Translate this page into:
“Sun-ray” periosteal reaction in the calvarium – uncommon presentation of a common disease
*Corresponding author: Malvika Gulati, Department of Radiology, Indraprastha Apollo Hospitals, New Delhi, Delhi, India. drmalvikagulati@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gulati M, Goyal N, Baweja P, Ghonge N. “Sunray” periosteal reaction in calvarium – uncommon presentation of a common disease. Case Rep Clin Radiol. doi: 10.25259/CRCR_193_2023
Abstract
Meningiomas usually present with vague neurological symptoms or are incidentally detected on imaging. Radiologists are aware of the classical imaging picture of this entity comprising of enhancing extra-axial mass with associated hyperostosis. However, the presence of an aggressive sunburst type of periosteal reaction in a primary intra-osseous osteolytic meningioma, along with an extra-axial soft tissue as seen in our case has not been described previously in the literature.
Keywords
Calvarial meningioma
Intraosseous osteolytic meningioma
Sunburst periosteal reaction
Sunray periosteal reaction
Atypical meningioma
INTRODUCTION
Meningiomas constitute nearly a third of all brain neoplasms presenting most commonly in the fourth–fifth decade of life. They are often asymptomatic masses, however, they may present with vague symptoms. In majority of the cases, imaging shows enhancing extra-axial mass with associated features such as dural tail and bony hyperostosis which clinch the diagnosis and are typical of a classical meningioma.[1] However, atypical radiological features rarely complicate the imaging picture. Primary intraosseous osteolytic meningioma is a rare subtype constituting <2% of cases of meningiomas and is extradural arising within the bone thus, often being confused with primary bone tumors. These extradural meningiomas are more likely to display atypical imaging features and aggressive pathology.
CASE REPORT
A 55-year-old lady of African ethnicity presented with headache and a gradually progressive left scalp swelling for 4 months. No antecedent history of trauma or fever was present and the patient was well preserved otherwise.
On examination, a large firm-to-hard swelling was present over the left parietal region close to the vertex. The overlying skin and scalp hair were intact without any evidence of ulceration or local skin changes.
Skull radiograph showed areas of moth-eaten lytic destruction of the left parietal bone with associated sunburst type of periosteal reaction and the presence of a large soft-tissue component [Figure 1]. Contrast-enhanced magnetic resonance imaging (MRI) of the brain corroborated the findings of the osteolytic lesion and extensive spiculated sunburst type of periosteal reaction with new bone formation along the extracranial aspect of the lesion. The mass appeared isointense on T1-weighted imaging (T1WI) and T2-weighted imaging (T2WI) with strong diffusion restriction on diffusion-weighted images with an apparent diffusion coefficient value of 0.93 × 10−3 mm2/s. The periosteal reaction was particularly well seen on susceptibility-weighted images. In addition, a large, avidly enhancing extraosseous soft-tissue solid mass was present on both sides of the skull. The intracranial component measured 8.6 × 6.5 cm and showed a significant mass effect with gliosis and edema in the underlying left parietal parenchyma [Figure 2]. Differentials considered were calvarial intraosseous hemangioma, osteosarcoma, and osteoblastic metastasis. Gross primary resection of the tumor was done by a left parietal craniotomy with negative margins and the post-operative computed tomography (CT) scan revealed no residual mass. The patient did not require any adjuvant therapy and is doing well in 6-month follow-up.

- (a) Xray skull AP and (b) lateral shows areas of moth-eaten lytic destruction of left parietal bone with sunburst type of periosteal reaction. A large soft tissue component is seen overlying these bony changes without any foci of calcification or ossification.
