Translate this page into:
Extensive calcified peritoneal carcinomatosis: An imaging awe
*Corresponding author: Aruna R. Patil, Department of Radiology, Apollo Hospitals, Bengaluru, Karnataka, India. dr.arunarpatil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil AR, Rao PK, Kini D, Shivakumar S, Madhurkar R. Extensive calcified peritoneal carcinomatosis: An imaging awe. Case Rep Clin Radiol. doi: 10.25259/CRCR_7_2025
Abstract
Peritoneal calcification can be due to various benign and malignant pathologies. Malignant calcifications are commonly due to serous adenocarcinomas either of ovarian or primary peritoneal origin. Nodular calcification favors neoplastic etiology, while benign calcifications are smooth and linear.
Keywords
Adenocarcinoma
Calcification
Computed tomography
Peritoneal carcinomatosis
INTRODUCTION
Extensive peritoneal calcification is a rare phenomenon and can be either metastatic or dystrophic. Malignant calcifications are secondary to serous adenocarcinomas of ovarian or primary peritoneal origin and intestinal mucinous neoplasms. The pattern of calcification on computed tomography (CT) can aid in differentiating benign from malignant causes. This case report highlights the characteristic imaging features of calcified peritoneal carcinomatosis.
CASE REPORT
A 71-year-old female presented to the gastroenterology outpatient department with abdominal distension and vague pain for several months. She denied a history of fever or weight loss. Relevant past history included hysterectomy and salpingo-oophorectomy 25 years back for unknown indications. On clinical examination, the abdomen was firm on palpation without tenderness. Abdominal radiograph showed multiple areas of ill-defined increased density obscuring normal bowel shadow and fat planes [Figure 1]. Contrast-enhanced computed tomography (CECT) was done for further evaluation. CT showed extensive confluent clumps of calcifications with mild heterogeneity (HU +400 to +600) in the entire abdomen with predilection for anterior, anterolateral portions of peritoneal cavity and pelvis conforming to omentum, paracolic gutters, and pouch of Douglas [Figure 2]. Multiple smaller calcific deposits were also noted along the subphrenic peritoneum, perihepatic, and perisplenic regions and abutting the serosal surface of the small and large bowel [Figure 3]. No evidence of bowel obstruction was noted. No obvious non-calcified masses were evident. Minimal perihepatic ascites was seen. Based on the imaging features, diagnosis of diffuse calcified peritoneal deposits was considered. Chronic granulomatous disease such as tuberculosis was a differential diagnosis. Upper and lower gastrointestinal endoscopy was negative for malignancy. Biopsy of the omentum and aspiration of the ascitic fluid was done. The ascitic fluid was hemorrhagic, rich in protein, and cellular with few atypical cells arranged in clusters. The atypical cells were round to cuboidal having vesicular nucleus with prominent nucleoli and a moderate amount of acidophilic cytoplasm. Few lamellated dystrophic calcification was seen along with plenty of reactive mesothelial cells, lymphocytes, and few macrophages against a hemorrhagic background. Omental biopsy showed cores of tumor tissue arranged in acinar and micropapillary pattern with low-grade nuclear morphology and extensive psammomatous calcifications [Figure 4]. On immunohistochemistry, the atypical cells were immunopositive for CK Cocktail - CK7, WT-1, PAX 8, and a few cells expressed p16. p53 showed wild type nuclear staining.
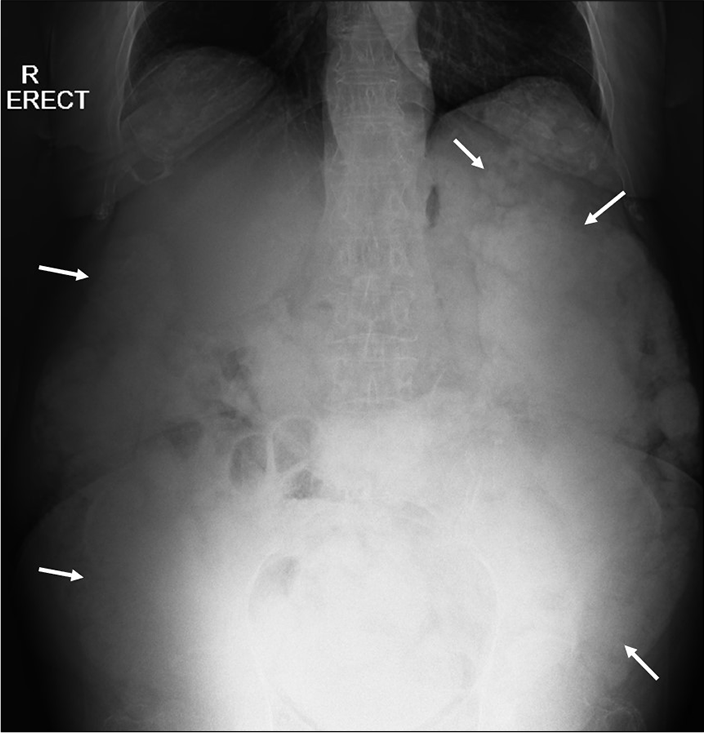
- Erect radiograph of the abdomen shows extensive confluent fluffy densities (white arrows) distributed predominantly in the lateral and the inferior aspect obscuring the normal bowel and solid organ shadows.

- (a and b) Axial contrast-enhanced computed tomography (CECT) sections in venous phase at the level of pelvis, mid abdomen in bone window shows extensive confluent calcific areas (HU: +400 to +600) predominantly involving the omentum, paracolic gutters and the pelvis (solid white arrows). (c) Axial CECT section in venous phase of upper abdomen in soft tissue window shows mild perihepatic ascites (dashed white arrow).

