Translate this page into:
An often-forgotten cause of perihepatic abscess following cholecystectomy
*Corresponding author: Anderson Kuo, Department of Radiology, Midland Memorial Hospital, Midland, Texas, United States. anderson.kuo@midlandhealth.org
-
Received: ,
Accepted: ,
How to cite this article: Kondoor V, Le D, Kuo A. An often-forgotten cause of perihepatic abscess following cholecystectomy. Case Rep Clin Radiol. 2024;2:45-8. doi: 10.25259/CRCR_126_2023
Abstract
Gallbladder perforation during laparoscopic cholecystectomy with gallstone spillage is common and typically without serious sequela. Rarely, retained gallstones may cause important complications such as focal infection, fistula formation, and adhesions. Here, a case of dropped gallstone related perihepatic abscess and sepsis is presented. Because the retained stone location and timeline of presentation are both highly variable, accurate diagnosis can be difficult. Knowledge of this condition is thus paramount to prompt consideration of this possibility.
Keywords
Gallstones
Cholelithiasis
Cholecystectomy
INTRODUCTION
Gallbladder disease is common. In particular, cholelithiasis affects approximately 15% of the adult population, corresponding to an estimated annual cost of 6 billion direct and indirect health-care dollars in the US.[1] Laparoscopic cholecystectomy has become the mainstay treatment due to its minimally invasive nature, shorter hospital stay, lower infection rate, decreased cost, better cosmesis, and lower mortality.[2] However, risk of procedure-related gallbladder perforation and gallstone spillage is increased compared to open cholecystectomy secondary to limited control of the surgical field. When recognized, retrieval of the dropped stone may be attempted with or without washout and conversion to open surgery. Sadly, not all cases of gallstone spillage are feasibly removed (36% could not in one series[3]). Here, a case of delayed complication from an unrecognized retained gallstone is presented.
CASE REPORT
A 61-year-old female presented with chief complaint of backpain, subjective fever, and chills. Medical history was relevant for Class III obesity (body mass index 48). Physical examination revealed tenderness across the upper abdomen without rebound. Ultrasound findings were suggestive of cholelithiasis with acute cholecystitis (not shown), confirmed on subsequent magnetic resonance cholangiopancreatography performed for evaluation of possible associated choledocholithiasis [Figure 1]. Laparoscopic cholecystectomy was thus performed. No complication was reported, although the procedure was noted to be difficult.
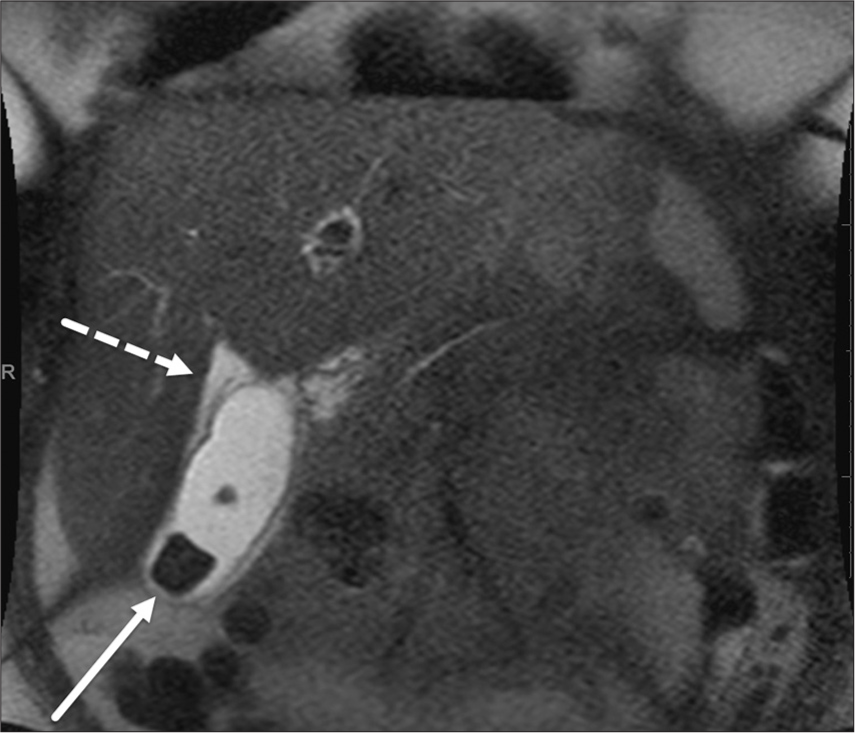
- Magnetic resonance cholangiopancreatography image shows cholelithiasis with rectangular gallstones (solid arrow) with gallbladder wall edema and pericholecystic fluid (dashed arrow), compatible with acute cholecystitis.
