Translate this page into:
Rare benign breast neoplasm masquerading as malignancy on anatomical and functional imaging with contrast-enhanced mammography
*Corresponding author: Porkodi Dharmalingam, Institute of Radiodiagnosis, Government Kilpauk Medical College and Hospital, Chennai, Tamil Nadu, India. porkodid1976@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dharmalingam P, Jagannathan D. Rare benign breast neoplasm masquerading as malignancy on anatomical and functional imaging with contrast-enhanced mammography. Case Rep Clin Radiol. doi: 10.25259/CRCR_47_2024
Abstract
We discuss a unique case of a benign breast neoplasm that initially appeared to be an intracystic papillary carcinoma on digital breast tomosynthesis, ultrasound, and contrast-enhanced mammogram. However, subsequent histopathological examination (HPE) revealed it to be a benign adenomyoepithelioma, an uncommon neoplasm in the breast. Understanding this rare condition and confirming it pre-operatively through HPE can prevent unnecessary aggressive treatment.
Keywords
Benign adenomyoepithelioma
Contrast-enhanced mammography
Breast neoplasm
Circumscribed complex cystic lesion
INTRODUCTION
Adenomyoepithelioma (AME) of the breast is an extremely rare neoplasm, most often benign, but with a high recurrence rate and the potential to metastasize, although with a likelihood of malignant transformation.[1-4] AME is characterized histopathologically by the simultaneous proliferation of epithelial and myoepithelial cells.[1-3] Due to their rarity, literature on their radiological presentation is scarce. To our knowledge, there is no data available on the contrast-enhanced mammogram (CEM) features of AME. This case report discusses the digital breast tomosynthesis (DBT), ultrasound (US), and CEM features of a benign AME case.
CASE REPORT
A 70-year-old female presented with complaints of a lump in her left breast for 2 months. Over the past 15 days, she developed skin ulceration and bleeding at the site of the lump. On inspection, the left breast was enlarged with contour deformity. The skin appeared stretched and thinned and presented with a small ulcer, which was actively bleeding. Palpation revealed a large, firm lump occupying all four quadrants of the breast.
