Translate this page into:
Role of imaging in atypical infantile lipofibromatosis
*Corresponding author: Mrinal Matish, Department of Radiodiagnosis, All India Institute of Medical Sciences, Patna, Bihar, India. drmrinalmatish@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Matish M, Kumar P, Bhartiya R, Jana S. Role of imaging in atypical infantile lipofibromatosis. Case Rep Clin Radiol. 2025;3:63-6. doi: 10.25259/CRCR_162_2023
Abstract
Lipofibromatosis is an extremely rare, hamartomatous soft-tissue tumor seen almost exclusively in the pediatric age group. They are typically found in the extremities. Varied clinical presentations and lack of specificity in imaging findings often create a diagnostic dilemma. A systematic approach with emphasis on tumor composition is needed to arrive at a correct diagnosis. We report an unusual case of a giant lipofibromatosis that presented as a painless progressive back swelling in a 10-month-old male infant.
Keywords
Lipofibromatosis
Chemical shift imaging
Fibrofatty tumor
INTRODUCTION
Lipofibromatosis is a sporadic, benign, fibrofatty soft-tissue tumor that recently gained recognition as a distinct entity.[1] It is classically found in the distal extremities and pediatric population with a male predominance.[1,2] Imaging plays a crucial role in the detection and characterization of such lesions. This case report focuses on the radiological features and enumerates the imaging differentials of pediatric fibrofatty tumors.
CASE REPORT
A 10-month-old male infant presented with a painless swelling in the upper back region since birth. The swelling was initially a coin-sized flat lesion at birth and then slowly progressed to reach the present size. On physical examination, it was firm, immobile, and non-tender.
Ultrasound showed a large (15 × 8 cm), well-defined, avascular, heterogeneously hypoechoic lesion with interspersed radiating hyperechoic strands involving the subcutaneous and intermuscular plane of the upper back region [Figure 1a and b].
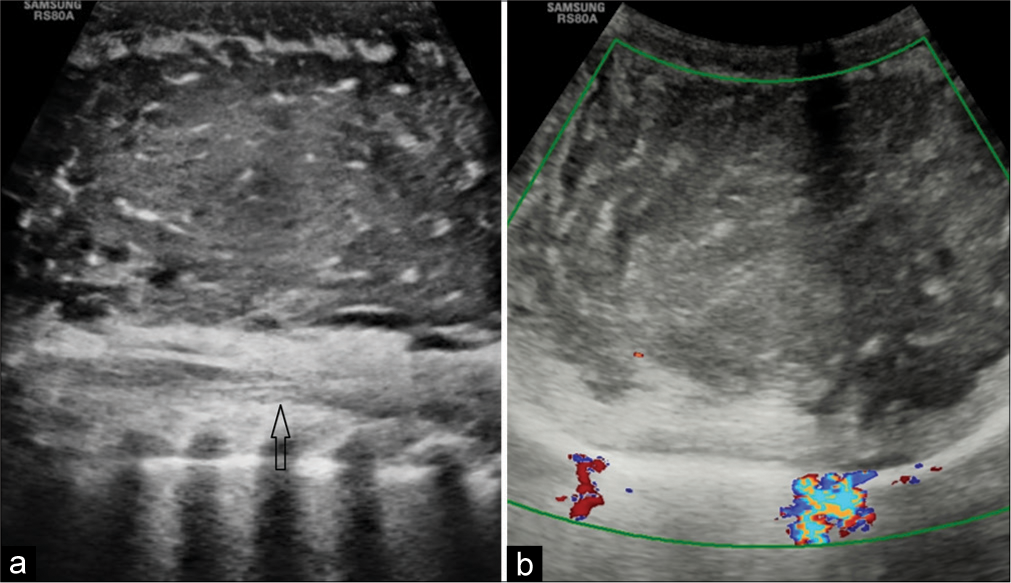
- (a) Longitudinal B-mode ultrasound image showing heterogeneously hypoechoic mass with radiating hyperechoic strands. The mass is seen separately from the underlying spinal canal (black arrow). (b) Transverse color Doppler image showing no significant vascularity of the lesion.
Magnetic resonance imaging (MRI) with contrast was done for further characterization of the lesion. It appeared hypointense on T1-weighted (T1w) and T2-weighted (T2w) images with substantial homogenous post-contrast enhancement [Figure 2]. On in-phase images, there were a few tiny T1 and T2 hyperintense foci scattered within the lesion, which showed a loss of signal on out-of-phase images suggestive of microscopic fat [Figure 3]. There was no evidence of infiltration into the adjacent tissues or communication with the underlying spinal canal.
