Translate this page into:
Unilateral facial asymmetry: Do not forget to look at the subcutaneous tissue
*Corresponding author: Vandana Yadav, Departments of Radiodiagnosis and Imaging, Institute of Medical Sciences, Banaras Hindu University (BHU), Varanasi, Uttar Pradesh, India. vandana.ydv@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadav V, Kumar I, Yadav N, Aggarwal P, Verma A. Unilateral facial asymmetry: Do not forget to look at the subcutaneous tissue. Case Rep Clin Radiol. doi: 10.25259/CRCR_171_2023
Abstract
Parry–Romberg syndrome is a rare cause of hemifacial atrophy with associated other systemic complaints including neurological symptoms. Diagnosis is based on history and clinical examination supported by imaging. Here, we report a case of a 10-year-old female presenting with gradually progressive left hemifacial atrophy for 2 years and describe the clinical and imaging findings of the patient.
Keywords
Parry–Romberg syndrome
Unilateral facial atrophy
Progressive hemifacial atrophy
Magnetic resonance imaging
INTRODUCTION
Parry-Romberg syndrome is a rare disease with unknown etiology and thought to be of sporadic origin. The disease is more common in females. Diagnosis is primarly based on history and clinical examination supported by imaging. The management is predominantly symptomatic.
CASE REPORT
A 10-year-old girl presented with gradually progressive left hemifacial atrophy over the past 2 years. A focal area of bony depression and focal alopecia at the left parietal region is seen. There is no history of focal neurological deficit or vision abnormality. There is no history of headache, facial paresthesia, or seizures. On physical examination, the left side of the face showed gross atrophy [Figure 1a]. Palpable depression of the left parietal skull bone was noted. Focal alopecia was noted [Figure 1b]. Central nervous system examination was normal.

- (a) Photograph demonstrates assymetric atrophy of subcutaneous tissue on the left side of face. (b) Focal alopecia over the left parietal region.
3D reconstructed computed tomography (CT) shows asymmetric thinning of the left parietal bone [Figure 2]. Magnetic resonance imaging (MRI) of the face reveals asymmetric scalp thickness and relatively reduced subcutaneous fat on the left side [Figure 3a and b]. There is atrophy of masticator group of muscles and muscles of face on the left side [Figure 3c]. The left lentiform nucleus demonstrates an abnormal hyperintense punctate focus on T2/fluid-attenuated inversion recovery (FLAIR) images [Figure 3d].
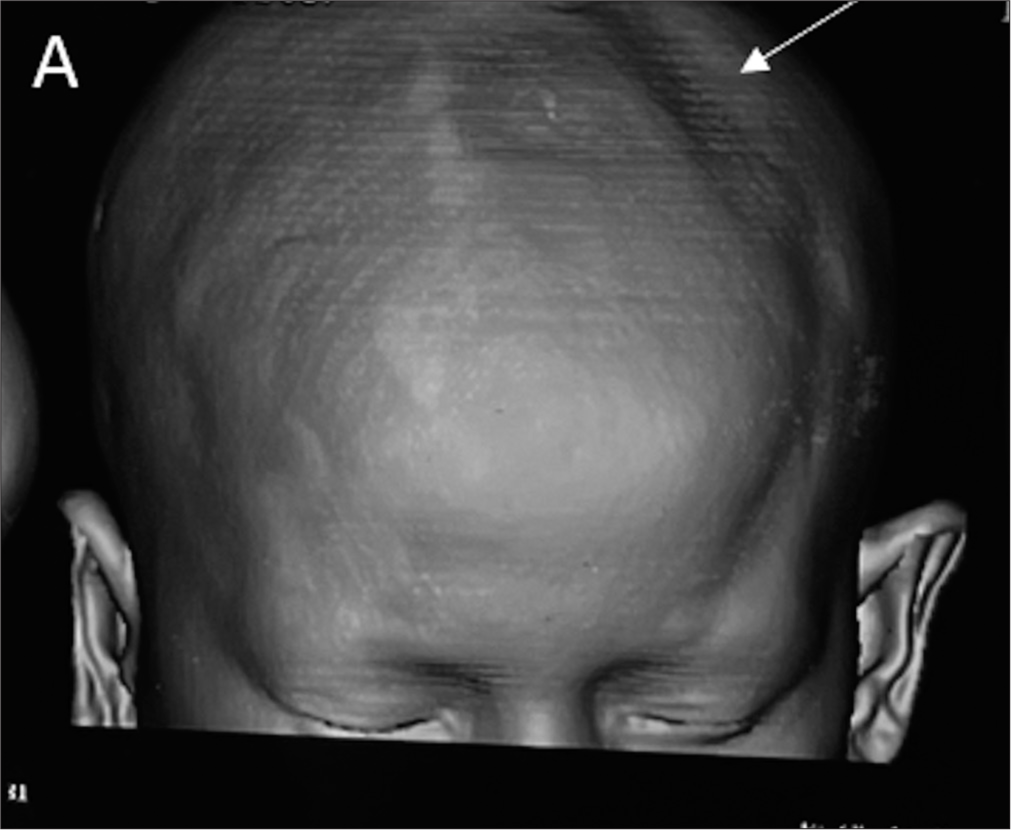
- 3D reconstructed computed tomography shows asymmetric thinning of left parietal bone (white arrow).