With DBT, a large circumscribed oval mass lesion with variable density (peripheral low density and central equal density) measuring 11 × 9 cm was observed in the central compartment, extending to all four quadrants of the left breast. The skin overlying the lump appeared stretched, causing deformity of the breast contour. No associated micro/macrocalcifications were noted.
US of left breast showed a large complex cystic lesion of size 10.7 × 8.8 × 9.4 cm containing multiple irregular solid components and dense mobile internal echoes within the cystic component, occupying all four quadrants. On Doppler examination, internal vascularity was noted in the solid component. Both of the axillae were clear with no evidence of axillary lymphadenopathy [Figure 1].
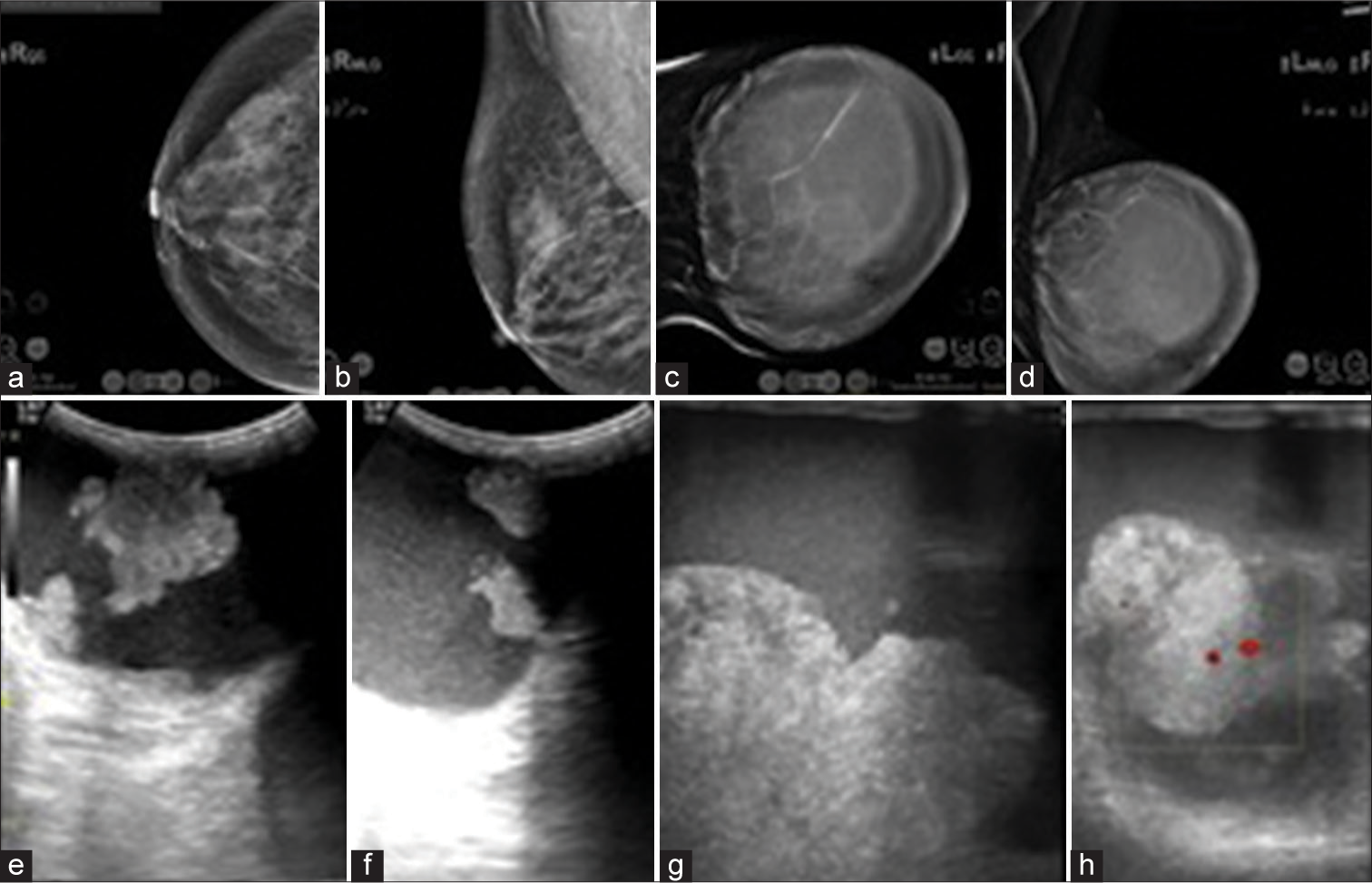
- (a-d) Digital Breast Tomosynthesis images of both breasts; (e-f) US images of left breast. (a and b) CC and MLO views of right breast- BIRADS-1. (c and d) CC and MLO views of left breast show a large circumscribed mass lesion with variable density (central equal density and peripheral low density areas) causing stretching of overlying skin and deformity of left breast contour- BIRADS 4c. (e and f) low frequency US images and (g and h) high frequency US images of left breast show circumscribed complex cystic lesion with multiple irregular solid components and vascularity within the solid component. CC: Craniocaudal, MLO: Mediolateral oblique, BIRADS: Breast imaging reporting and data system, US: ultrasound.
With CEM, the lesion showed uniform thin rim of enhancement with multiple irregular enhancing mural nodules amidst adjacent areas of negative enhancement. The lesion exhibited moderate conspicuity at 2 min and plateau kinetics on the delayed phase (8-min post-contrast image) compared to the 2-min post-contrast image.
DBT features were indeterminate; however [Figure 2], based on the findings from US and CEM, intracystic papillary carcinoma was suspected. The final impression, considering DBT, US, and CEM, was given as breast imaging-reporting and data system 4C.
