Translate this page into:
A rare case of a huge diffuse-type tenosynovial giant cell tumor in the ankle
*Corresponding author: Riya Samanta, Department of Radiology, Mahajan Imaging, Safdarjung Hospital Sports Injury Centre, New Delhi, India. samanta.ria1011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Samanta R, Batta NS, Abhinetri K. A rare case of a huge diffuse-type tenosynovial giant cell tumor in the ankle. Case Rep Clin Radiol. 2024;2:31-5. doi:10.25259/CRCR_101_2023
Abstract
Tenosynovial giant cell tumor (TSGCT) is a rare tumor originating from the synovial lining of joints, tendon sheaths, and bursae. It is categorized into localized and diffuse types. The diffuse-type TSGCT (D-TSGCT), formerly called pigmented villonodular synovitis, although benign, can be locally aggressive. Magnetic resonance imaging is the modality of choice for diagnosing and assessing the severity of the disease. The lesions demonstrate characteristic “blooming” on gradient echo sequences. Histopathology reveals villous, nodular, or villonodular components and hemosiderin deposition. Here, we report the case of a 28-year-old man with a huge D-TSGCT in the left ankle.
Keywords
Diffuse-type tenosynovial giant cell tumor
Ankle
Tendon sheath
Pigmented villonodular synovitis
INTRODUCTION
Tenosynovial giant cell tumor (TSGCT) is a rare benign neoplasm originating from the synovial lining of joints, tendon sheaths, and bursae. The occurrence of TSGCT in the ankle and foot is much less frequently reported compared to that of the upper extremity and knee, and a previous study has reported an incidence of only 3–5% in the ankle and foot.[1] It has been thought to be a result of inflammation secondary to chronic antigenic stimulation, reactive synovial proliferation, or a lesion of macrophage/monocyte derivation.[2] Radiographic features are often non-specific. Magnetic resonance imaging (MRI) manifestations are frequently characteristic of the lesions which display low signal intensity on all pulse sequences. Gradient echo (GRE) pulse sequences enable confirmation of the presence of hemosiderin, which shows prominent “blooming” due to magnetic susceptibility artifact. MRI is optimal for evaluating the extent of the disease which is necessary for guiding treatment.[3] Based on the biological behavior, it has further been classified as localized (L-TSGCT) and diffuse (D-TSGCT), the latter being more aggressive.[3] The literature on D-TSGCT arising from the ankle is sparse, and the cases documented till date have shown a relatively limited extent of the disease process. We present a rare case of a very large D-TSGCT in the ankle with extensive involvement of the synovial lining of the ankle joint and the tendon sheaths.
CASE REPORT
A 28-year-old male presented with progressive swelling for 2 years along the medial and lateral aspects of the left ankle and a dull aching pain without any previous history of trauma. He had symptomatic improvement in pain with analgesics. Clinically, he was found to have a diffuse, lobulated, firm, and non-tender soft-tissue mass at the ankle [Figure 1]. There was a minimal limitation of motion. Mildly prominent and tortuous subcutaneous vessels were noted medially. The temperature and color of the overlying skin were normal. Plain radiograph [Figure 2] of the left ankle revealed lobulated periarticular soft-tissue masses with few calcific foci posteromedially. Extrinsic pressure erosions of the dorsal talar neck, plantar aspect of the anterior calcaneum, and distal fibula were present. The bone density and joint spaces were preserved. Ultrasonography (USG) [Figure 3] revealed multiple globular heterogeneous hypoechoic masses in multiple compartments about the ankle joint in close relation to the tendons in the flexor, extensor, and peroneal compartments. Many of these lesions were completely encasing the tendons and grew between the tendon and the underlying bone. Color Doppler flow imaging (CDFI) did not demonstrate appreciable internal vascularity. The lesions did not move with the tendons on dynamic sonography. MRI of the ankle [Figure 4] was subsequently performed which revealed an extensive globular mass like synovial proliferation at the ankle joint showing multiple T1 isointense and T2 hypointense nodules with blooming artifact on gradient images suggesting the presence of hemosiderin. The nodules were extending into the talocrural, retrocalcaneal and dorsal talonavicular spaces, the sinus tarsi and along the plantar aspects of tarsals and metatarsal bases. The lesions were seen along the tendon sheaths; almost completely enveloping multiple tendons at the flexor, extensor, and peroneal compartments; and causing multiple pressure erosions at the distal tibia, fibula, lateral talar dome, talar neck, calcaneum, navicular base, and other tarsal bones. Multifocal bone marrow edema was present with preservation of joint space and no intraosseous extension. Microscopic examination of excision biopsy of a single globular soft tissue revealed a partially circumscribed, lobulated mass with the presence of numerous multinucleated giant cells, round-to-oval eosinophilic mononuclear cells, chronic inflammatory cells, few xanthoma cells, and hemosiderin in a collagenous background confirming the diagnosis of (D-TSGCT).

