Translate this page into:
Retrograde jejunogastric intussusception
*Corresponding author: V. Senthilvelmurugan, Department of Radiodiagnosis, Kauvery Hospital, Trichy, Tamil Nadu, India. drsenthilvelmuruganrd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Senthilvelmurugan V, Raam Prasanth N, Arivarasan K, Aravinth Raj S. Retrograde jejunogastric intussusception. Case Rep Clin Radiol. 2024;2:53-6. doi:10.25259/CRCR_146_2023
Abstract
Retrograde intussusception pertains to the invagination of the intussusceptum in a direction opposite to normal peristalsis. Jejunogastric intussusception (JGI) is an infrequent complication linked to procedures such as gastrojejunostomy, Billroth II gastrectomy, and Roux-en-Y anastomosis. There are four types of JGI based on the type of intussuscepted bowel loop and two types based on clinical presentation. In its acute form, JGI presents as severe intestinal blockage, a mass in the left hypochondriac region, and the occurrence of hematemesis. In a chronic situation, it leads to the recurrent episodes of feeling full in the upper abdomen and experiencing vomiting because of intermittent and reversible intussusception. The gold standard investigation for diagnosis is a contrast-enhanced computed tomography (CECT) scan. Here, we describe a case of retrograde JGI in a patient who presented with the complaints of hematemesis. The CECT scan revealed the invagination of jejunal bowel loops into the stomach. This condition was treated surgically.
Keywords
Retrograde jejunogastric intussusception
Contrast-enhanced computed tomography
Gastrojejunostomy
Hematemesis
Upper gastrointestinal bleed
INTRODUCTION
Retrograde intussusception is characterized by the intussusceptum invaginating in an antiperistaltic or proximal direction, in contrast to the typical peristaltic or distal direction.[1,2] Jejunogastric intussusception (JGI) is a rare complication associated with gastrojejunostomy, Billroth II gastrectomy, and Roux-en-Y anastomosis. For diagnostic purposes, a Contrast-enhanced computed tomography (CECT) scan is the preferred imaging method. Upper gastrointestinal (UGI) endoscopy can also aid in both diagnosis and treatment by reducing intussusception.[3] In this case, we present a patient with a history of truncal vagotomy and posterior gastrojejunostomy who presented with hematemesis. A CECT scan revealed the invagination of jejunal bowel loops into the stomach. The patient was successfully treated through surgical intervention.
CASE PRESENTATION
A 65-year-old man arrived with an abrupt onset of intense abdominal pain, along with several instances of coffee-brown-colored vomiting (approximately six to seven episodes). There was no history of fever or melena, and he had not experienced similar complaints in the past. Fourteen years ago, the patient underwent a truncal vagotomy with posterior gastrojejunostomy surgery to treat gastric outlet obstruction.
Upon examination, the patient appeared thin and drowsy but was responsive to oral commands. His vital signs were within normal range, and further investigation was planned, beginning with an UGI endoscopy.
The UGI endoscopy revealed a mass lesion located near the greater curvature of the stomach [Figure 1]. Subsequently, a CECT abdomen was conducted for a more detailed evaluation. The computed tomography (CT) scan revealed the intraluminal projection of jejunal bowel loops, including the mesentery and mesenteric vessels, into the stomach along the greater curvature [Figures 2 and 3]. This discovery aligned with the diagnosis of retrograde JGI, where the intussuscepted portion involved the efferent loop of the jejunum. The patient was scheduled for laparoscopic reduction of the JGI, along with jejunopexy. The intussuscepted portion of the efferent loop of the jejunum extended up to the proximal stomach, and manual reduction was successfully performed.
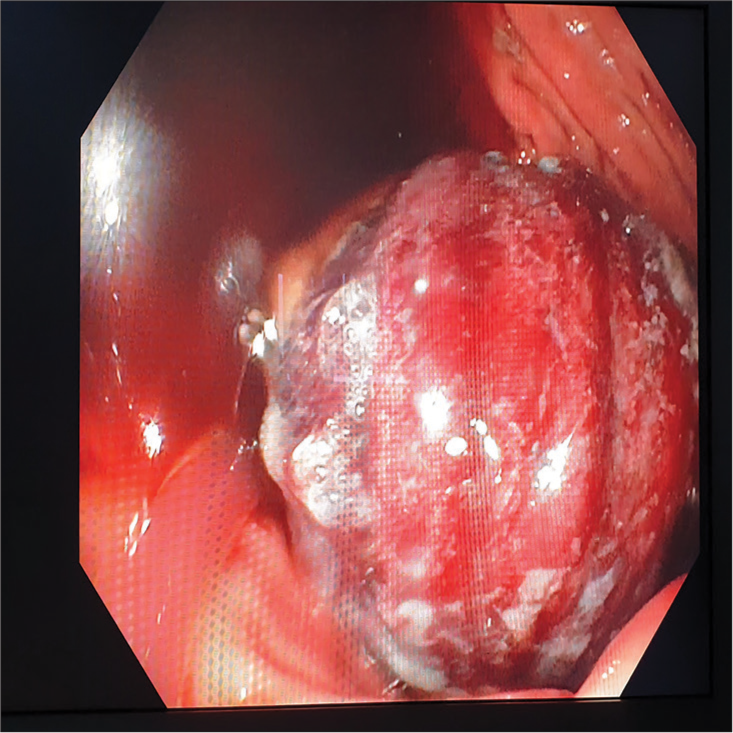
- Endoscopic image shows mass lesion in stomach.