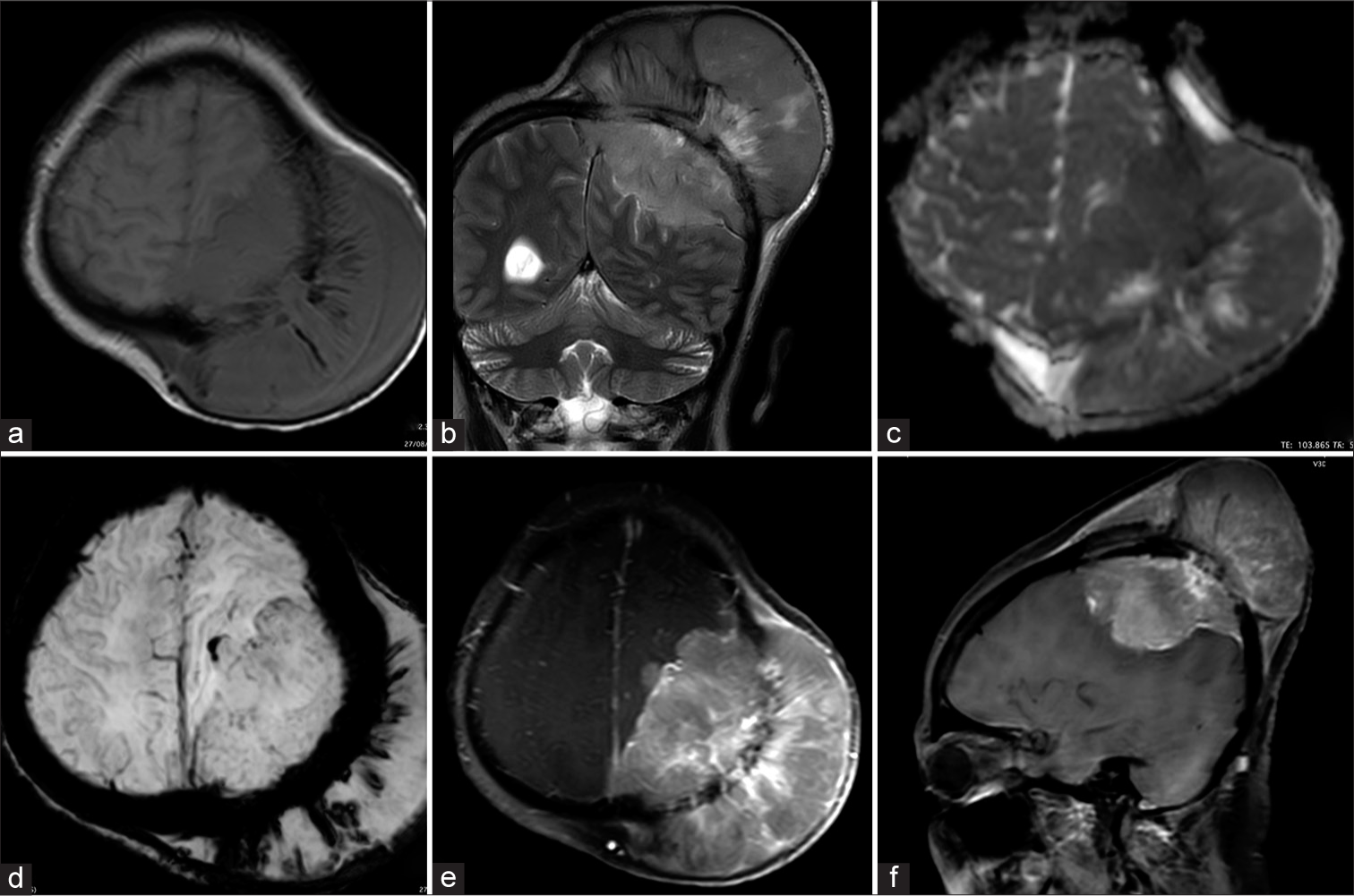
- Magnetic resonance imaging (MRI) shows an area of marrow signal alteration in the left parietal bone with a large extraosseous soft-tissue mass having an extradural component. The patient had presented with the large scalp component of the mass. (a) The mass is isointense on T1WI, (b) hyperintense on T2WI and (c) shows diffusion restriction. Extensive spiculated sunburst type of periosteal reaction with new bone formation is seen along the extracranial aspect of the lesion. (d) Susceptibility weighted imaging (SWI) images shows the periosteal reaction very well. (e, f) On post contrast intense heterogeneous enhancement of the lesion is seen.
Histopathology of the mass showed proliferation of spindle cells with syncytial and whorling patterns at places with few psammoma bodies with areas of increased cellularity. On immunohistochemistry, strong patchy cells were positive for EMA and PR and negative for GFAP, STAT6, and S100. Ki67 proliferative index is 20–25% in hot spot areas. The final diagnosis favored an atypical meningioma [Figure 3].
