Translate this page into:
Diffuse cerebral microhemorrhages in Wiskott-Aldrich syndrome – A rare radiological manifestation of a rare immunodeficiency disorder
*Corresponding author: Kavan Ashesh Parikh, Department of Radio Diagnosis, B J Medical College, Ahmedabad, Gujarat, India. kavanparikh26@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Parikh KA. Diffuse cerebral microhemorrhages in Wiskott-Aldrich syndrome – A rare radiological manifestation of a rare immunodeficiency disorder. Case Rep Clin Radiol. doi: 10.25259/CRCR_11_2024
Abstract
Wiskott-Aldrich syndrome (WAS) is a rare X-linked primary immunodeficiency disorder with the characteristic triad of immunodeficiency, thrombocytopenia, and eczema. It results from a genetic mutation in the gene encoding WAS protein. We present a case of a 4-year-old male child who presented with two episodes of generalised tonic clonic seizures (GTCS) type convulsions. Magnetic resonance imaging (MRI) brain with contrast revealed diffuse cerebral microhemorrhages in supratentorial and infratentorial brain parenchyma which is a rare manifestation and not adequately documented in literature to the best of our knowledge.
Keywords
Wiskott-Aldrich syndrome
Immunodeficiency
Thrombocytopenia
Microhemorrhages
Eczema
INTRODUCTION
Wiskott-Aldrich syndrome (WAS) is a rare X-linked recessive disorder caused by abnormal number and function of anti-inflammatory myeloid and lymphoid lineage cells. The incidence of WAS is around 1 in 100000 live births. WAS has a wide clinical spectrum ranging from mild, isolated thrombocytopenia to life-threatening hemorrhage, immunodeficiency with severe infections, eczema, autoimmunity, and malignancy. Neurological manifestations are rarely reported in these patients and the underlying etiologies are not well established. Brain imaging by magnetic resonance imaging (MRI) can be helpful in identifying secondary implications of thrombocytopenia like microhemorrhages and large intraparenchymal bleeds or rarely, secondary malignancies like lymphomas.
CASE REPORT
A 4-year-old male patient presented to our department with a history of episodes of generalised tonic clonic seizures (GTCS) type convulsions in 24 h. Each episode lasted for 4–5 min and was followed by loss of consciousness for next 30 min. There was no associated history of fever, vomiting, headache, neck rigidity, or trauma. Birth history of the patient was insignificant. There was history of pulmonary tuberculosis (TB) 7 months back for which 6 months of anti-tubercular therapy (ATT) was administered, and subsequently, the patient was sputum negative for TB. The patient had frequent complaints of infections since the age of 2 years for which bone marrow biopsy was done in 2022 which revealed immune thrombocytopenia. Clinically, the patient had eczema around angle of mouth and multiple purpuric lesions over abdomen and lower limbs [Figure 1]. Laboratory investigations of the patient revealed markedly elevated immunoglobulin (Ig)E levels (>2500 IU/mL), elevated IgA and IgG levels, cytoplasmic staining of antinuclear antibody on indirect immunofluorescence, and pancytopenia on hemogram. Based on clinical and laboratory findings, diagnosis of Wiskott-Aldrich syndrome (WAS) was made.

- Clinical images of the patient showing perioral eczema and purpuric skin hemorrhages on abdomen and lower limbs.
MRI brain with contrast was performed on Siemens 1.5T MRI machine which revealed diffuse varying sized foci of susceptibility artifacts (blooming) in random distribution on susceptibility-weighted images. These foci were hypointense on magnitude images and bright on phase images – suggestive of blood products (in accordance with the “left-handed” system used by Siemens) [Figure 2]. Few of these foci appeared hypointense on T2/fluid-attenuated inversion recovery images [Figure 3]. There was involvement of both cerebral hemispheres, corpus callosum, midbrain, and both cerebellar hemispheres. On computed tomography correlation, few of these foci corresponded to small foci of hemorrhages.