- (a and b) A 28-year-old man with diffuse-type tenosynovial giant cell tumor who presented with progressive left ankle swelling for 2 years. Clinical photographs showing swelling over the lateral aspect of the distal leg (black arrow) and medial and lateral aspects of the left ankle (arrowheads). Prominent and tortuous subcutaneous vessels (white arrow).
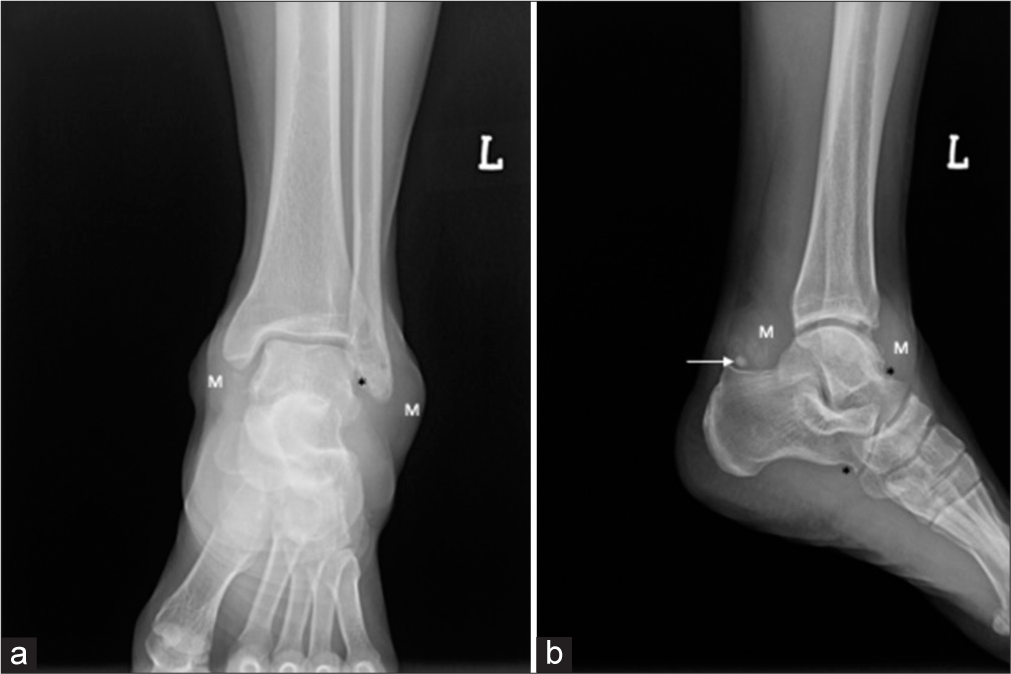
- A 28-year-old man with diffuse-type tenosynovial giant cell tumor who presented with progressive left ankle swelling for 2 years. X-ray of the left ankle in the anteroposterior (a) and lateral views (b) showing lobulated periarticular soft-tissue masses (M) with few calcific foci posteromedially (arrow) and extrinsic erosions/scalloping (asterisk) of the dorsal talar neck, plantar aspect of the anterior calcaneum, and distal fibula.
