Translate this page into:
“Leopard skin” sign: Magnetic resonance imaging appearance of Lhermitte-Duclos disease with histopathologic correlation
*Corresponding author: Anitha Mandava, Department of Radiodiagnosis, Basavatarakam Indo American Cancer Hospital and Research Institute, Hyderabad, Telangana, India. kanisri@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mandava A, Koppula V, Kodandapani S, Kommu V. “Leopard skin” sign: Magnetic resonance imaging appearance of Lhermitte-Duclos disease with histopathologic correlation. Case Rep Clin Radiol. 2024;2:36-9. doi: 10.25259/CRCR_103_2023
Abstract
Dysplastic cerebellar gangliocytoma or Lhermitte-Duclos disease (LDD) is a rare hamartomatous malformation of cerebellum that can occur in isolation or as a component of Cowden syndrome. Although uncommon, the characteristic clinical symptoms and magnetic resonance imaging (MRI) features are highly suggestive of the condition and histopathological features confirm the diagnosis. We report a case of LDD, presenting with “Leopard skin” appearance of the lesion on MRI with a brief review of imaging, clinical, and histopathological features.
Keywords
Lhermitte-Duclos disease
Dysplastic cerebellar gangliocytoma
Magnetic resonance imaging
Leopard skin sign
INTRODUCTION
Dysplastic cerebellar gangliocytoma is a rare cerebellar hamartomatous lesion with characteristic imaging features. We report a case of LDD presenting with signs of raised intracranial tension.
CASE REPORT