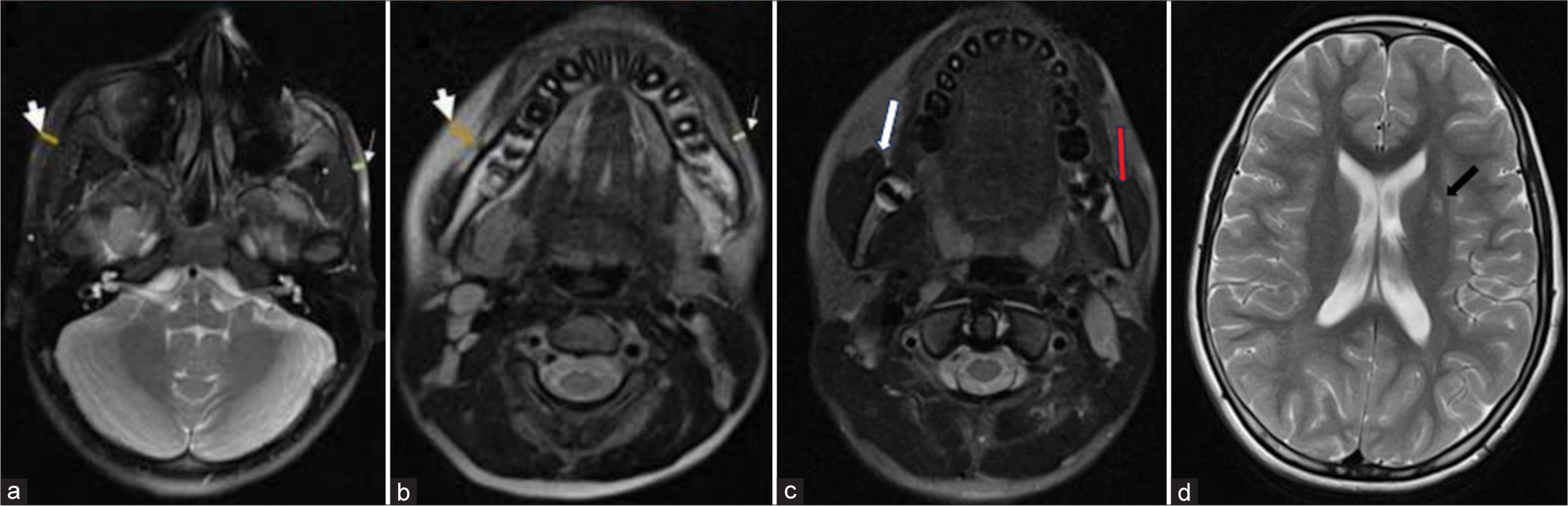
- (a and b) Magnetic resonance imaging of brain showing asymmetric atrophy of skin and subcutaneous tissue on left side (thin arrows) as compared to that on the right side (thick arrows); (c) atrophy of masticator group of muscles on left side (red arrow) as compared to that on right side (white arrow); (d) abnormal T2 hyperintense foci in left lentiform nucleus (black arrow).
DISCUSSION
Parry–Romberg syndrome (PRS), also called progressive hemifacial atrophy is a rare, gradually progressive condition that tends to resolve spontaneously. It is more prevalent in females.[1] It presents as hemifacial atrophy, with variable age of presentation and variable progression of disease, ranging from 2 to 20 years, and stabilizing with no discernible reason.[1,2]
The underlying mechanism of disease is unknown, and various theories have been proposed encompassing factors such as trauma, heredity, developmental, exposure to radiation, infection, dysfunction of sympathetic cervical ganglion, endocrine and metabolic disturbances, and inflammatory autoimmune disorder associated with or without vasculopathy.[3]
Clinically, it presents as hemifacial atrophy, neurological complications (including facial paresthesia, severe headache, trigeminal neuritis, and seizures), and can also have pathologies related to hair (including depigmentation and alopecia) as seen in our case, symptoms related to eyes (such as uveitis, globe retraction, enophthalmos, heterochromia, and vision problems). Dental and jaw-related issues can also be presented.[3]
Diagnosis is established on the basis of history and examination, further supported by imaging studies.[3,4] Radiologically, the findings of hemifacial atrophy are well seen with either CT or MRI of the face. Findings include as follows:[1,3]
Atrophy of bone, soft tissue, or muscles
Non-specific T2/FLAIR white matter hyperintensity
Leptomeningeal enhancement
Intracranial calcifications
Brain atrophy.
