Translate this page into:
CT-peritoneography in diagnosis of patent processus vaginalis in peritoneal dialysis
*Corresponding author: S. Shanmuga Jayanthan, Department of Radiology, Meenakshi Hospital, Thanjavur, Tamil Nadu, India. jettan.32@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shanmuga Jayanthan S, Nadanasadharam K, Dwarak S, Annamalai PR. CT-peritoneography in diagnosis of patent processus vaginalis in peritoneal dialysis. Case Rep Clin Radiol. 2024;2:23-5. doi: 10.25259/CRCR_45_2023
Abstract
Patent processus vaginalis is a congenital condition characterized by persistent communication between the scrotum and peritoneal cavity which is associated with pathologies like congenital hydrocele/hernias. Asymptomatic patent processus vaginalis may become clinically evident in patients undergoing peritoneal dialysis, who may present with unilateral scrotal edema following dialysis. Conventional plain computed tomography (CT) may be difficult to identify the communication, especially if small, and in such cases, CT peritoneography will be useful to detect the patent processus vaginalis.
Keywords
Peritoneal dialysis
Computed tomography peritoneography
Patent processus vaginalis
INTRODUCTION
Diagnosis of peritoneal complications following peritoneal dialysis was done during the earlier periods around 1970s with the help of plain radiographs, contrast catheterograms, and peritoneographys.[1] However, these methods were inaccurate and misleading. Hence, they have been replaced with nuclear isotope scans (peritoneal scintigraphy), computed tomography peritoneography (CTP), and magnetic resonance peritoneography (MRP) using contrast/dye materials recently. Herein, we report a case of a 60-year-old male patient who presented with unilateral scrotal swelling following peritoneal dialysis and CTP was used to delineate the communication.
CASE REPORT