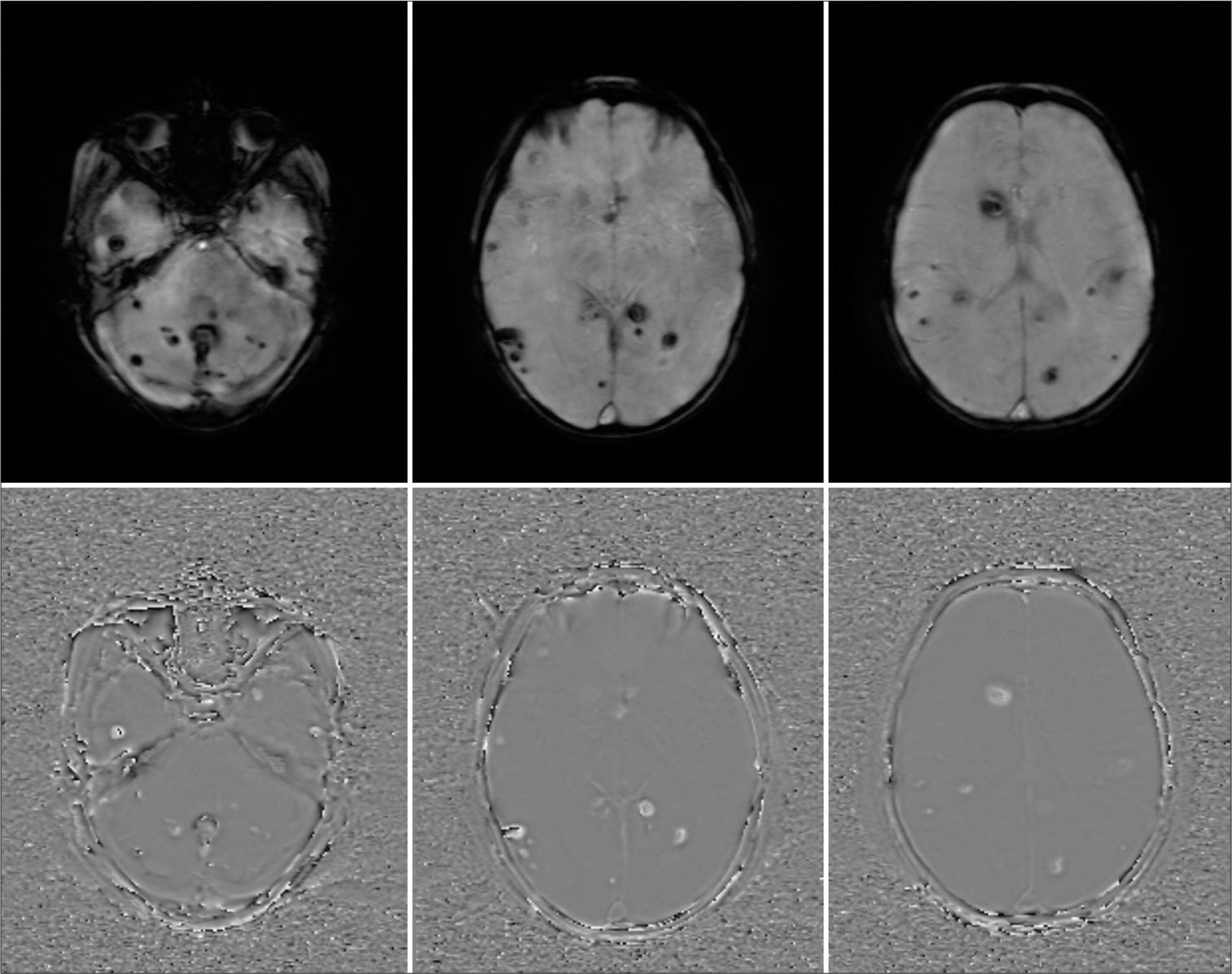
- Representative axial sections of magnitude (top row) and phase (bottom row) images at different levels showing multiple foci of blooming corresponding to microhemorrhages.

- Representative axial sections of T2-weighted imaging (top row) and fluid-attenuated inversion recovery (bottom row) images at different levels showing multiple hypointense foci corresponding to microhemorrhages on susceptibility-weighted imaging.