- Coronal sections of the (a and b) contrast-enhanced computed tomography abdomen in the venous phase bone window show extensive fluffy calcific areas conforming to peritoneal distribution (solid white arrows). Dashed arrows point to small calcific deposits in the subphrenic region.

- (a) Whole mount view (×2) shows cores of tumor tissue with calcifications. (b and c) Hematoxylin & Eosin (H&E) stain ×40 magnification shows tumor cells arranged in acinar (solid black arrow) and micropapillary (dashed black arrow) patterns with low-grade nuclear features along with psammomatous calcification (solid white arrow).
The cells were immunonegative for CK20, SATB2, calretinin, CK5/6, and CDX2 with Ki67 labeling index of 15%. Gene expert for tuberculosis was negative. The histopathological diagnosis was malignant calcified peritoneal deposits secondary to low-grade serous carcinoma of peritoneal origin/borderline serous tumor of ovarian origin. Clinically, the ovarian origin was favored due to relatively increased prevalence and prior history of pelvic surgery. The patient was advised palliative care.
DISCUSSION
Diffuse peritoneal calcification can be metastatic or dystrophic and is a result of several etiologies including tuberculosis, meconium peritonitis, pneumocystis infection, sclerosing or sterile peritonitis secondary to chronic dialysis, multiple surgeries, hyperparathyroidism, and calcified deposits.[1-3] Calcifications secondary to hypercalcemic state are metastatic whereas those secondary to infections, and neoplasms are dystrophic. The common neoplasms that can result in calcified peritoneal metastasis include serous ovarian cyst adenocarcinoma, and mucinous carcinomas of the stomach and intestine.[4-6] Calcification can also occur as a result of chemotherapy.[4] With regard to ovarian carcinoma, lower histopathological grades are associated with more bulky calcifications.[7] Calcifications are also noted to occur in primary peritoneal tumors such as papillary serous carcinoma and malignant mesothelioma.[2]
Among the imaging modalities, CT is the best investigation to detect peritoneal calcifications and characterize them. Ultrasound is not very reliable as small calcifications can be missed and extensive calcifications obscure further details.
The peritoneal calcifications secondary to tuberculosis are not extensive and can be associated with calcified or necrotic lymph nodes, ascites, and bowel thickening.[5]
Calcifications secondary to chronic dialysis are generally smooth and linear and tends to clump bowel loops resulting in cocoon formation[3] with or without obstructive features.
In general, linear and smooth calcifications are benign, and nodular and confluent calcifications are malignant.[1,3] Extensive nodular calcifications like our case can be confidently attributed to low-grade or borderline serous adenocarcinoma deposits of either primary peritoneal or ovarian origin.
DIFFERENTIAL DIAGNOSIS
The following Table 1 summarizes the differential diagnosis.
| Differential | Imaging features |
|---|---|
| Tuberculosis | Not extensive, small and patchy, associated calcified/low attenuating lymph nodes. Bowel thickening, ascites. |
| Chronic peritoneal dialysis | Smooth, linear calcification, sclerosing in nature forming cocoon or clumping of bowel loops. History of dialysis present. |
| Hypercalcemic states | More organ specific – renal, pancreatic, cutaneous, and intestinal. |
CONCLUSION
Extensive calcified peritoneal lesions especially when nodular in a female patient should raise suspicion of malignancy and worked up accordingly.
TEACHING POINTS
Peritoneal calcifications can be due to both benign and malignant processes.
Nodular clumps of calcification generally favors malignant etiology, whereas calcification in benign causes is smooth and linear.
Extensive nodular peritoneal calcifications are commonly deposits secondary to borderline serous adenocarcinoma of ovarian origin or primary low-grade serous carcinoma of peritoneal origin.
MCQs
-
All the below are causes for peritoneal calcification except:
Tuberculosis
Chronic peritoneal dialysis
Mucinous neoplasms
-
Hypoparathyroidism
Answer key: d
-
Which imaging modalities can pick up extensive peritoneal calcifications?
Radiographs
CT
Ultrasonography
-
All of the above
Answer key: d
-
All the below are causes for malignant peritoneal calcification except:
Serous ovarian adenocarcinoma
Hepatocellular carcinoma
Primary peritoneal serous carcinoma
-
Gastric mucinous neoplasms
Answer key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Severely calcified peritoneal metastases masquerading as retained barium on CT scan. BMJ Case Rep. 2015;2015:bcr2015211487.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive peritoneal calcification in a patient with serous borderline ovarian tumor. Available from: https://wwweuroradorg/case/16550 [Last accessed on 2025 Jan 02]
- [Google Scholar]
- Peritoneal calcification: Causes and distinguishing features on CT. AJR Am J Roentgenol. 2004;182:441-5.
- [CrossRef] [PubMed] [Google Scholar]
- CT imaging of peritoneal carcinomatosis with surgical correlation: A pictorial review. Insights Imaging. 2021;12:168.
- [CrossRef] [PubMed] [Google Scholar]
- Primary and secondary tumors of the peritoneum: Key imaging features and differential diagnosis with surgical and pathological correlation. Insights Imaging. 2023;14:115.
- [CrossRef] [PubMed] [Google Scholar]
- The perihepatic space: Comprehensive anatomy and CT features of pathologic conditions. Radiographics. 2007;27:129-43.
- [CrossRef] [PubMed] [Google Scholar]
- Significance of tumour calcification in ovarian carcinoma. Br J Radiol. 2009;82:640-4.
- [CrossRef] [PubMed] [Google Scholar]







