Translate this page into:
Beyond the missed abortion: Uncovering the threat of scar ectopic in routine scan for RPOC
*Corresponding author: Nikita Mary Baby, Department of Radiology, Government Medical College, Ernakulam, Kerala, India. nikita92.nmb@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Baby NM. Beyond the missed abortion: Uncovering the threat of scar ectopic in routine scan for RPOC. Case Rep Clin Radiol. doi: 10.25259/CRCR_114_2024
Abstract
Cesarean scar ectopic pregnancy (CSEP) is a rare but potentially life-threatening form of ectopic pregnancy where the gestational sac implants within the myometrium at the site of a previous cesarean section scar. If undiagnosed, it can lead to severe complications during the management of non-viable pregnancies. This report discusses a case initially managed as a missed abortion, later diagnosed as CSEP on magnetic resonance imaging. The case emphasizes the necessity of accurate imaging in patients with a history of cesarean sections to prevent missed diagnoses.
Keywords
Cesarean scar ectopic pregnancy
Missed abortion
Magnetic resonance imaging
Retained products of conception
Cesarean section scar
Hemorrhage
INTRODUCTION
Cesarean scar ectopic pregnancy (CSEP) is a rare complication of pregnancy that occurs when the embryo implants within the scar tissue of a previous cesarean section. Seow et al. described CSEP as a growing clinical concern due to the rising number of cesarean sections globally, noting that early diagnosis is crucial to avoid potentially life-threatening complications such as uterine rupture and hemorrhage.[1] The incidence of CSEP is still relatively low, but with increasing cesarean deliveries, there is an urgent need for awareness and appropriate diagnostic approaches.[2] In this case, we report a patient initially diagnosed with a missed abortion but later confirmed to have CSEP through magnetic resonance imaging (MRI), underscoring the importance of advanced imaging.
CASE REPORT