- Topogram shows distended stomach gas shadow with intraluminal mass consistent with bowel loops.
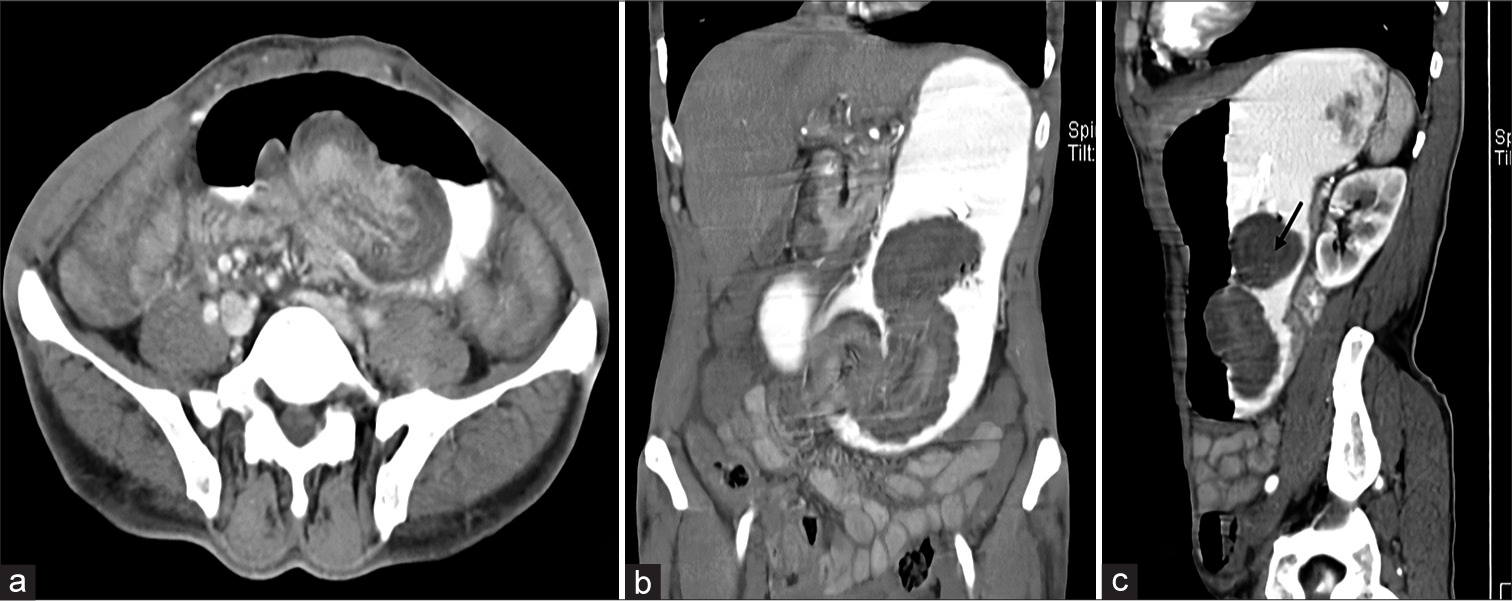
- Contrast-enhanced computed tomography (a) axial and (b) coronal sections show intraluminal projection of jejunal bowel loops along with mesenteric vessels into stomach and (c) sagittal section shows Target sign (black arrow) consistent with intussusception.