A 27-year-old female with a gradually progressive history of headache, giddiness, and vomiting of 2-month duration underwent evaluation with magnetic resonance imaging (MRI) at our institution. MRI of brain showed an ill-defined intra-axial lesion in the left cerebellar hemisphere with internal cystic foci and striations that are heterogeneously hypointense on T1 and hyperintense on T2-weighted images giving “leopard skin” appearance. Enhancement was not seen on contrast images and magnetic resonance spectroscopy was inconclusive. Mass effect with effacement of fourth ventricle and associated hydrocephalous was also noted [Figure 1]. Based on the location of lesion and the characteristic imaging findings, it was diagnosed as LhermitteDuclos disease (LDD). Surgery was performed with excision of lesion and histopathology confirmed the diagnosis [Figure 2]. Post-surgery, the symptoms have resolved and the patient is advised further follow-up.
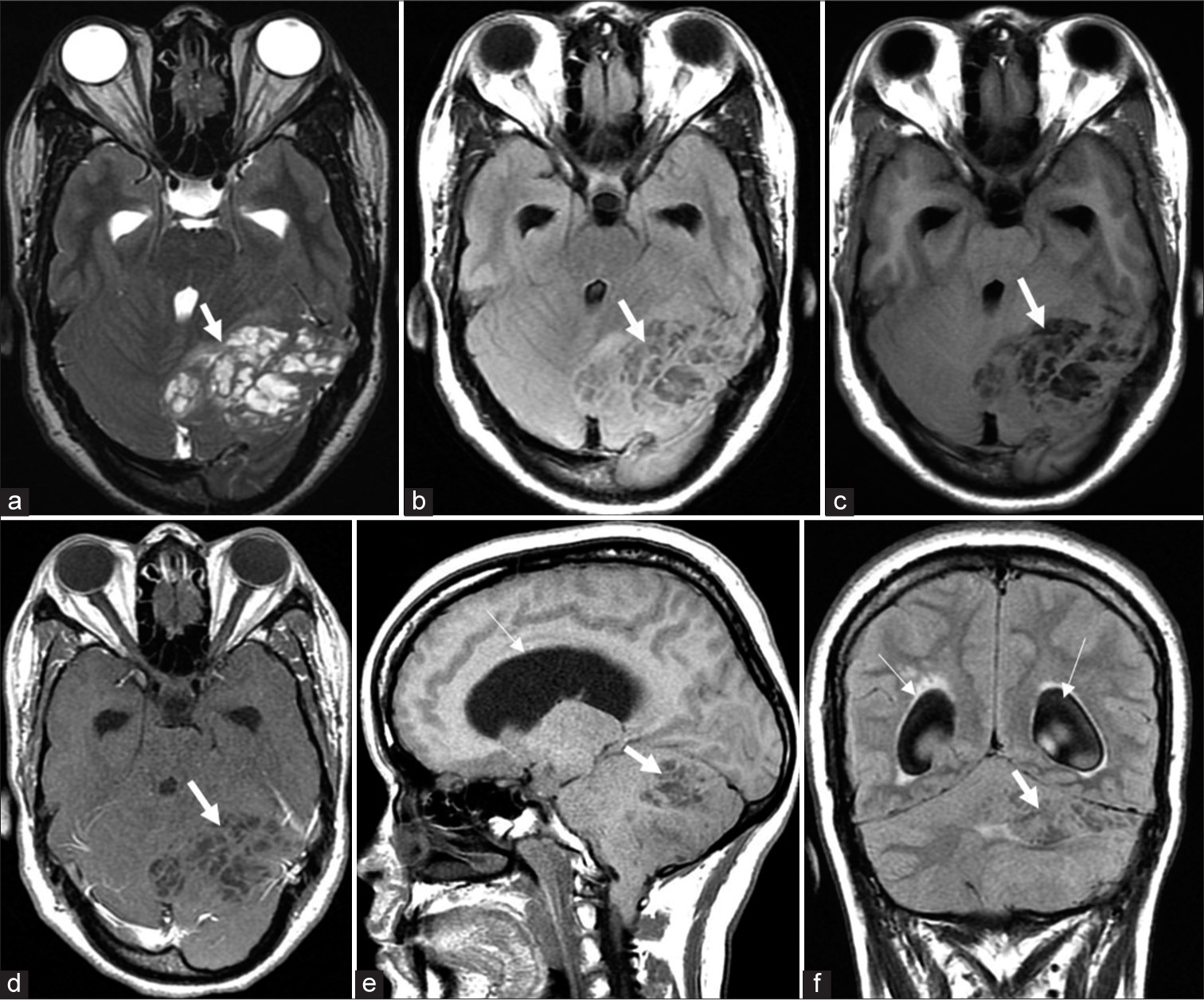
- (a-c) Axial T2-weighted image, T2-weighted-fluid-attenuated inversion recovery (T2 FLAIR), and T1-weighted image (T1W) magnetic resonance imaging images show unilateral cerebellar hypertrophy exhibiting the characteristic “leopard skin” appearance with alternating hypointense and hyperintense cystic areas and striations (thick arrows). (d) T1W contrast image shows non-enhancement of the lesion. (e and f) Sagittal T1W and coronal T2 FLAIR images show the dilated lateral ventricles (thin arrows) secondary to the lesion (thick arrows) causing obstructive hydrocephalus.
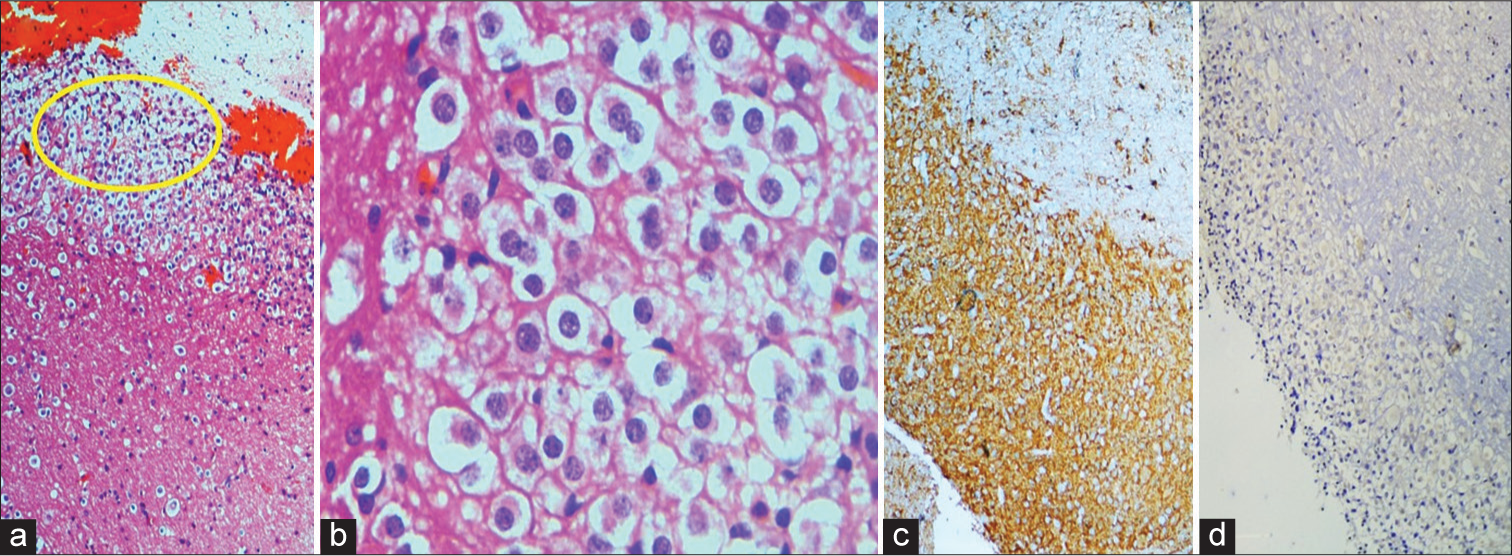
- H&E staining of tumor tissue (a). Shows diffuse enlargement of the molecular and internal granular layers with abnormally myelinated axon bundles in outer molecular layer (magnification ×10). (b) Dysplastic granular neurons shown in the inset of (a) (magnification ×40). (c and d) Immunohistochemistry positive for Synaptophysin and Ki67.