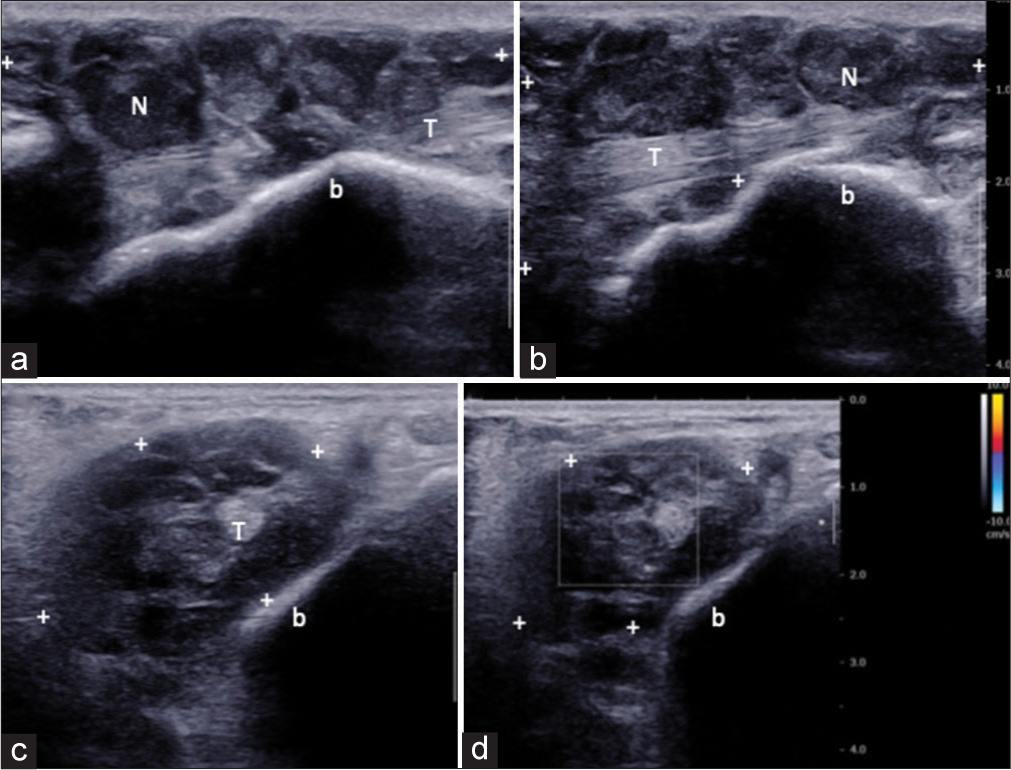
- A 28-year-old man with diffuse-type tenosynovial giant cell tumor who presented with progressive left ankle swelling for 2 years. Ultrasonography of the left ankle. Longitudinal (a and b) and transverse (c and d) sonograms along the posteromedial aspect of the ankle (flexor compartment) showing globular heterogeneous mass (cursors “+”) with numerous hypoechoic nodules (N) completely encasing the tendon (T) of flexor hallucis longus and present between the tendon and the underlying bone (b). Color Doppler flow imaging (d) not showing appreciable internal vascularity.
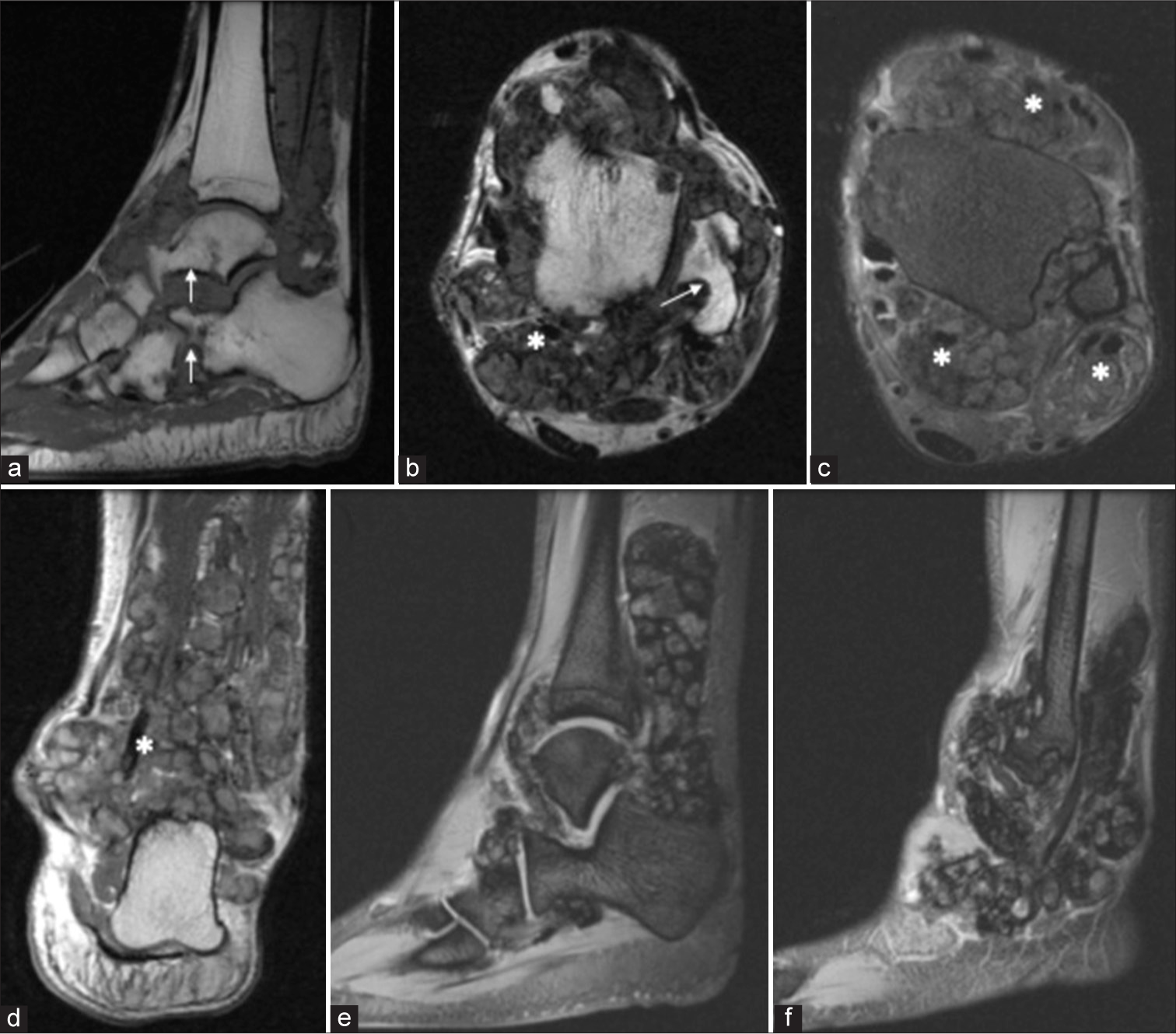
- A 28-year-old man with diffuse-type tenosynovial giant cell tumor who presented with progressive left ankle swelling for 2 years. MRI of the left ankle. (a) Sagittal T1-weighted image, (b) Axial T2-weighted image, axial and coronal proton density (PD)-weighted image (c and d) showing an extensive globular mass like synovial proliferation with multiple T1 isointense and T2/PD hypointense nodules along the bursae, recesses, and tendon sheaths causing extrinsic pressure erosions of multiple bones (white arrow) and encasing multiple tendons (asterisk). Gradient recalled echo images (e and f) showing characteristic “blooming artifact” confirming the presence of hemosiderin deposition.
DISCUSSION
TSGCTs are rare, slow-growing, non-tender, benign soft-tissue tumors of the extremities, which are more common in the upper extremity, but very rarely seen in the ankle and foot.[2] They originate from the synovial lining of joints, tendon sheaths, and bursae.[4] The usual presentation is that of a slow-growing firm mass in the vicinity of a joint which may be associated with pain and limitation of joint movement. The etiopathogenesis involves both neoplastic and inflammatory components. Based on its growth pattern, it can be classified as L-TSGCT or D-TSGCT, the latter being rarer with an incidence rate of 5 per million and more aggressive nature with frequent recurrences after excision (14–55%).[4,5] The L-TSGCT is most prevalent and usually follows an indolent course, frequently affecting the joints of the hands. D-TSGCT, formerly known as pigmented villonodular synovitis, on the contrary, is much less common and affects the knee joint most commonly followed by the hip or shoulder.[6]
