Translate this page into:
Parotid duct sialocele following dental procedure: An uncommon cause of right oro-buccal swelling; with review of literature
*Corresponding author: Debraj Saha, Department of Radiodiagnosis, Shatabdi Hospital, Mumbai, Maharashtra, India. debrajdon7521@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Masrani S, Saha D, Singhai A, Sanghavi S. Parotid duct sialocele following dental procedure: An uncommon cause of right oro-buccal swelling; with review of literature. Case Rep Clin Radiol. 2024;2:49-52. doi: 10.25259/CRCR_106_2023
Abstract
There are various types of masses seen in the parotid region; however, parotid duct sialocele is a cystic mass seen arising at the expense of the parotid duct following a facial trauma or post-surgery. It may occur secondary to a stricture formed at the end of the duct or due to a complete laceration of the salivary gland. In our case, a 36-year-old female patient came to the outpatient department with a fullness of mouth in the right cheek, was evaluated clinically by the surgeon, and was sent to the radiology department for ultrasonography. Ultrasonography and a computed tomography (CT) scan were performed, and a diagnosis of parotid duct sialocele secondary to stenosis in the parotid duct was made. The patient underwent surgery, and the mass was removed. Parotid duct sialocele is a salivary cavity arising at the expense of the parotid duct. Facial trauma is the most common cause of this rare condition. If left untreated, a sialocele may develop into a significantly large facial swelling. Fistula formation may occur, often draining extraorally. We report a case of parotid duct sialocele that was assessed by sialography and ultrasonography and managed by the placement of an intraductal cannula for 15 days until the duct was found patent. We also discuss various treatment options for this condition in this case report.
Keywords
Ultrasonography
Computed tomography scan
Sialocele
Parotid duct
INTRODUCTION
There are different types of facial masses with which a patient comes to the outpatient department for evaluation. Parotid duct sialocele is a relatively rare mass that is formed involving the parotid duct secondary to degeneration of the parotid gland or distal obstruction of the Stenson’s duct. The possible causes are facial trauma and post-surgery. Complications of sialocele, such as abscess or fistula formation, have been mentioned.[1]
CASE REPORT
A 36-year-old male complained of fullness in the right cheek [Figure 1] immediately after putting a morsel of food in his mouth, the swelling was maximum on coming in contact with sour food and was mildly painful. The patient gradually realized that he could compress the swelling, which resulted in fluid accumulation on the right side of his mouth.

- Clinical photograph of the patient with swelling in the right parotid region.
He gave a past history of recurrent dental procedures in the left upper jaw spanning over the last 3–4 months. This was followed by tooth extraction of the carious right upper 2nd molar; the tooth was apparently maligned with the rest of the dental apparatus of the right upper jaw, which can be inferred from the patient’s complaint that he had developed soreness in the region of the upper gingival mucosa, which, on examination, was in the vicinity of the punctum of the opening of the left main Stensen’s duct opposite the upper 2nd molar tooth.
On high-frequency ultrasound with a 7–11 MHz linear probe, small foci of air appearing as small echogenic foci with dirty shadowing were seen in the right parotid gland, but there was no intra-glandular acinar or lobular distension with secretions. Foci of mobile, non-dependent air in a large fusiform collection [Figure 2a] in the subcutaneous plane and along the course of the right main parotid duct measuring approximately 5 × 2 × 3 cm were seen in the soft tissue of the right mid-cheek.