Differential includes as follows:
Linear scleroderma en coup de sabre (variant of localized scleroderma) - presence of myositis/myopathy and unilateral limb atrophy on the same side of facial atrophy is seen in linear scleroderma which is not seen in PRS. Atrophy of underlying bone is usually not seen in linear scleroderma[5]
Rasmussen encephalitis - it involves unilateral atrophy of brain parenchyma with no skin lesion or atrophy of subcutaneous tissue/muscles/bone[5]
Sturge–Weber syndrome - diagnosis is usually clear because of congenital port-wine stain. Differential of PRS is considered in approximately 5% cases of Sturge–Weber syndrome where cutaneous involvement is absent; however, facial atrophy is still not present in such cases of Sturge–Weber syndrome and intracranial imaging features of subcortical calcification, ipsilateral parenchymal loss, rules out PRS[5]
Goldenhar syndrome - is a syndromic congenital disease with ear, ocular, and vertebral anomalies. When present with hemifacial atrophy, differential of PRS should be considered
Hemifacial microsomia (first and second branchial arch syndrome) - it is a congenital non-progressive condition causing hypoplasia of mandible, temporomandibular joint, external ear malformation, and absent/hypoplastic zygoma. Common features of PRS are hypoplasia of facial muscles and adjacent soft tissues. Extracranial anomalies of skeletal, lung, kidney, and gastrointestinal symptoms may be seen
Hemifacial hyperplasia also leads to facial asymmetry due to overgrowth rather than atrophy
Partial lipodystrophy also known as Barraquer–Simons syndrome may present as PRS, but typically these manifestations are bilateral.[1,3]
No curative therapy for the disease has been identified. Treatment primarily focuses on symptomatic management, such as migraine pain relief, anti-seizure drugs, immunosuppressant therapies, and steroids. After disease stabilization, cosmetic therapies for aesthetics can be done, which include muscle flap or fat flap grafts, silicone injections, and bone augmentations.[1,3]
DIFFERENTIAL DIAGNOSIS
Linear scleroderma
Rasmussen encephalitis
Sturge–Weber syndrome
Goldenhar syndrome
Hemifacial microsomia
Hemifacial hyperplasia
Barraquer–Simons syndrome
CONCLUSION
Parry Romberg Syndrome is a disfiguring disease with other systemic complaints. Diagnosis is established on the basis of history and examination, further supported by imaging studies. No curative therapy for the disease has been identified.
TEACHING POINTS
Careful scrutiny of subcutaneous fat should be done on MRI in cases of unilateral facial asymmetry.
Parry–Romberg syndrome can be associated with various intracranial and extracranial focal lesions identifiable on MRI.
MCQs
-
Which one of the following is not a cause of hemifacial atrophy?
Linear scleroderma
Parry–Romberg syndrome
Goldenhar syndrome
Congenital hemihyperplasia
Answer Key: d
-
Which one of the following is not a clinical feature of Parry–Romberg Syndrome?
Exophthalmos
Facial atrophy
Optic neuropathy
Dystonia
Answer Key: a
-
Intracranial radiological changes in patient of Parry– Romberg syndrome are all except
Cerebral microhemorrhages
Intracranial aneurysm
Grey matter heterotopia
Leptomeningeal enhancement
Answer Key: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Parry Romberg syndrome: 7 cases and literature review. Am J Neuroradiol. 2015;36:1355-61.
- [CrossRef] [PubMed] [Google Scholar]
- Parry-Romberg syndrome: Intracranial MRI appearances. J Craniomaxillofac Surg. 2003;31:321-4.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and radiologic findings in progressive facial hemiatrophy (Parry-Romberg syndrome) AJNR Am J Neuroradiol. 1997;18:751-7.
- [Google Scholar]
- Parry Romberg syndrome with localized scleroderma: A case report. J Clin Exp Dent. 2014;6:e313-6.
- [CrossRef] [PubMed] [Google Scholar]