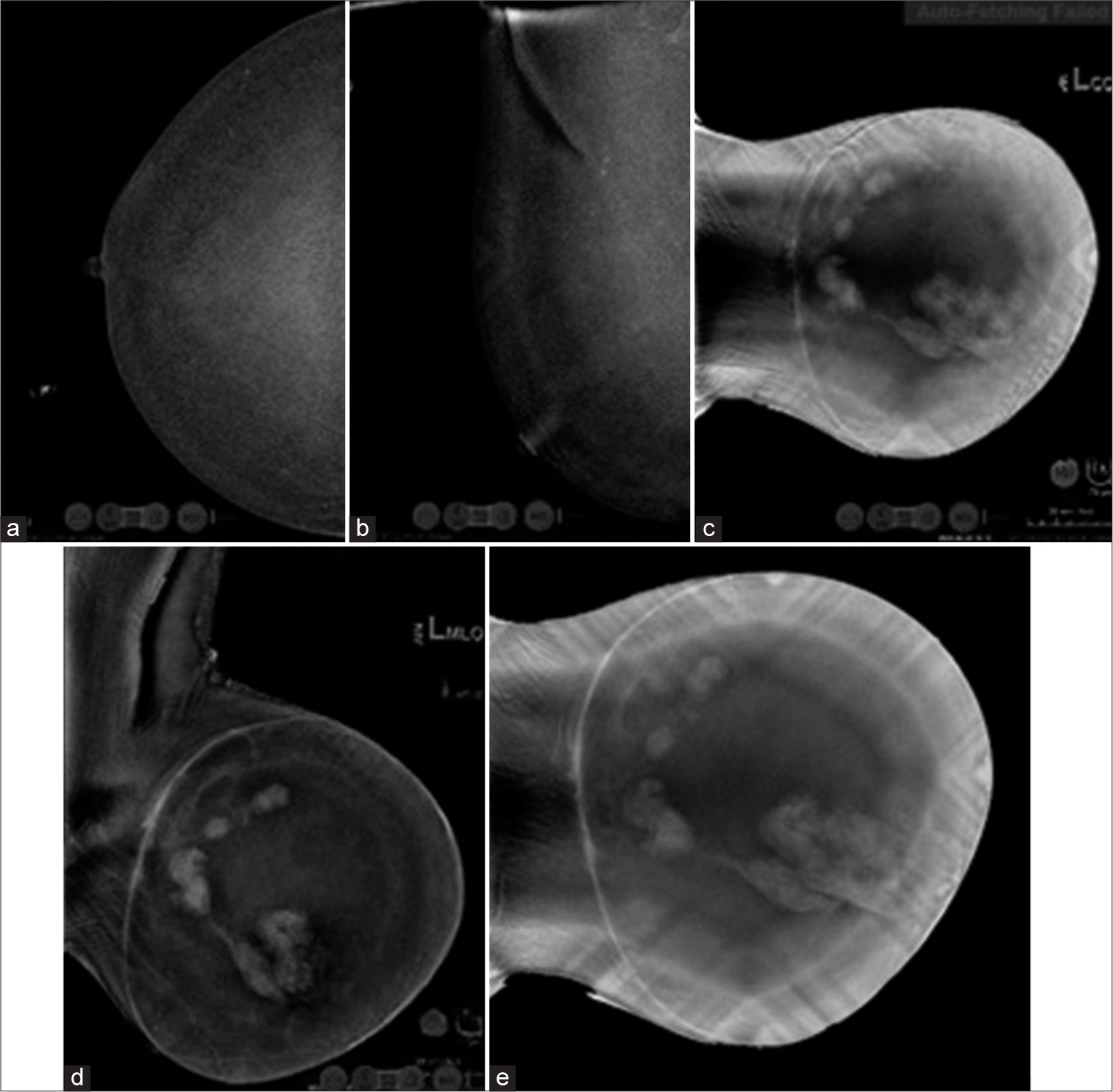
- Contrast Enhanced Mammogram images. (a and b) Post contrast images of right breast show minimal background parenchymal enhancement with no abnormal enhancing lesion- BIRADS-1. (c) 2-min post CC view of left breast, (d) 4-min MLO view of left breast (e) 8-min (delayed) CC view of left breast show smooth thin rim enhancing mass with multiple enhancing mural nodules amidst adjacent negative internal enhancement with plateau kinetics in the delayed image as compared to the initial image- BIRADS 4c. CC: Craniocaudal, MLO: Mediolateral oblique, BIRADS: Breast imaging reporting and data system.
In such cases, fine needle aspiration cytology (FNAC) is considered obsolete. As anticipated, the US-guided FNAC yielded inconclusive results, indicating epithelial proliferation. Subsequently, an US-guided core biopsy was performed. The histopathological examination (HPE) revealed multiple linear tissue fragments demonstrating proliferation of round to angulated tubules lined by epithelial and myoepithelial cell layers, and intervening scant fibrous stroma with numerous congested vessels was also observed. Hence, it was reported as benign AME. Immunohistochemistry (IHC) analysis of the specimen revealed the following: estrogen receptor positivity in 90% of cells with strong intensity, progesterone receptor positivity in 90% of cells with strong intensity, Her2Neu negativity, Ki67 positivity in approximately 5% of cells, and P63 positivity in myoepithelial cells in all tubules and glands [Figure 3].