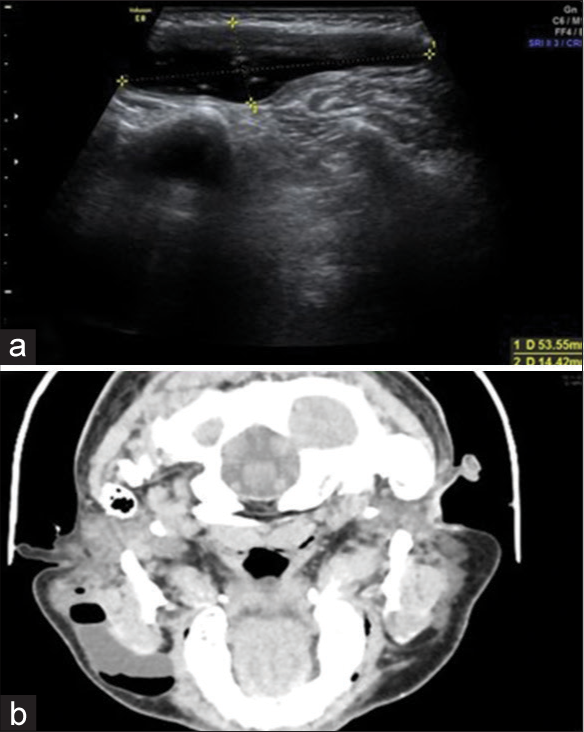
- (a) Ultrasonography image in axial plane with a linear transducer over the right cheek region; shows the size of the swelling of around 5×1.5 cm; (b) contrast-enhanced axial image of the face and neck depicts a large cystic swelling in the right parotid region; with air-fluid levels; along the direction of the right parotid gland.
A computed tomography (CT) scan of the region [Figure 2b] shows an air-fluid level in the cystic fusiform region of the dilated right main parotid duct with a significant increase in the air content on puffing the cheek with oral air, indicative of communication of the cavity with the oral cavity, and length of the stricture is only a few millimeters from the punctum to the medial edge of the dilated region of the duct.
A provisional diagnosis of sialocele of the right main parotid (Stensen’s) duct was made, which was corroborated by a CT scan. A magnetic resonance imaging scan was also sought for further evaluation and for measurement of the terminal duct stricture as the likely cause of the sialocele, which was probably secondary to the repeated dental microtrauma.
The patient was given conservative treatment such as compression dressings and anti-sialagogues for a month; however, as the patient was quite symptomatic, the decision was taken to completely excise the mass. Under all aseptic precautions and with informed consent, the mass was excised [Figure 3]. Post-procedural vitals were stable. The patient followed up after 1 month without any recurrence of the lesion.
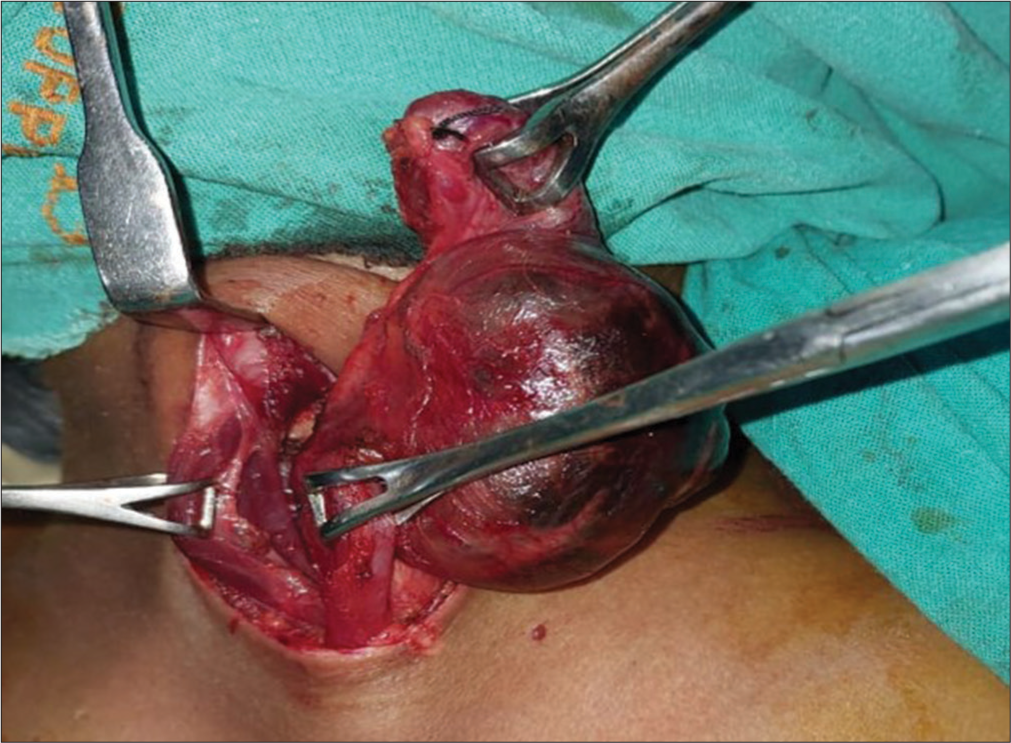
- Intraoperative zoomed image depicts the photography of removal of the parotid duct sialocele.