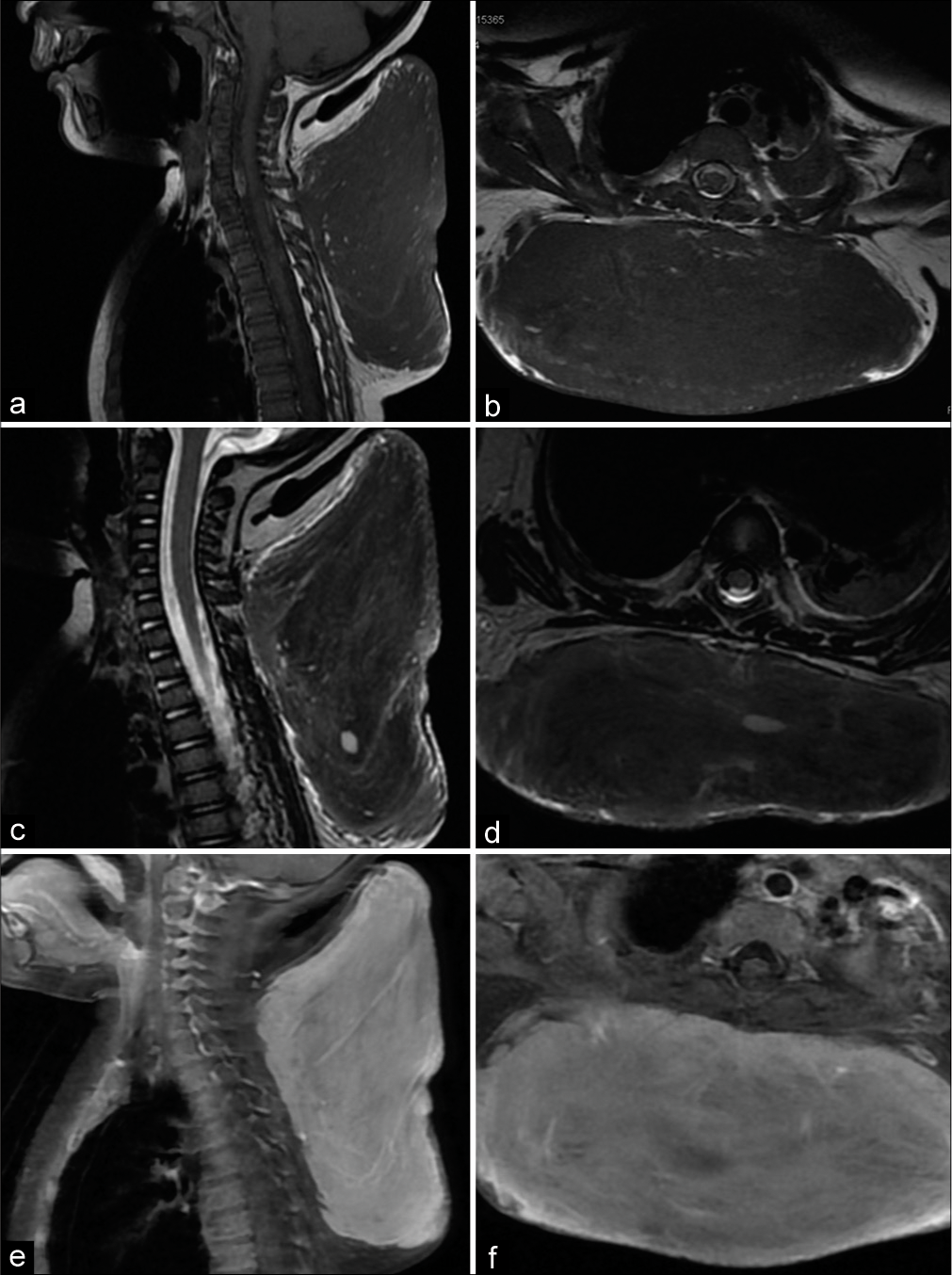
- (a) Sagittal T1w, (b) axial T1w, (c) sagittal T2w, (d) axial T2w images showing the diffuse hypointense signal intensity of the lesion on both T1w and T2w images. (e and f) Sagittal and Axial Gadolinium-enhanced T1 Fat saturated (FS) images showing substantial homogeneous enhancement of the lesion.