DISCUSSION
Dysplastic cerebellar gangliocytoma or LDD, named after French physicians “Jacques Jean Lhermitte” and “P Duclos,” is an uncommon hamartomatous malformation of cerebellum classified under central nervous sysytem World Health Organization Grade 1 glioneuronal and neuronal tumors.[1]
The incidence of this condition is rare with around 230 cases reported in the literature. LDD can occur either in isolation or as a component of Cowden syndrome associated with PTEN mutations. It is usually seen in adults without any race or gender predilection. Clinical symptoms depend on the size of the lesion and patients with small lesions can be asymptomatic. Patients with large lesions present with signs and symptoms of cerebellar dysfunction (vertigo and ataxia) and raised intracranial pressure due to mass effect (headache, vomiting, cranial nerve palsies, and hydrocephalus).[2] An extremely rare case of LDD presenting with psychiatric disturbances was also reported.[2]
On MRI, LDD is typically seen as an expansile unilateral cerebellar lesion with alternating hypointense and hyperintense linear and rounded areas giving rise to the typical “tigroid” pattern of appearance or the less common “Leopard skin” appearance. The lesion does not show any significant contrast enhancement or diffusion restriction.
On histopathology, macroscopically, the lesion is characterized by cerebellar folial hypertrophy and thinning of medullary white matter. On microscopic examination, the lesion characteristically shows loss of granular cells and purkinje cells with an overgrowth of dysplastic ganglionic cells.
The differential diagnosis of LDD with clinical and imaging features is given in Table 1.[3]
| Cerebellar lesion | Clinical features | MRI features |
|---|---|---|
| Lhermitte-Duclos-Disease | Dysplastic cerebellar gangliocytoma, usually seen in adults, association with Cowden’s syndrome | Alternating hypointense and hyperintense linear and rounded areas with typical “tigroid” or “Leopard skin” appearance |
| Cerebellar cortical dysplasia/heterotopias | Focal area of disorganized cerebellar architecture, association with chromosomal abnormalities, intrauterine infections, and congenital muscular dystrophies | Folial thickening, irregular grey-white matter interface, abnormal fissures, and cortical cystic lesions |
| Acute cerebellitis | Secondary to acute infection or inflammation, most commonly of viral etiology | Rarely unilateral. T2 hyperintense lesion with perilesional edema, mild diffusion restriction, and contrast-enhancement with or without adjacent leptomeningeal involvement |
| Sonic hedgehog activated medulloblastoma | Originate from the cerebellar granule neuron progenitor lineage and usually occur in the lateral parts of the cerebellar hemispheres | Isointense on T1 and T2 W sequences with cystic areas, perilesional edema, diffusion restriction, and contrast-enhancement |
| High grade neuroectodermal tumor | Associated with BCOR gene exon 15 internal tandem duplication | Large, well-circumscribed, heterogeneous masses with variable enhancement and reduced diffusion |
MRI: Magnetic resonance imaging
Asymptomatic patients can be left alone, whereas, symptomatic larger lesions causing mass effect need surgical resection.[4] Although complete surgical resection is not possible in all the cases and recurrence can occur after surgery, prognosis is favorable due to the slow growth and progression of the lesion.[4,5]
CONCLUSION
LDD should be considered as a differential diagnosis in young adults presenting with signs and symptoms of unilateral cerebellar mass and raised intracranial hypertension.
LEARNING POINTS
Although the incidence of LDD is extremely rare, clinical symptoms related to the location of the lesion and the characteristic “tigroid” or “leopard skin” MR imaging appearance are diagnostic of this condition, and the typical histopathologic features confirm the diagnosis.
LDD occurring as a part of Cowden syndrome (multiple hamartoma syndrome) is associated with increased risk of melanomas, breast, endometrium, thyroid, and colorectal malignancies; hence, further clinical assessment and radiological screening are recommended in these patients.
MCQs
-
The most common malignancy associated with Cowden’s syndrome is
Ductal breast cancer
Dysplastic gangliocytoma of the cerebellum
Colorectal cancer
Melanoma
Answer Key: a
-
18FDG PET/CT scan in LDD shows
Increased uptake in all lesions
Increased uptake in the vicinity of the lesions
Increased uptake in and around the lesions
Variable uptake in and around the lesion, not specific for the diagnosis
Answer Key: d
-
In regard to calcifications in the lesions of LDD, the following statement is correct
Calcifications are seen in all the lesions
Calcifications are seen in few cases
Lesions never exhibit calcifications
None of the above
Answer Key: b
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The 2021 WHO classification of tumors of the central nervous system: A summary. Neuro Oncol. 2021;23:1231-51.
- [CrossRef] [PubMed] [Google Scholar]
- A case report of Lhermitte-Duclos disease revealed by psychiatric disturbances. Ann Gen Psychiatry. 2017;16:24.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging spectrum of cerebellar pathologies: A pictorial essay. Pol J Radiol. 2015;80:142-50.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic findings of dysplastic cerebellar gangliocytoma (Lhermitte-Duclos disease) in a woman with Cowden syndrome: A case study and literature review. J Radiol Case Rep. 2020;14:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Lhermitte-Duclos disease: Assessment with MR imaging, positron emission tomography, single-photon emission CT, and MR spectroscopy. AJNR Am J Neuroradiol. 2001;22:824-30.
- [Google Scholar]