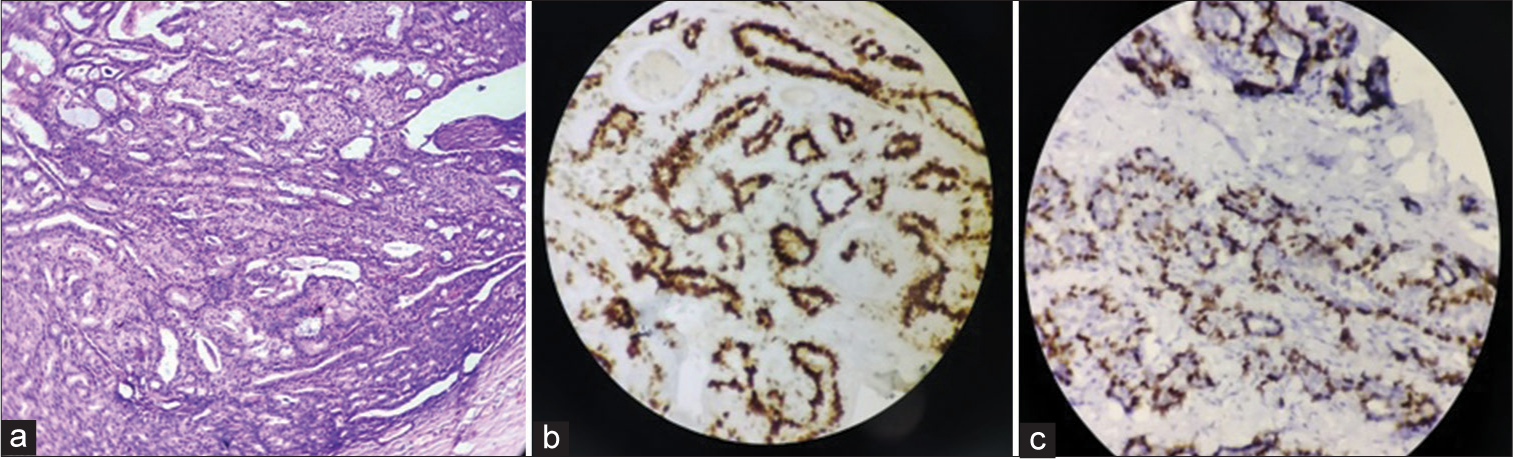
- (a) Histopathological examination image- benign adenomyoepithelioma of breast, (b) immunohistochemistry (IHC) image-Estrogen receptor positive in myoepithelial cells, (c) IHC image-p63 positive in myoepithelial cells.
Subsequently, a wide local excision of the mass was performed outside. The patient continues to do well to date.
DISCUSSION
AME is an uncommon breast tumor, typically non-cancerous, yet characterized by a notable recurrence rate. It has low likelihood of becoming malignant, and even a benign lesion has the propensity for metastasis.[3,4] It predominantly occurs in women and is extremely rare in men[3,5,6] The age group affected varies from 16 to 81 years, with the incidence increasing with age.[1,7] Bilateral benign AME is extremely uncommon and has been scarcely documented.[7] It typically manifests as a unilateral mass, preferably within the central compartment. Imaging characteristics are non-specific, often resembling either benign or malignant lesions.[3-9] These presentations may include irregular masses, well-defined solid lesions, or complex solid-cystic formations, sometimes appearing as asymmetries on mammography.[3-11] Associated pleomorphic microcalcifications have been reported in only one case.[8] Vascularity is typically evident within the solid portion on Doppler imaging or as an enhancing solid component exhibiting washout kinetics on contrast-enhanced MRI.[5] Histologically, AME is distinguished by the simultaneous growth of myoepithelial and epithelial cells in two distinct layers. Diagnosing AME can be challenging due to its diverse histological traits and the variability observed within these tumors.[1,2] Our case presented as a circumscribed complex solid cystic mass with internal hemorrhage in the cystic component and vascularity in the solid component evidenced by internal vascularity on Doppler and enhancing nodules with plateau kinetics on CEM, mimicking papillary carcinoma. Consistent with the literature review, FNAC yielded inconclusive results. However, a core needle biopsy, complemented by IHC, provided the diagnosis in our case. Surgical excision with wide margins is recommended for confirming and treating AME due to its tendency for recurrence and the potential for malignant transformation. This approach was followed accordingly in our case.