Radiographic appearances are variable and typically reveal a soft-tissue mass in 50–70% of cases. Osseous abnormalities are seen in 15–25% of the cases, with extrinsic erosions of the underlying bone being the most common abnormality.[3] Other common radiographic features are normal bone mineralization, preserved joint space, and the absence of calcification.[3] USG may show joint effusion, complex heteroechoic masses, and hypoechoic thickened synovium. The hypoechoic solid masses in D-TSGCT usually show well-defined margins and are intimately related to/encase the involved tendon. However, as D-TSGCT has its origin from the tendon sheath, dynamic USG shows the absence of movement of the lesion with the tendon.[3] CDFI usually depicts increased blood flow in the lesions, although, in our case, internal vascularity was not appreciable. USG also helps in determining vascularity and guiding biopsies from the lesions. Computed tomography (CT) depicts soft-tissue thickening about the joint which may have slightly increased attenuation relative to that of muscle reflecting hemosiderin deposition. The extension of the lesion is not clearly depicted on CT owing to its limited contrast resolution; however, it is optimal for demonstrating osseous erosions.[3]
Although TSGCT rarely involves the ankle and foot, it is very important to consider it as a differential diagnosis for soft-tissue tumors in this region. In addition to TSGCT, differential diagnosis of soft-tissue tumors in the ankle and foot may consist of synovial cyst, lipoma, tendon sheath fibroma, synovial hemangioma, undifferentiated pleomorphic sarcoma, leiomyosarcoma, and synovial sarcoma.[1] MRI has been known to be effective in differentiating TSGCT from other soft-tissue tumors in the ankle and foot.