A 40-year-old female, gravida 4 para 2 abortus 2, with one prior lower segment cesarean section (LSCS) and two previous dilation and curettage (D&C) procedures, presented for routine antenatal care. At 14-week gestation, an anomaly scan revealed a missed abortion. Surgical evacuation through D&C was performed on two occasions, but each attempt resulted in incomplete evacuation. Persistent vaginal bleeding and intermittent lower abdominal discomfort led to further imaging for suspected retained products of conception.
Radiological findings
MRI revealed findings consistent with a CSEP as illustrated in Figure 1. Vial et al. previously described how CSEP often presents as a mass embedded in the myometrium at the site of a previous cesarean scar, which was corroborated by the findings in this patient.[3] Specifically, the MRI identified:
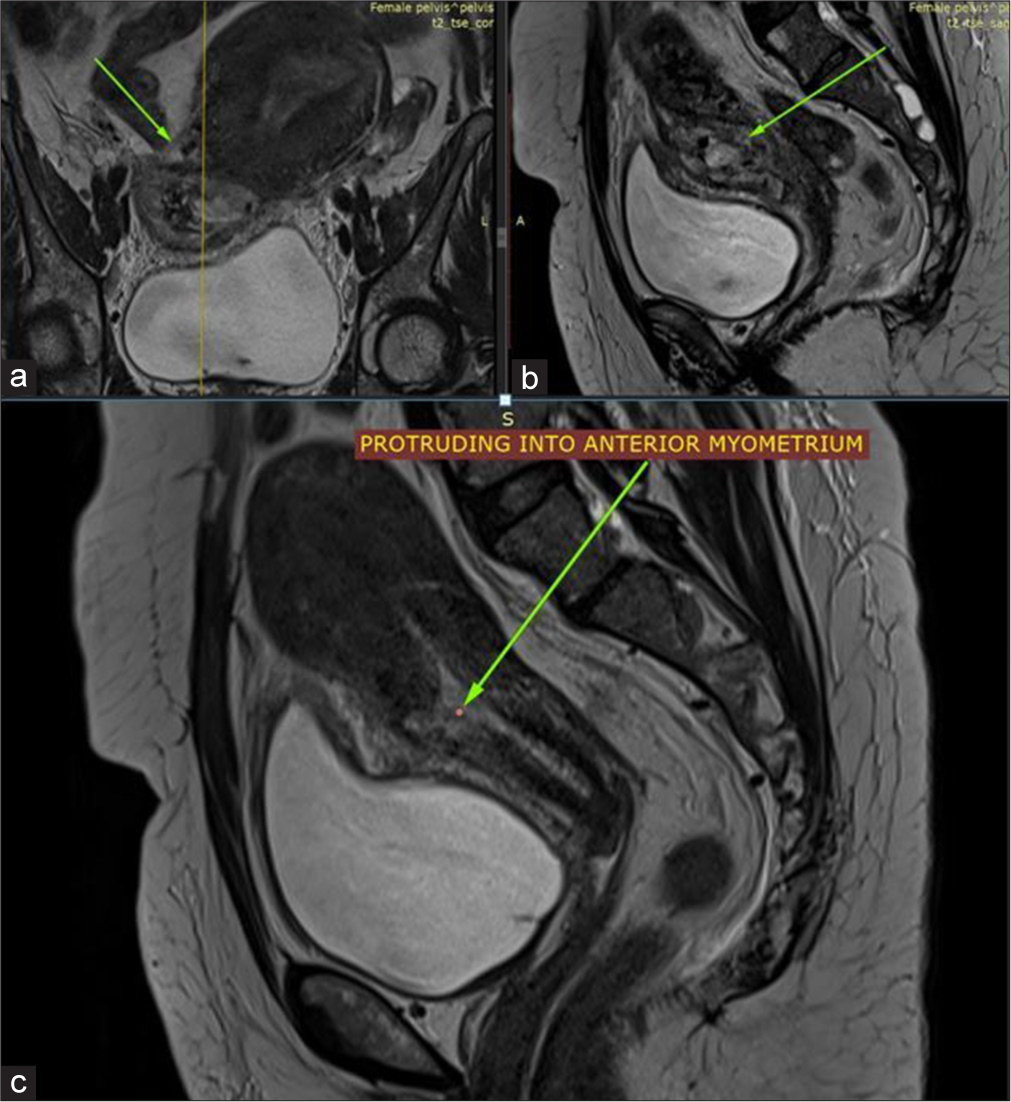
- T2 weighted (a) coronal and (b and c) sagittal sequence showing a mass protruding from the endometrial cavity in the lower part of uterus into the anterior myometrium (green arrows) with dehiscence/breeching of myometrium at the probable site of previous lower segment caesarian section.
A mass in the lower uterine segment protruding into the anterior myometrium at the site of the cesarean scar, which is typical for CSEP.[3]
Myometrial thinning and partial dehiscence at the site of the previous cesarean section, findings which are strongly suggestive of CSEP, as discussed by Jurkovic et al. in their extensive review of cesarean scar pregnancies.[4]
-
Intense blooming within the mass indicated calcified fetal structures [Figure 2], consistent with fetal bones. This type of presentation, described by Timor-Tritsch et al., is a key diagnostic feature for recognizing advanced cases of CSEP.[5]
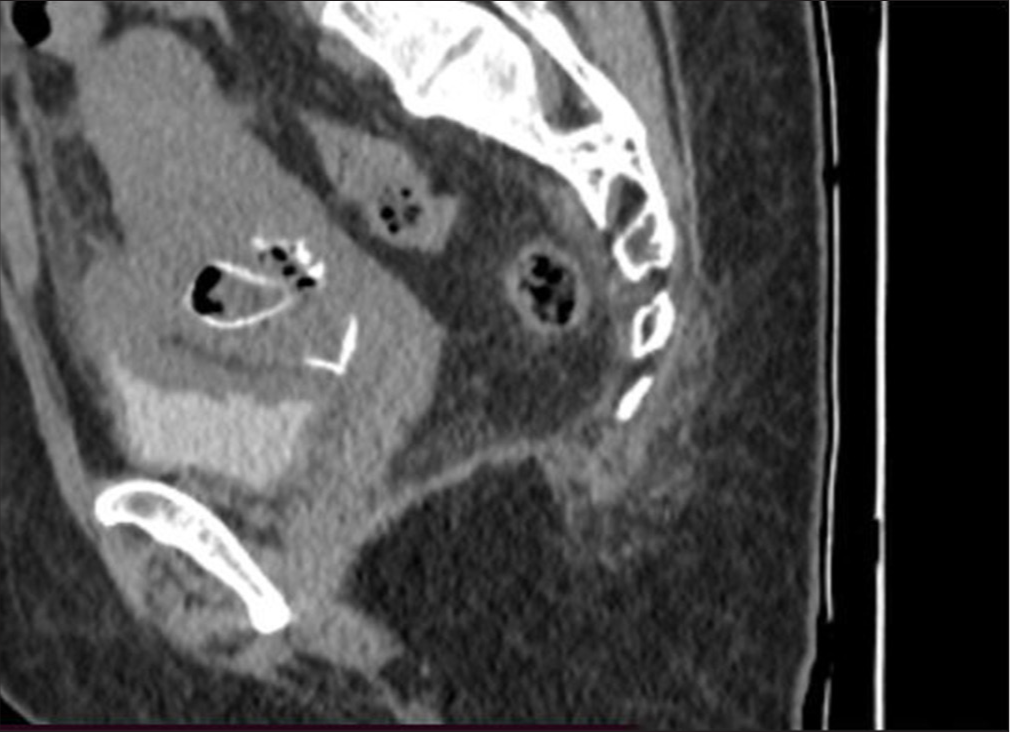 Figure 2:
Figure 2:- Computed tomography showing calcified structures (foetal bones).
Peripheral enhancement of the mass on post-contrast sequences, with associated air foci within the endometrial cavity, suggested the presence of retained products of conception.[6]
Diffusion restriction at the periphery of the mass, a characteristic finding seen in retained products, further confirmed the diagnosis.