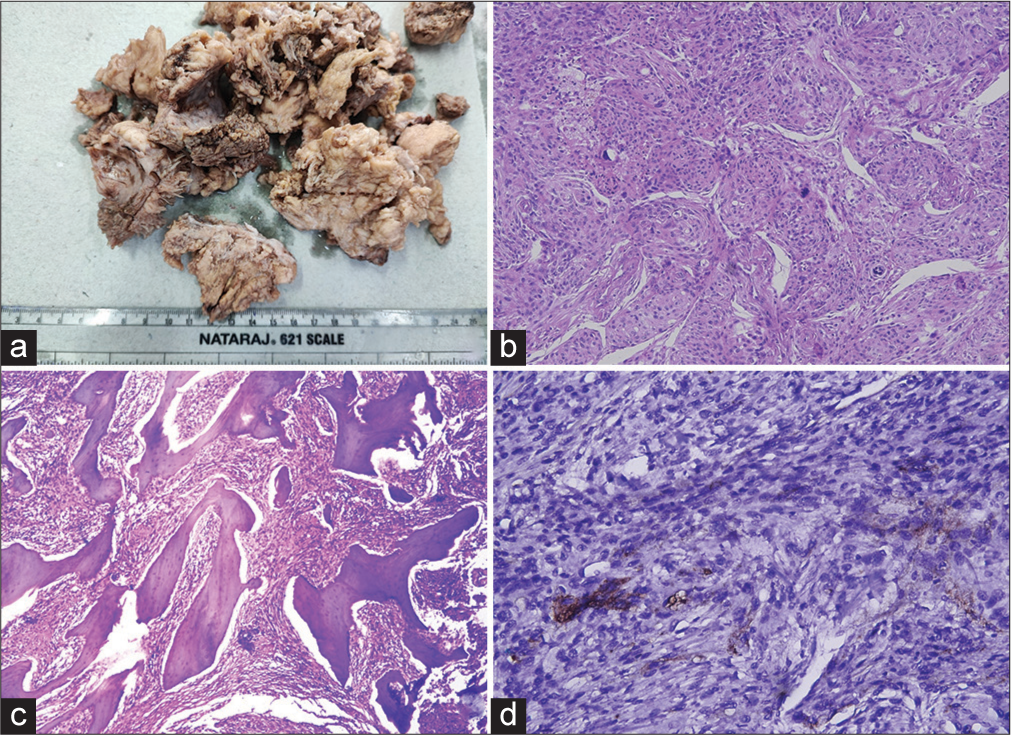
- (a) Grossly the tumor was tan-grey and predominantly solid. (b) Sections (200x) show proliferation of spindle cells with syncytial and whorling pattern at places. Few psammoma bodies seen. 4 to 5 mitotic figures noted /10 high power fields. Focal patchy areas of increased cellularity, small cells with high nuclear-cytoplasmic (N/C) ratio, large and prominent nucleoli, patternless or sheet-like growth (loss of lobular architecture) and foci of spontaneous or geographic necrosis noted. (c) Few bone bits noted with adhered and entrapped tumor tissue (100x). (d) On immunohistochemistry (200x), strong patchy cells were positive for EMA and PR, negative for GFAP, STAT6, S100. Ki67 proliferative index is 20-25% in hot spot areas. The final histopathological diagnosis favoured an atypical meningioma (WHO grade 2).
DISCUSSION
Majority of meningiomas arise from the arachnoid cap cells of the dura mater and show classical imaging features, and bony changes such as hyperostosis or direct invasion of the bone are described in atypical and higher-grade tumors. Primary intraosseous meningiomas are a subtype of primary extradural meningiomas and are rare in occurrence. Even among these, only a small number of cases show both aggressive imaging features and atypical pathological features. The various bony changes described constitute osteolysis and sclerosis. However, the spiculated sunburst type of periosteal reaction seen in our case is atypical for a meningioma. To the best of our knowledge, this is the first report of such a pattern of bony reaction in meningiomas. Due to such an extensive aggressive type of periosteal reaction, the imaging differentials considered were intraosseous hemangioma and bone-forming tumors such as metastasis, osteosarcoma, and more than a meningioma [Table 1].
| Calvarial hemangioma | Intradiploic expansile lesions, thin sclerotic rim, sunburst type of trabecular thickening |
| Meningioma | Extradural mass with bony hyperostosis, rarely aggressive type of periosteal reaction |
| Osteosarcoma | <1% of total osteosarcomas. Soft-tissue mass present. New bone formation and aggressive periosteal reaction |
| Metastasis | Known primary, multiplicity of lesions |
Calvarial hemangiomas are characteristically intradiploic expansile lesions with thin sclerotic rims. They show a sunburst type of trabecular thickening that radiates from a central point. Often, there may be areas of cortical breach with bony trabeculae growing beyond the cortex simulating an aggressive tumor.[2-4]
Calvarial osteosarcoma is a rare entity comprising <1% of total osteosarcoma cases. Few case reports describe this entity, which on imaging appears as a calvarial-based soft-tissue lesion with external and internal components. New bone formation and sunburst type of aggressive periosteal reaction are seen.