Eight months later, an outpatient contrast computed tomography (CT) of the chest was performed to evaluate shortness of breath and cough. Ground-glass opacities of the lungs were seen, suspicious for resolving viral pneumonitis and thought to account for the presenting symptoms. In addition, a fluid collection was seen in the subdiaphragmatic space abutting the left hepatic dome, which was noted to contain a rectangular peripherally calcified internal focus [Figure 2a]. Dropped gallstone from prior cholecystectomy with abscess formation was proposed. However, due to neither significant upper abdominal symptoms nor laboratory findings of infection (white blood cells [WBC]: 3.49, upper normal reference limit 10.8; 49% neutrophils), no intervention was pursued at this time.
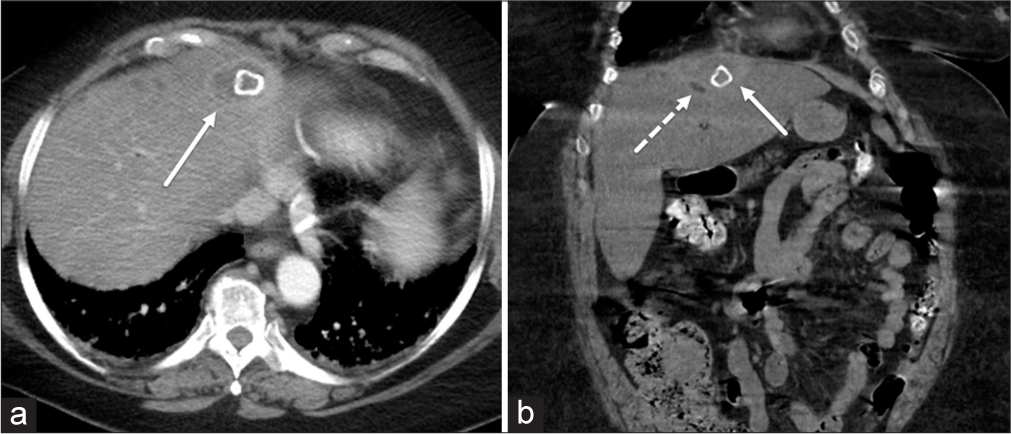
- (a) Contrast-enhanced computed tomography (CT) of the upper abdomen shows a new fluid collection in the subdiaphragmatic space (solid arrow) with an internal rectangular peripherally calcified focus reminiscent of a gallstone. (b) Follow-up non-contrast CT again shows the subdiaphragmatic fluid collection (solid arrow), now with adjacent area of hypodensity (dashed arrow) that is suspicious for infectious changes.
Seven months later, the patient presented to the emergency department, this time with severe right upper abdominal pain and in septic shock. The presenting vitals were: Blood pressure of 72/55, respiration of 22 breaths/min, heart rate of 90 beats/min, and oral temperature of 36°C. Laboratory evaluation revealed leukocytosis (WBC 13.89; 78% neutrophils). Due to concurrent acute kidney injury (creatinine 3.4 mg/dL, estimated glomerular filtration rate 14 mL/min), a non-contrast CT of the abdomen and pelvis was performed. The previously seen sub-diaphragmatic space calcified focus containing abscess was reidentified with mild interval increase in size of the collection [Figure 2b]. A small amount of hypodensity/fluid was seen in the surrounding region, not previously present. Overall diagnosis of dropped gallstone-related chronic abscess formation with focal hepatitis was thus made. Surgical consultation was requested with ensuing abscess evacuation and retrieval of the peripherally calcified focus. Frank pus was expressed intraoperatively with perihepatic adhesions. Gross pathology examination was consistent with a cholelith. Culture of the obtained material was positive for mostly Streptococcus sanguinis and some Bacillus spp.
DISCUSSION
Surgical bed fluid collection, hepatic trauma, biliary leak, vascular injury, and bowel perforation are well known complications of cholecystectomy. In contrast, dropped gallstones are a less well appreciated complication and more often a diagnostic challenge. In this case, delayed complications from a dropped gallstone are presented with relatively typical features.
It should first be noted that while gallbladder perforation and gallstone spillage are not rare, the vast majority of the cases do not cause significant harm. In the largest analysis to date including 10,174 patients who underwent laparoscopic cholecystectomy, Schäfer et al. reported gallstone spillage in 581 patients (5.7%) but only 8 (0.08%) of which had attributable complications.[4] In that series, 34 cases were converted to open procedure with retrieval of the lost gallstones. Male sex, older age, increased body weight, and presence of omental adhesions are associated with increased risk of gallbladder perforation,[5] presumably due to increased difficulty with gallbladder dissection or extraction through the trocar. With open laparotomy, spillage of the gallstones is less common and more readily identified and corrected, making spillage-related complications much less likely.[4]
Early electron microscopy study showed a large portion of pigmented and composite stones have live bacteria internally, not seen in cholesterol stones.[6] Experimentally in animal studies, sterile dropped stones were found to lead to granuloma formation, and infectious stones (or those with infected bile) result in abscesses.[7] In keeping with this finding, a dropped stone from cholecystectomy for acute cholecystitis is more frequently problematic than that for cholelithiasis.[4] Abscess formation and trocar site/abdominal wall fistula are the most common complications.[8] Other less common complications of dropped gallstone include adhesions, cholangitis, bowel obstruction or volvulus, vascular thrombosis, and infection of other organs.