A 60-year-old male patient who was diagnosed with chronic kidney disease was undergoing regular cycles of peritoneal dialysis. He reported with complaints of the left scrotal swelling following dialysis which was increasing in size progressively. To detect any peritoneal defects, CTP was done. CTP coronal and volumetric reconstruction images demonstrated the communication between peritoneum and left hemi-scrotum [Figure 1a and b]. Surgical excision was planned and the patient was treated with lower dialysate volumes till then. Left patent processus vaginalis was confirmed intraoperatively [Figure 2], for which lichtenstein tension free hernioplasty was done.
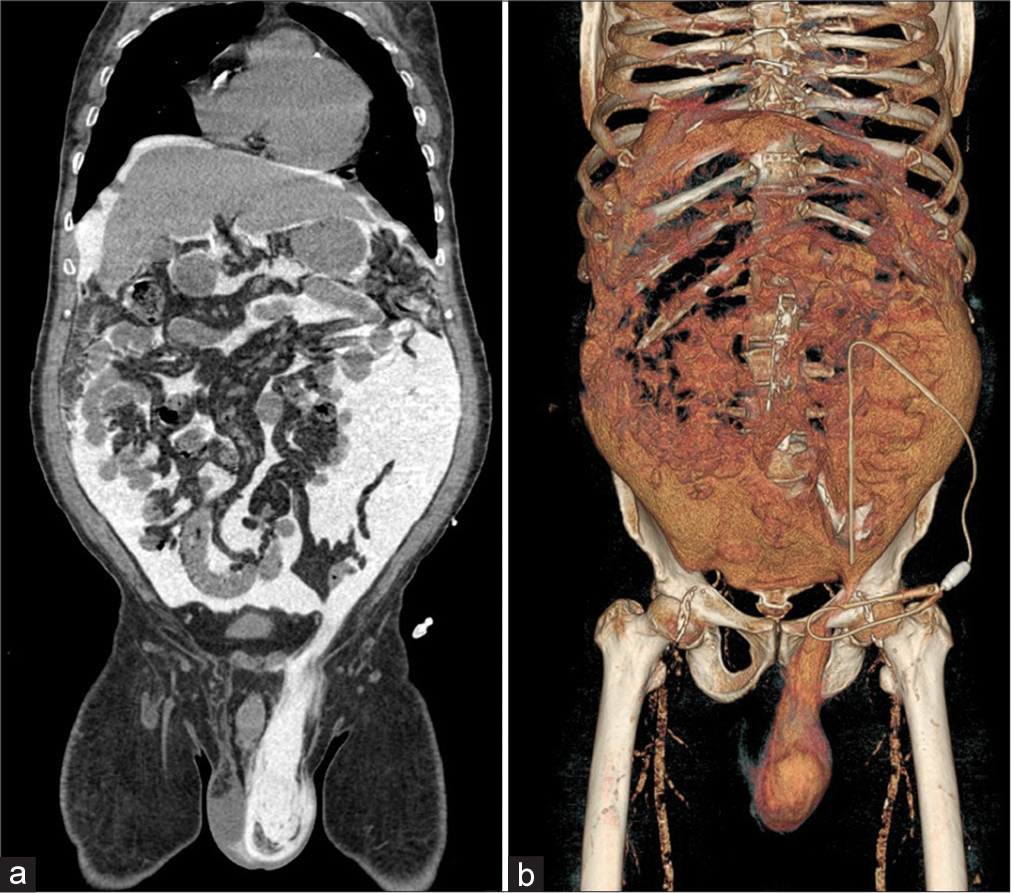
- (a) Computed tomography peritoneography (CTP) coronal image demonstrates communication between peritoneum and left hemiscrotum. (b) CTP volumetric reconstruction image demonstrates communication between peritoneum and left hemiscrotum.
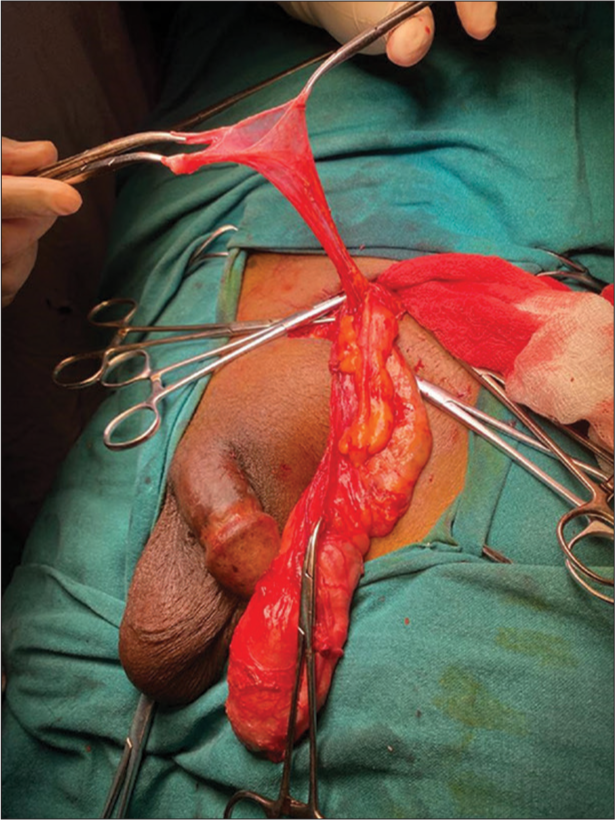
- Intraoperative image showing left patent processus vaginalis.
Technique
The peritoneal cavity is completely drained of dialysate, before performing this procedure. About 50 mL of non-ionic iodinated contrast is used for each 1 l of dialysis fluid. Appropriate volume should be administered in the above ratio and simultaneously oral or iv contrast can also be administered to diagnose any abscess or tumor, if needed. Scanning is initially performed with the patient in the supine position, 1 h post-contrast injection. Delayed scan, 4-h later, may be needed if the first scan is negative. Lateral decubitus or prone positions may be performed in selected cases. The contrast material dialysate mixture is drained at the end of the procedure.[2,3]
DISCUSSION
Continuous ambulatory peritoneal dialysis (CAPD) is a common alternative treatment to hemodialysis for endstage/chronic renal disease. The most common complication of CAPD is acute peritonitis.[4] CTP has an edge advantages over plain computed tomography (CT) in detecting some of the other complications associated with CAPD. Abdominal wall and inguinal hernias are other common complications; sometimes previously asymptomatic hernias are exacerbated following CAPD.