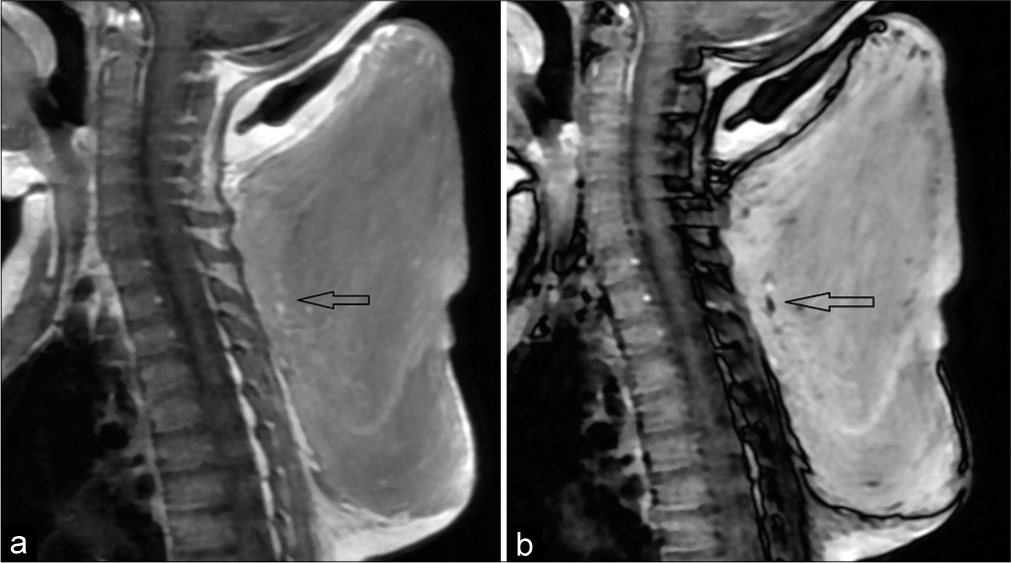
- (a) Chemical shift in phase image shows a few scattered hyperintense foci within the lesion (black arrow). (b) Corresponding loss of signal (black arrow) in opposed phase image suggestive of microscopic fat.
The patient subsequently underwent an excision biopsy of the mass under general anesthesia. The excised mass was reddish-yellow with a firm consistency [Figure 4]. Histopathological examination revealed haphazardly arranged spindle cells with oval to elongated nuclei and bland chromatin along with interspersed mature adipose tissue. The final diagnosis of a spindle cell neoplasm favoring lipofibromatosis was made. The patient was discharged and follow-up was advised.
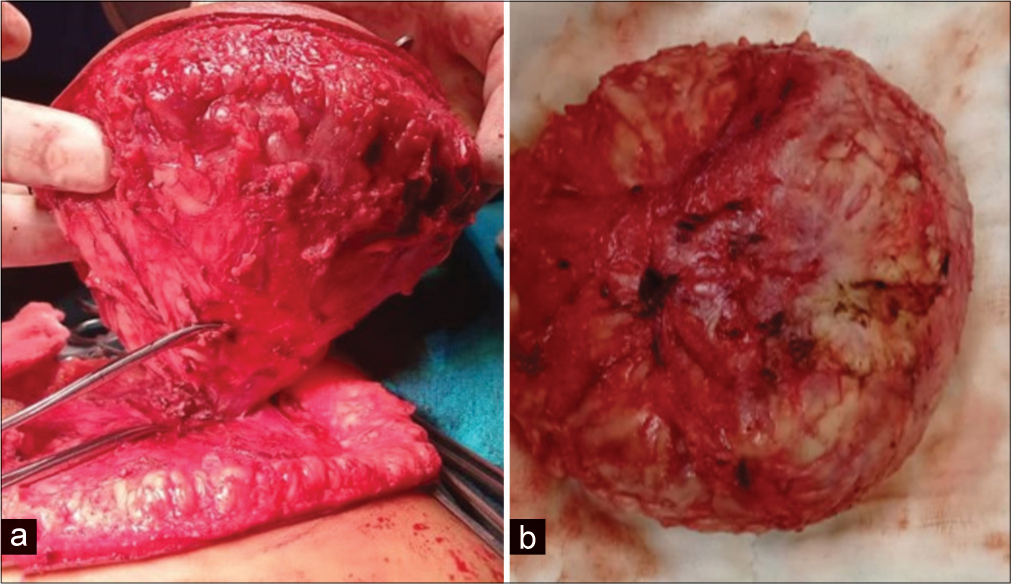
- (a) Post-operative excised specimen showing reddish yellow tumor with no capsule. (b) Yellowish fatty component within the excised specimen suggestive of fat.
DISCUSSION
Lipofibromatosis is clinically characterized by a painless mass with indistinct borders. It has a predilection for the extremities, usually found under the skin and/or involving deep soft tissues of the hand or foot. Entrapment of vessels, nerves, and muscles is common, but significant functional impairment has not been associated with these tumors.[3] The etiology of this congenital neoplasm is uncertain. The age of onset ranges from 1 to 14 years. Most tumors are approximately 1–7 cm in diameter, with a mean diameter of approximately 2 cm.[1] Tumors exceeding 5 cm in diameter are rare.[4]
Most published case reports of lipofibromatosis to date have shown a predominantly lipomatous tumor (appearing heterogeneously hyperintense on T1w and T2w images) with relatively minor fibrous components.[5-7] However, in our case, the mass showed scanty fatty components and primarily fibrous tissue composition, resulting in MRI appearance of hypointensity on T1w and T2w images and homogenous enhancement on post-contrast images. Moreover, the truncal location of the tumor and size <10 cm makes it unique.
