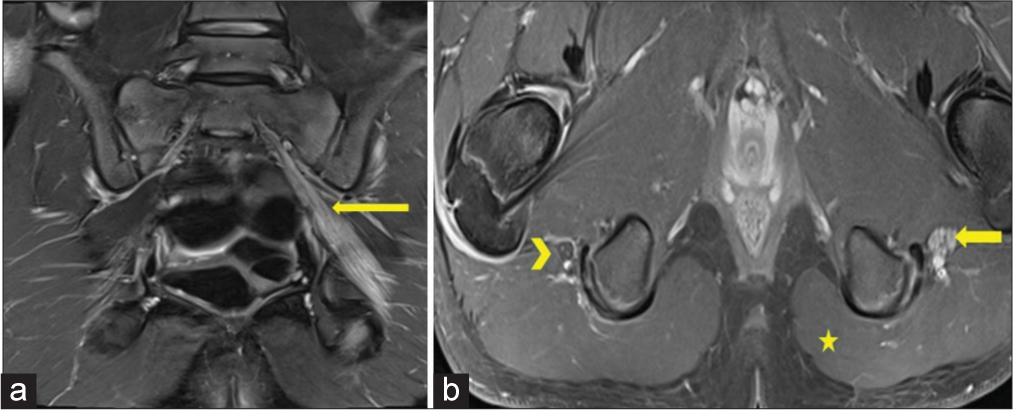
- (a) Coronal short tau inversion recovery (STIR) image including the sciatic notch and thighs. The left sciatic nerve is diffusely enlarged from the sciatic notch to the upper thigh with an increase in signal intensity (arrow). (b) Axial STIR image at the level of the upper thigh. There is a diffuse enlargement of the left sciatic nerve with hypertrophied fascicles (arrow). Contralateral sciatic nerve appears unremarkable (arrowhead). Note mild asymmetry of the gluteal muscles with decreased bulk on left (star).
DISCUSSION
MR plays a valuable important role in the pre-operative assessment and ascertaining the extent of the lesion. There is an equal predilection between the upper and lower extremity, but the sciatic nerve is the most common location overall.[2] The need for confirmatory biopsy is redundant due to a definitive assessment on MR. However, before MR study, it is necessary to exclude other central causes with a thorough clinical assessment and nerve conduction exam. The differential diagnosis for this entity includes other focal neuropathies including schwannoma, inflammatory neuritis, and post-traumatic neuroma [Table 1].
| Schwannoma | Typical magnetic imaging appearance and split fat sign |
| Inflammatory neuritis | Positive lab markers. Multifocal involvement |
| Post-traumatic neuroma | Corroborative history with partial/complete nerve transection |
| Chronic inflammatory demyelinating polyneuropathy | More diffuse or multifocal appearance with involvement of multiple nerves |
The literature on the treatment of intraneural perineurioma is in favor of surgery with uncertainty on the best approach. Probable treatments include resection and nerve graft.[3] Ferraresi et al.[4] advocated use of muscle and tendon transfer in patients with advanced foot drop, wherein long-term recovery of nerve function was unlikely.
CONCLUSION
The best option for potential recovery of function is early identification giving the opportunity to proceed with appropriate treatment. It is essential to recognize and suspect this potentially treatable disease entity in the early childhood and exclude other causes of nerve palsy.
TEACHING POINTS
It is essential to recognize and suspect intraneural perineurioma disease as distinct entity causing symptoms leading to nerve palsy as it is treatable with the early diagnosis.
The best option for potential recovery of function is early identification giving the opportunity to proceed with appropriate treatment.
MCQs
-
What is usual presentation of intraneural perineurioma?
Gradual onset and slow progression of motor loss
Gradual onset and slow progression of sensory loss
Gradual onset and slow progression of motor and sensory loss
Rapidly progressive of motor and sensory loss
Answer Key: a
-
Following investigations are prudent in evaluation of focal nerve palsy, except?
USG
Radiographs
MR
EMG/NCV
Answer Key: b
-
Treatment options of intraneural perineurioma include all except?
Resection
Resection and nerve graft
Muscle and tendon transfer
Amputation
Answer Key: d
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Monosymptomatic interstitial hypertrophic neuritis. J Neurol Sci. 1964;1:340-7.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral tumor and tumor-like neurogenic lesions. Eur J Radiol. 2013;82:38-50.
- [CrossRef] [PubMed] [Google Scholar]
- Resection and graft repair for localized hypertrophic neuropathy. Neurosurgery. 1998;43:78-83.
- [CrossRef] [PubMed] [Google Scholar]
- Perineurioma of the sciatic nerve: A possible cause of idiopathic foot drop in children: Report of 4 cases. J Neurosurg Pediatr. 2010;6:506-10.
- [CrossRef] [PubMed] [Google Scholar]