On imaging, the most classic finding is a perihepatic or trocar track gallstone containing fluid collection/abscess. Secondary inflammation of the surrounding tissue or resultant systemic infection may be present. While geometric calcified gallstones are easy to identify, some gallstones may demonstrate irregular calcification or appear hypodense (fat or air in density), making diagnosis more difficult. Similarly, due to insufflation during the laparoscopy, the gallstone may be lost in various parts of the peritoneal cavity, complicating identification.[9] Another contributing factor to the diagnostic challenge is the somewhat unpredictable time course. Dropped gallstone complication has a peak incidence at 4 months but with a large degree of variability.[7] The case may present in a few weeks following cholecystectomy to as late as 20 years in one report.[10] Without awareness of the typically delayed presentation, the abscess may be dismissed as idiopathic in origin, leading to unnecessary work-up.
CONCLUSION
Despite its rarity, gallstone spillage-related complication may lead to significant morbidity and present as diagnostic dilemmas to those unaware. Fluid collection containing focal hyperdensity or hypodensity in a patient with prior laparoscopic cholecystectomy for acute cholecystitis should raise suspicion of this possibility. Delayed presentation is not uncommon. Male sex, older age, increased body weight, and presence of adhesions are additional risk factors. Accurate diagnosis may help streamline therapy and avoid unnecessary work-up.
TEACHING POINTS
Dropped gallstone is a known complication of laparoscopic cholecystectomy, especially in difficult cases.
The vast majority of gallstone spillage cases do not result in significant clinical complications.
When complications do arise, abscess formation and trocar site fistula are the most common complications of dropped gallstone.
A fluid collection or fistula tract containing a calcified or low-density focus should prompt consideration of dropped gallstone related complications.
MCQs
-
Dropped gallstone is more commonly seen with
Cholesterol stones
Laparoscopic approach for cholecystectomy
Pediatric or young adult patients
Patients with low body mass index
Answer Key: b
-
Dropped gallstones most commonly result in
No significant clinical sequel
Abscess formation
Fistula formation
Cholangitis
Answer Key: a
-
Spilled gallstone related complications are seen
Almost always within 1 week of cholecystectomy
Mostly around 1–2 month(s) of cholecystectomy
Up to 1 year following cholecystectomy
Any time after cholecystectomy, sometimes years later
Answer Key: d
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Epidemiology of gallbladder disease: Cholelithiasis and cancer. Gut Liver. 2012;6:172-87.
- [CrossRef] [PubMed] [Google Scholar]
- Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015;18:196-204.
- [CrossRef] [PubMed] [Google Scholar]
- Gallbladder and gallstone removal, open versus closed laparoscopy, and pneumoperitoneum. Am J Surg. 1993;165:497-504.
- [CrossRef] [PubMed] [Google Scholar]
- Spilled gallstones after laparoscopic cholecystectomy. A relevant problem? A retrospective analysis of 10,174 laparoscopic cholecystectomies. Surg Endosc. 1998;12:305-9.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term consequences of intraoperative spillage of bile and gallstones during laparoscopic cholecystectomy. J Gastrointest Surg. 1997;1:85-91. discussion 90-1
- [CrossRef] [PubMed] [Google Scholar]
- Pigment gallstones form as a composite of bacterial microcolonies and pigment solids. Ann Surg. 1987;206:242-50.
- [CrossRef] [PubMed] [Google Scholar]
- Spilled gall stones during laparoscopic cholecystectomy: A review of the literature. Postgrad Med J. 2004;80:77-9.
- [CrossRef] [PubMed] [Google Scholar]
- Consequences of lost gallstones during laparoscopic cholecystectomy: A review article. Surg Laparosc Endosc Percutan Tech. 2016;26:183-92.
- [CrossRef] [PubMed] [Google Scholar]
- Dropped gallstone mimicking retroperitoneal tumor 5 years after laparoscopic cholecystectomy posing a diagnostic challenge. Cureus. 2022;14:e31284.
- [CrossRef] [Google Scholar]
- Stones spilled during cholecystectomy: A long-term liability for the patient. Surg Laparosc Endosc. 1997;7:432-4.
- [CrossRef] [PubMed] [Google Scholar]