DISCUSSION
The term “retrograde intussusception” (or invagination) was first introduced by John Hunter to describe an unusual scenario, in which the intussusceptum invaginates in an antiperistaltic or proximal direction, as opposed to the more common peristaltic or distal direction.[3,4] JGI is a rare complication associated with procedures such as gastrojejunostomy, Billroth II gastrectomy, and Roux-en-Y anastomosis. Since its initial description in a patient who had undergone gastrojejunostomy, there have been fewer than 200 reported cases.[1,2]
JGI can be categorized into four distinct types depending on the loop that is intussuscepted:
Type I: Antegrade or afferent loop intussusception
Type II: Retrograde or efferent loop intussusception
Type III: A combination of both
Type IV: Intussusception following partial gastrectomy.[1-3]
Efferent loop JGI represents about 80% of cases, including the present one, whereas the remaining 20% encompass other types.[5] The precise mechanism behind JGI remains inadequately elucidated, with various functional and mechanical factors suggested but not proven. Suggested factors include antiperistalsis occurring during vomiting, adhesions that result in the bowels becoming twisted, bowel expansion subsequent to gastrectomy, jejunitis causing peristalsis to reverse, the shortening of the mesentery in the jejunal loop, constriction of the jejunum, leading to blockage that promotes antiperistalsis, an extended afferent loop, irregular motility causing spasms in the jejunum, heightened the mobility of the efferent loop, and adhesions that lead to the intussusception of a mobile segment into a fixed one. In addition, it has been proposed that increased intra-abdominal pressure, particularly in a dilated and weakened stomach after vagotomy, and retrograde peristalsis may also contribute to these occurrences.[1-3]
JGI manifests in two distinct clinical presentations. In the acute variant, it involves the imprisonment and constriction of the intussuscepted loop, leading to intense epigastric pain, vomiting, and hematemesis. The vomit initially appears clear but turns coffee-colored, with later massive hematemesis.[1,2] In the chronic form, individuals go through recurrent bouts of feeling full in the upper abdomen and experiencing vomiting due to intermittent and reversible intussusception. In approximately half of the cases, a noticeable lump in the abdomen may be detected. It’s crucial to bear in mind that the sudden onset of epigastric pain, vomiting, hematemesis, and the presence of a palpable abdominal lump in a patient with a prior history of gastric surgery may suggest the presence of JGI.[2]
Diagnostic methods encompass an abdominal X-ray, which has the potential to reveal an enlarged stomach containing a uniform mass. When employing water-soluble contrast for UGI examinations, one can observe a distinctive “coiled-spring” appearance of the jejunal intussusception within the stomach. Ultrasonography, on the other hand, exhibits an intragastric tubular mass characterized by peristaltic movement. CT scans offer insight into intragastric intussusception.[4] In addition, UGI endoscopy can serve both diagnostic and therapeutic purposes when addressing intussusception. Surgical intervention often becomes necessary upon diagnosis due to the difficulty in predicting whether the condition will resolve spontaneously or progress to gangrene.[1,2] Surgical options encompass reduction as a standalone procedure, mesentery plication within the intussusception area, anchoring the efferent loop to adjacent tissues such as the transverse mesocolon, colon, stomach, or parietal wall, or conversion to a Billroth I anastomosis. In cases involving gangrenous small intestine, resection of the affected segment remains the sole viable option.
DIFFERENTIAL DIAGNOSIS
Gastric volvulus
Gastric tumors
CONCLUSION
Retrograde JGI is an infrequent but acknowledged complication that may arise following gastrojejunostomy and Billroth II reconstruction. Early diagnosis is vital to prevent morbidity and mortality, demanding a high level of suspicion. Radiologists play a pivotal role in distinguishing this condition from postoperative internal hernias, enabling swift intervention to avert catastrophic infarction of the intussuscepted intestinal loop. Surgical treatment typically alleviates symptoms and can be lifesaving in acute cases.
TEACHING POINTS
Rare but recognizable: Jejunogastric intussusception is indeed a rare condition, but it should be kept in mind when evaluating patients who present with abdominal pain, vomiting, and a history of prior gastric surgery or gastrojejunostomy
Clinical suspicion: Physicians should maintain a high level of suspicion for jejunogastric intussusception in patients with a history of previous gastric surgery, especially when these patients develop symptoms such as vomiting, hematemesis, abdominal discomfort, and signs indicative of intestinal obstruction. Early recognition is crucial for timely intervention
Imaging importance: Radiological imaging, which includes abdominal X-rays and contrast-enhanced computed tomography scans, plays a pivotal role in both diagnosing and localizing the intussusception. These imaging modalities are instrumental in guiding healthcare professionals to implement the most appropriate management strategy.
MCQs
-
JGI occurs most commonly after which condition
Infective etiology
Post-operative
Trauma
Idiopathic
Answer Key: b
-
The most common type of JGI is
Afferent loop intussusception
Efferent loop intussusception
Combined form
Intussusception after gastrectomy
Answer Key: b
-
Investigation of choice for JGI is
Endoscopy
Barium meal
Contrast-enhanced CT scan
PET CT scan
Answer Key: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Jejunogastric intussusception: A rare complication of gastric surgery. Case Rep Surg. 2013;2013:838360.
- [CrossRef] [PubMed] [Google Scholar]
- Intussusception into the enteroanastomosis after Billroth II gastrectomy and Rouxen-Y jejunostomy: Sonographic and CT findings. AJR Am J Roentgenol. 2001;177:624-6.
- [CrossRef] [PubMed] [Google Scholar]
- Retrograde (reverse) jejunal intussusception might not be such a rare problem: A single group's experience of 23 cases. Surg Obes Relat Dis. 2008;4:77-83.
- [CrossRef] [PubMed] [Google Scholar]
- Retrograde jejunogastric intussusception following gastrectomy. Arch Surg. 1960;81:485-91.
- [CrossRef] [PubMed] [Google Scholar]