Because of the lesion’s predominant fibrous nature, the differential diagnoses in our case included infantile fibrosarcoma, calcifying aponeurotic fibroma, fibrous hamartoma of infancy, and inflammatory myofibroblastic tumor. On ultrasound, rhabdomyosarcoma was a potential differential diagnosis; however, MRI images revealed no evidence of infiltration or edema of the surrounding structures, and the presence of microscopic fat within the lesion allowed us to rule it out.
Ultrasonography is not very sensitive in the identification of fat due to the variable appearance of adipose tissue. In contrast, MRI is highly sensitive for the detection of fatty tissue and the macroscopic fat appears as hyper-intense on T1w and T2w images with signal suppression on fat-suppressed or short tau inversion recovery images.
Chemical shift imaging (CSI) is a valuable tool for the identification of microscopic fat as shown in our case. Loss of signal intensity between the in-phase and opposed-phase MR images indicates intravoxel lipid, thus aiding in the definitive benign diagnosis.[8]
The preferred course of treatment for pediatric fibrous tumors is complete surgical resection with the preservation of neurovascular structures. These tumors can grow quite large if untreated and have a high rate of local recurrence if only partially excised.[7]
DIFFERENTIAL DIAGNOSIS
Infantile fibrosarcoma
Calcifying aponeurotic fibroma
Fibrous hamartoma of infancy
Inflammatory myofibroblastic tumor
CONCLUSION
Pediatric soft-tissue tumors have diverse clinical and radiological presentations. A systematic approach with emphasis on tumor composition is needed for accurate diagnosis. Identifying fat within the lesion suggests benign etiology. We recommend that CSI should be included in the MRI protocol of every pediatric soft-tissue tumor case. Definitive diagnosis usually will require a pathology work-up.
TEACHING POINTS
Lipofibromatosis is a benign, painless, slow-growing lesion seen in the pediatric age group, typically located in the extremities but can be present in atypical locations
When dealing with pediatric soft-tissue tumors, emphasis on tumor composition should be given as identifying fibrous or fatty or soft-tissue components within the lesion help in narrowing down the differential diagnosis and additional sequences such as CSI should be included in the MRI protocol.
MCQs
-
MRI findings of a patient with a slow-growing lump in the dorsum of the foot show an ill-defined mass, appearing hyperintense on T1w and T2w images with multifocal scattered hypointense contents within. Which among the following is the most possible diagnosis?
Lipoma
Liposarcoma
Lipofibromatosis
Rhabdomyosarcoma
Answer Key: c
-
Which among the following are differential diagnoses of fibrofatty tumors?
Infantile fibrosarcoma
Calcifying aponeurotic fibroma
Fibrous hamartoma of infancy
All of the above
Answer Key: d
-
Which of the modalities may offer the most information in the assessment and management of pediatric soft-tissue tumor?
X-ray
Ultrasound
CT
MRI
Answer Key: d
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A clinicopathologic study of 45 pediatric soft tissue tumors with an admixture of adipose tissue and fibroblastic elements, and a proposal for classification as lipofibromatosis. Am J Surg Pathol. 2000;24:1491-500.
- [CrossRef] [PubMed] [Google Scholar]
- WHO classification of soft tissue tumours: An update based on the 2013 (4th) edition. Pathology. 2014;46:95-104.
- [CrossRef] [PubMed] [Google Scholar]
- Aberrant receptor tyrosine kinase signaling in lipofibromatosis: A clinicopathological and molecular genetic study of 20 cases. Mod Pathol. 2019;32:423-34.
- [CrossRef] [PubMed] [Google Scholar]
- Giant dorsal lipofibromatosis in an infant: A case report. BMC Pediatr. 2022;22:59.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging characteristics of lipofibromatosis presenting as a shoulder mass in a 16-month-old girl. Pediatr Radiol. 2010;40(Suppl 1):S43-6.
- [CrossRef] [PubMed] [Google Scholar]
- Lipofibromatosis: Report of a rare paediatric soft tissue tumour. Skeletal Radiol. 2008;37:555-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lipofibromatosis presenting as a pediatric neck mass. Int J Pediatr Otorhinolaryngol. 2004;68:1545-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fat suppression in MR imaging: Techniques and pitfalls. Radiographics. 1999;19:373-82.
- [CrossRef] [PubMed] [Google Scholar]