DISCUSSION
Sialocele of the parotid duct is a frequently reported entity in the literature and is essentially post-traumatic or iatrogenic after dental extraction of superficial parotidectomy. The diagnosis is made clinically after a proper evaluation of the mass and history.[2] Differential diagnosis of intraparenchymal parotid lesions includes Warthin’s tumor, first branchial cleft cyst, parotid lymphangioma, benign lymphoepithelial cysts, and necrotic lymph nodes. However, that of extraparenchymal lesions includes retention cysts, sialodochitis, branchial cleft cyst, and a lymphoepithelial cyst.[3] Table 1 depicts the different radiological features of the differential diagnostic entities of extraparenchymal parotid lesion. Ultrasonography and CT scan are the current preferred modalities for evaluation of the mass, confirmation of the diagnosis, assessing the causes, looking for the extent, assessing any potential complications, and planning the management.[4] Management can be non-surgical or surgical. Non-surgical methods include compression, anti-sialagogues, and needle aspiration. Even intraoral parotid duct catheterization may also be tried out.[5] If left untreated, potential complications include fistula and abscess formation. Other potential sites of sialocele are parotid gland; submandibular gland; sublingual; pharyngeal; and zygomatic.
| Entity | Radiological features |
|---|---|
| Retention cyst | Cystic lesion proximal to the level of obstruction of the duct |
| Sialodochitis | Inflammation of the parotid duct with associated duct wall thickening; fat stranding and possible intraductal calculus. There will be associated ductal stenosis or dilation; giving rise to “sausage link appearance” |
| First branchial cleft cyst | Well-defined cystic masses located superficial to, within, or deep to the parotid gland. If they form a sinus, the sinus tract can be identified draining into the external auditory canal or even extending to the hyoid bone |
| Lymphoepithelial cyst | Multiple well circumscribed small lesions scattered throughout; may be associated with a mural nodule; association with HIV/Sjogren’s syndrome. |
CONCLUSION
Although there is a lower percentage of patients presenting with post-traumatic or iatrogenic parotid sialocele, surgeons, dentists, and radiologists must be aware of this entity, as the condition is easily diagnosed and there are multimodality methods for treating it.
TEACHING POINTS
Parotid duct sialocele is a rare but important cause of right-sided buccal swelling, especially if there is a previous history of facial trauma; and/or a surgical procedure
Ultrasonography is a simple yet effective method for diagnosing the condition and characterizing the lesion
CT scan and confirm the extent of the lesion, along with a demonstration of the pathology
Warthin’s tumor, first branchial cleft cyst, and parotid gland lymphangioma are the few other differential diagnoses that should be considered while evaluating the lesion.
MCQs
-
What is the name of the duct that drains the parotid gland?
Duct of Rivinus
Duct of Wirsung
Wharton duct
Stensen duct
Answer Key: d
-
All of the following are differentials of an intra-parotid swelling except
Warthin tumor
Second branchial cleft cyst
First branchial cleft cyst
Lymphoepithelial cysts of HIV.
Answer Key: b
-
Which of the following is a contraindication to conventional sialography?
Acute sialadenitis
Sialocele
Sialolithiasis
Sialectasis
Answer Key: a
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Repair of traumatic pseudocyst of parotid duct. J Indian Dent Assoc. 1979;51:89-90.
- [Google Scholar]
- Post traumatic parotid fistulae and sialocele a prospective study of conservative management in 51 cases. Ann Surg. 1989;209:105-11.
- [CrossRef] [PubMed] [Google Scholar]
- Post traumatic parotid sialocele: Report of two cases. J Oral Maxillofac Surg. 1999;57:742-5.
- [CrossRef] [PubMed] [Google Scholar]
- Some sialographic findings in traumatic lesions of the parotid duct and gland. Am J Roentgenol Radium Ther Nucl Med. 1967;100:656-63.
- [CrossRef] [PubMed] [Google Scholar]
- Sialocele: An unusual case report and its management. Indian J Dent Res. 2011;22:336-9.
- [CrossRef] [PubMed] [Google Scholar]