However, one should be vary to not confuse this “sunburst periosteal reaction” with the sunburst sign described in T2-weighted or post-contrast MRI or angiography. In this, the dural vessels are seen to diverge radially into the meningioma when viewed from the side.[5-8]
These primary intraosseous meningiomas most commonly present as a gradually increasing scalp mass. On imaging, they are bone based rather than being “dural based” as described for classical meningiomas.[9] There is bony erosion with areas of osteolysis and the presence of scalp and intracranial soft-tissue components. Dural and soft-tissue invasion may be coexisting. They typically appear as avidly enhancing masses having isointense signals on T1WI and T2WI. 68Ga DOTATEC positron emission tomography/CT has been used for diagnosis, radiotherapy response assessment, and detection of recurrence of extradural meningiomas.[10,11]
The management of choice is gross tumor excision with or without adjuvant radiotherapy.
This case emphasizes that even in the presence of a sunray type of periosteal reaction in the calvarium, meningioma should be kept as one of the differential diagnoses.
CONCLUSION
Meningiomas are the most common brain tumors and have typical imaging features. However atypical features like sunray type of periosteal reaction and large extraaxial soft tissue components can also be seen in some cases and meningioma should be a consideration if such features are seen.
TEACHING POINTS
Even in the presence of a sunray type of periosteal reaction in the calvarium, meningioma should be kept as one of the differential diagnoses.
Other rarer differential diagnosis of the sunray type of periosteal reaction in the calvarium includes hemangioma, osteosarcoma, and metastasis.
MCQs
-
What are the types of bony changes in meningiomas? (multiple options can be correct)
Hyperostosis
Osteolysis
Sunray type of periosteal reaction
None of the above
Answer key: a, b, c
-
Which nuclear medicine study is recommended for detection of extradural meningioma?
68Ga DOTATOC PET/CT
Sestamibi scan
Bone scan
None of the above
Answer key: a
-
What is the treatment of choice for intraosseous meningiomas?
Gross tumor resection
Chemotherapy
Conservative
Radiotherapy only
Answer key: a
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Magnetic resonance imaging of meningiomas: A pictorial review. Insights Imaging. 2014;5:113-22.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of skull vault tumors in adults. Insights Imaging. 2020;11:23.
- [CrossRef] [PubMed] [Google Scholar]
- Classic imaging features of calvarial hemangioma-a case report. Egypt J Radiol Nucl Med. 2018;49:663-5.
- [CrossRef] [Google Scholar]
- Hemangiomas in the calvaria: Imaging findings. AJR Am J Roentgenol. 1995;164:683-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dural masses: Meningiomas and their mimics. Insights Imaging. 2019;10:11.
- [CrossRef] [PubMed] [Google Scholar]
- Role of intratumoral flow void signs in the differential diagnosis of intracranial solitary fibrous tumors and meningiomas. J Neuroradiol. 2016;43:325-30.
- [CrossRef] [PubMed] [Google Scholar]
- Variants of meningiomas: A review of imaging findings and clinical features. Jpn J Radiol. 2016;34:459-6.
- [CrossRef] [PubMed] [Google Scholar]
- Primary osteolytic intraosseous atypical meningioma with soft tissue and dural invasion: Report of a case and review of literatures. J Korean Neurosurg Soc. 2014;56:509-12.
- [CrossRef] [PubMed] [Google Scholar]
- 68Ga DOTATOC PET/CT follow up after single or hypofractionated gamma knife ICON radiosurgery for meningioma patients. Brain Sci. 2021;11:375.
- [CrossRef] [PubMed] [Google Scholar]
- Primary intraosseous osteolytic meningioma with aggressive clinical behaviour: Clinicopathologic correlation and proposed new clinical classification. Life (Basel). 2022;12:548.
- [CrossRef] [PubMed] [Google Scholar]