MRI is the modality of choice for diagnosing and assessing the severity of D-TSGCT. The MRI appearance is characteristic of the lesions which demonstrate prominent “blooming” on GRE sequences confirming the presence of hemosiderin. This feature is not seen in other T2 hypointense masses like tendon sheath fibroma.[3,7] Another lesion that may mimic TSGCT on MRI is synovial osteochondromatosis; however, it can be differentiated from the latter on the basis of plain radiographs that show numerous intra-articular calcified and ossified loose bodies in synovial osteochondromatosis. Calcification is very rare in TSGCT and is present in only 6% of cases.[3]
MRI also gives a preoperative map prior to synovectomy, the cornerstone of treatment for D-TSGCT. Finally, with the advent of CSF 1-receptor inhibitors, a novel therapy for patients with tumor relapse or inoperability, MRI plays a key role in assessing treatment response as well as in follow-up imaging in recurrence of D-TSGCT.[4]
DIFFERENTIAL DIAGNOSIS
Differential diagnosis for synovial masses [Table 1].
| S. No. | Differential diagnosis | Differentiating features |
|---|---|---|
| 1. | Tendon sheath fibroma | • No blooming on GRE pulse sequence |
| 2. | Synovial osteochondromatosis | • Calcifications are present (seen on radiographs) • No blooming on GRE pulse sequence (unless there is intra-articular hemorrhage) |
| 3. | Synovial hemangioma | • Soft-tissue mass isointense to skeletal muscle on T1-weighted images • Phleboliths can be seen on radiographs |
| 4. | Synovial sarcoma | • Arise near the joints and rarely from the joint itself. Despite their name, they do not arise from synovial structures (joints, bursae, and tendon sheaths) • Calcifications are common • Direct bone invasion can be seen with aggressive features (geographic, permeative, or moth-eaten appearances) |
| 5. | Undifferentiated pleomorphic sarcoma | • Tumor of the soft tissues • May rarely arise from the bone in case of which it appears as an aggressive destructive bony lesion with or without calcifications |
GRE: Gradient echo
CONCLUSION
D-TSGCT is a very rare neoplasm in the ankle and foot and should be taken into consideration as a differential diagnosis for soft-tissue tumors in this region. MRI plays a pivotal role in diagnosing the disease and assessing its extent, thus enabling clinicians for optimal treatment planning. MRI appearances are characteristic of the lesions which display low signal intensity on all pulse sequences. Prominent “blooming” within the lesions from hemosiderin deposition on GRE pulse sequences is virtually pathognomonic of this disease.
TEACHING POINTS
D-TSGCT is a very rare neoplasm of the ankle and foot characterized by irregular synovial proliferation infiltrating the tendon sheaths and bursae, encasing the tendons.
T2 hypointense lesions on MRI with “blooming” from hemosiderin deposition on GRE images are virtually pathognomonic of this disease.
MRI plays a key role in diagnosis, preoperative planning, assessment of response to systemic treatment as well as follow-up of recurrent tumors.
MCQs
-
The imaging modality of choice for diagnosing TSGCT is
Plain X-ray
CT
Ultrasonography
Magnetic resonance imaging
Answer Key: d
-
D-TSGCT is histologically identical to
Fibroma of tendon sheath
PVNS
Synovial osteochondromatosis
Synovial sarcoma
Answer Key: b
-
True about TSGCTs are all except-
Preserved bone density
Extrinsic pressure erosions of the underlying bones
Permeative bone destruction and loss of joint space
Hemosiderin deposition
Answer Key: c
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Giant cell tumor of the tendon sheath originating from the ankle capsule: A case report and literature review. Oncol Lett. 2016;11:3461-4.
- [CrossRef] [PubMed] [Google Scholar]
- Giant cell tumor of the tendon sheath around the foot and ankle: A report of three cases and a literature review. J Am Podiatr Med Assoc. 2015;105:249-54.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented villonodular synovitis: Radiologicpathologic correlation. Radiographics. 2008;28:1493-518.
- [CrossRef] [PubMed] [Google Scholar]
- MRI of diffuse-type tenosynovial giant cell tumor in the knee: A guide for diagnosis and treatment response assessment. Insights Imaging. 2023;14:22.
- [CrossRef] [PubMed] [Google Scholar]
- Tenosynovial giant cell tumor in the foot and ankle. Foot Ankle Surg. 2020;26:712-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diffuse giant cell tumors of the tendon sheath in temporomandibular joint: Two case reports and review of the literature. Medicine (Baltimore). 2018;97:e11101.
- [CrossRef] [PubMed] [Google Scholar]
- Common soft tissue tumors involving the hand with histopathological correlation. J Clin Imaging Sci. 2019;9:15.
- [CrossRef] [PubMed] [Google Scholar]