Localized genital edema can occur in 4–10% of CAPD patients[2] and the most common cause is inguinal hernia (10–15%).[2] Genital swelling without a palpable hernia is often a diagnostic dilemma. This can occur as a result of dialysate leak along the fascial planes, which could mimic the inguinal hernia or due to embryological defect like patent processus vaginalis. Diagnosis of these conditions is vital to avoid unnecessary surgery.[4]
Asymptomatic patent processus vaginalis can be seen in about 15–35% of adults.[2] It can present as inguinoscrotal swelling following dialysis in a previously asymptomatic individual.[4] Increase in intra-abdominal pressure following peritoneal dialysis is an important cause for leakage of dialysis fluid through acquired or congenital defect in abdominal wall or thorax. It can manifest as hydrothorax or genital/abdominal wall edema. Sometimes, the defect may be very small and may not be appreciated with routine CT. However, following increase in abdominal pressure during CTP can accurately elicit the defect.[4]
During the earlier periods around 1970s, these complications were diagnosed using plain radiographs, contrast catheterograms, and peritoneographys. However, these methods were obsolete and have been replaced nowadays with nuclear isotope scans (peritoneal scintigraphy), CTP, and MRP using contrast/dye materials.[1] Among these, CTP is the gold standard technique in accurate diagnosis of these conditions.[1,4,5]
CONCLUSION
CTP has an edge over conventional plain CT in detection of small defects, adhesions, loculated fluid collections, intra-abdominal abscesses, and pseudocysts with higher sensitivity and specificity.[5]
TEACHING POINTS
CT-peritoneography has high sensitivity and specificity compared to conventional CT in detection of complications associated with continuous ambulatory peritoneal dialysis.
Although patent processus vaginalis is rare, it should be kept in differentials for patients presenting with unilateral scrotal swelling, following continuous ambulatory peritoneal dialysis.
COMPLICATIONS OF CAPD
|
MCQs
-
How much amount of contrast is used in the procedure of CT-Peritoneography?
100 mL/L of dialysate
150 mL/L of dialysate
50 mL/L of dialysate
None of the above
Answer Key: c
-
Which of the following modalities have high sensitivity and specificity in diagnosis of patent processus vaginalis?
Non-contrast CT
CT-peritoneography
MRI
None of the above
Answer Key: b
-
Which of the following are not complications of peritoneal dialysis?
Acute peritonitis
Intra-abdominal abscess
Adhesions
Leakage of dialysis fluid
None of the above
Answer Key: e
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Genital edema in patients on continuous ambulatory peritoneal dialysis, Report of 3 cases and review of the literature. Am J Nephrol. 1986;6:471-5.
- [CrossRef] [PubMed] [Google Scholar]
- Patent processus vaginalis in peritoneal dialysis. Kidney Int. 2013;84:628.
- [CrossRef] [PubMed] [Google Scholar]
- Computerized tomography with and without intraperitoneal contrast for determination of intraabdominal fluid distribution and diagnosis of complications in peritoneal dialysis patients. ASAIO Trans. 1990;36:95-103.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of continuous ambulatory peritoneal dialysis: Evaluation with CT peritoneography. AJR Am J Roentgenol. 1992;159:983-9.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness and safety of computed tomographic peritoneography and video-assisted thoracic surgery for hydrothorax in peritoneal dialysis patients: A retrospective cohort study in Japan. PLoS One. 2020;15:e0238602.
- [CrossRef] [PubMed] [Google Scholar]