DIFFERENTIAL DIAGNOSIS
The differentials for the imaging findings of our case of benign AME of breast are outlined in Table 1.
| Differential diagnosis | Discriminating features |
|---|---|
| Intracystic benign papilloma | Cyst with mural nodule with or without enhancement. Usually size varies from few millimetres to 2 cm. Rarely, giant intra cystic papilloma may present with larger size, posing diagnostic difficulty |
| Encapsulated papillary carcinoma with or without invasion | Usually, thin-walled cyst with mural nodule with vascularity, showing enhancement with contrast and washout kinetics No discriminating imaging features |
| Necrotic malignancy | Usually associated with irregular/thick enhancing wall with/without enhancing septae |
| Acute suppurative lesion/granulomatous lesion | Commonly associated with thick/irregular hyperemic walls, adjacent parenchymal edema, skin and subcutaneous thickening. Granulomatous lesions may present with sinus |
| Phyllodes tumor | Variable size, predominantly solid with internal small cystic areas with vascularity in solid component, heterogenous contrast enhancement with variable contrast kinetics |
CONCLUSION
AME of the breast is an uncommon tumor with diverse imaging features that can sometimes resemble malignant tumors in both anatomical and functional imaging, such as CEM. Consequently, false-positive diagnoses based on imaging are common. Recognizing this condition, especially when it presents as a lesion without calcification, is crucial for considering it as a potential diagnosis. This highlights the necessity biopsy and IHC confirmation. HPE ensures accurate diagnosis and facilitates appropriate treatment, such as wide local excision, rather than resorting to more aggressive approaches such as modified radical mastectomy and axillary dissection.
TEACHING POINTS
It is imperative to be aware of this entity, as it is an uncommon neoplasm in the breast with variable imaging features that require confirmation by HPE.
AME may have variable imaging features, such as non-calcified lesions in plain mammograms, internal vascularity in the solid component detected with Doppler, and enhancing solid component with malignant contrast kinetics in CEM that can lead to false-positive diagnoses with imaging. This awareness helps us to keep it in mind as a differential diagnosis since the treatment modality varies from malignant lesions.
MCQs
-
The common plain mammographic features of benign adenomyoepithelioma of the breast may include any of the following, except
Circumscribed mass
Irregular mass
Focal asymmetry
Associated calcifications
Answer key: d
-
Which among the following may be the typical US features of adenomyoepithelioma
Circumscribed mass, either solid or complex solid-cystic mass
Irregular mass with spiculations
Internal vascularity on Doppler
All the above
Answer key: d
-
With contrast-enhanced mammogram (CEM), benign adenomyoepithelioma may commonly manifest in the following ways, except:
Absent enhancement
Irregular heterogeneously enhancing solid mass
Circumscribed thin rim enhancing lesion with enhancing mural nodule/nodules
Plateau/washout contrast kinetics
Answer key: a
-
The following facts are true about benign adenomyoepithelioma, except
Wide local excision is the treatment of choice
Fine-needle aspiration cytology (FNAC) usually confirms the diagnosis
Metastasis can occur
Local recurrence is common
Answer key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Adenomyoepithelioma of the breast: A case report and a review of the literature. Breast Cancer. 1996;3:65-9.
- [CrossRef] [Google Scholar]
- Adenomyoepithelioma of the breast: A brief diagnostic review. Arch Pathol Lab Med. 2013;137:725-9.
- [CrossRef] [Google Scholar]
- Adenomyoepithelioma of the breast: Spectrum of disease with associated imaging and pathology. Am J Roentgenol. 2003;180:799-803.
- [CrossRef] [Google Scholar]
- "Benign," metastasizing adenomyoepithelioma of the breast: A report of 2 cases. Arch Pathol Lab Med. 2006;130:1349-53.
- [CrossRef] [Google Scholar]
- Adenomyoepithelialtumors of the breast: imaging findings with histopathologic correlation. Am J Roentgenol. 2011;197:W184-90.
- [CrossRef] [Google Scholar]
- Benign adenomyoepitelioma of the breast: Presentation of two rare cases and review of literature. Int J Surg Case Rep. 2020;67:1-4.
- [CrossRef] [Google Scholar]
- Bilateral adenomyoepithelioma of breast. J Cancer Res Ther. 2013;9:523-5.
- [CrossRef] [Google Scholar]
- Benign adenomyoepithelioma of the breast: Imaging findings mimicking malignancy and histopathological features. Acta Radiol. 2007;48:27-9.
- [CrossRef] [Google Scholar]
- Intracystic adenomyoepithelioma of the breast-case report and review. Breast Cancer. 2007;14:429-33.
- [CrossRef] [Google Scholar]
- Adenomyoepithelioma of the breast: Radiologic-pathologic correlation and management. J Breast Imaging. 2024;6:64-71.
- [CrossRef] [Google Scholar]
- Benign adenomyoepithelioma of the breast: A case report and review of imaging features. Cureus. 2024;16:e58421.
- [CrossRef] [Google Scholar]