DISCUSSION
WAS is a rare X-linked recessive disorder caused in part by defects in the number and function of anti-inflammatory myeloid and lymphoid lineage cells.[1] This X-linked disorder demonstrates an estimated incidence of 1 in every 100,000 live births. It is seen almost exclusively in males.[2] WAS has a wide clinical spectrum ranging from mild, isolated thrombocytopenia to life-threatening hemorrhage, immunodeficiency with severe infections, eczema, autoimmunity, and malignancy. Severe infections with opportunistic pathogens, such as Pneumocystis jirovecii pneumonia, herpes simplex virus, and Aspergillus, also occur. Malignancy is frequently seen in patients with WAS, with lymphoproliferative disorders and myelodysplasia being the most common. Extranodal disease is common, predominantly involving the central nervous system (CNS) and lungs. Moreover, Kaposi sarcoma is seen in 15% of patients with WAS and lymphoproliferative disorders.[1]
Various imaging findings reported in patients with WAS include recurrent pneumonia, hemorrhage related to thrombocytopenia, or lymphoma with nodal and extranodal involvement. There are few case reports of necrotizing vasculitis and aortic aneurysms in patients with WAS.[1] Few case reports describe associations of splenic hamartoma,[3] infantile cortical hyperostosis,[4] and abdominal visceral aneurysms.[5] CNS imaging findings described in these patients are largely limited to few case reports of extranodal non-Hodgkins lymphoma.[6]
To the best of our knowledge, there is no reported case of diffuse cerebral microhemorrhages in patients with WAS. The underlying mechanism can be attributed to thrombocytopenia and autoimmune small vessel vasculitis which are described in the pathophysiology of WAS.[7] However, more radiological data of similar presentation with pathological correlation are required to establish the exact mechanism.
CONCLUSION
Wiskott Aldrich syndrome is a rare primary immunodeficiency disorder which is mainly diagnosed on clinical and laboratory grounds. However, radiological investigations are helpful is detection of pathologies that are either a result of disease process or an association with disease. This case report aims at describing one of the possible radiological manifestations that can be attributable to neurological complaints developing in these patients with a view to expand our insights into the radiological presentation of the disease.
TEACHING POINTS
Wiskott-Aldrich syndrome (WAS) is a rare primary immunodeficiency disorder with evolving insights into possible radiological manifestations.
Possibility of cerebral microhemorrhages should be considered in patients with WAS who present with sudden onset neurological signs and symptoms.
MCQs
-
Which of the following is false regarding WAS?
It is an X-linked disorder
It occurs only in females
Classic triad includes eczema, immunodeficiency, and thrombocytopenia
There is a predisposition for recurrent infections
Answer Key: b
-
Most common malignancy associated with WAS is?
Hodgkin’s Lymphoma
Non-Hodgkin’s lymphoma
Acute myeloid leukemia
Acute lymphoblastic leukemia
Answer Key: b
-
Which of the following MRI sequences is helpful in differentiating hemorrhage from calcification?
FFE
DWI
Phase
SPAIR
Answer Key: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Imaging features of primary immunodeficiency disorders. Radiol Cardiothorac Imaging. 2021;3:e200418.
- [CrossRef] [PubMed] [Google Scholar]
- Primary immunodeficiency diseases in Norway. J Clin Immunol. 2000;20:477-85.
- [CrossRef] [PubMed] [Google Scholar]
- Nonneoplastic, benign, and malignant splenic diseases: Cross-sectional imaging findings and rare disease entities. AJR Am J Roentgenol. 2014;203:315-22.
- [CrossRef] [PubMed] [Google Scholar]
- Infantile cortical hyperostosis associated with the Wiskott-Aldrich syndrome. Eur J Pediatr. 1988;147:518-9.
- [CrossRef] [PubMed] [Google Scholar]
- Wiskott-Aldrich syndrome: Life-threatening haemorrhage from aneurysms within the liver, small bowel mesentery and kidney, requiring both surgical and radiological intervention. J R Coll Surg Edinb. 2000;45:326-8.
- [Google Scholar]
- Sinonasal diffuse large B-cell lymphoma in a patient with Wiskott-Aldrich syndrome: A case report and literature review. Front Immunol. 2023;13:1062261.
- [CrossRef] [PubMed] [Google Scholar]
- The Wiskott-Aldrich syndrome: The actin cytoskeleton and immune cell function. Dis Markers. 2010;29:157-75.
- [CrossRef] [PubMed] [Google Scholar]