In addition, a fluid density lesion closely adherent to the anterior uterine wall, possibly a seroma, was observed. The uterus was noted to be enlarged with inflammatory stranding in the surrounding fascia. Both ovaries and the cervix appeared normal, and there was no free fluid in the pelvis.
DISCUSSION
This case demonstrates the importance of imaging in identifying CSEP, especially in patients with a history of LSCS who present with symptoms of missed abortion. As Rotas et al. pointed out, conventional approaches to missed abortion, such as D&C, may fail to fully resolve cases involving CSEP due to the abnormal implantation within the myometrium.[2] Repeated surgical interventions may increase the risk of complications like uterine rupture or severe hemorrhage.[5]
In this patient, MRI was instrumental in confirming the diagnosis of CSEP and in identifying critical features such as myometrial dehiscence and the presence of calcified fetal tissue. Patel emphasized the role of advanced imaging techniques like MRI in providing a detailed evaluation of the extent of implantation and its associated complications, which was crucial in guiding further management in this case.[6]
This case further supports the argument made by Jurkovic et al. that radiological imaging, particularly MRI, should be considered an essential tool in evaluating suspected cases of CSEP, as it allows for accurate assessment of the implantation site, myometrial integrity, and risk factors for complications.[4]
TEACHING POINTS
Cesarean scar ectopic pregnancy should always be considered in every case of retained products of conception (RPOC) scan in patients with a history of cesarean section and abnormal imaging findings in the lower uterine segment, especially when conventional interventions fail to resolve symptoms.
MRI is pivotal in identifying critical diagnostic features of CSEP, such as myometrial thinning, dehiscence, and diffusion restriction, which are not easily discernible through routine ultrasound.
CONCLUSION
CSEP remains a diagnostic challenge, particularly in patients with a history of LSCS presenting with missed abortion. This case emphasizes the importance of considering CSEP in these patients and highlights the role of MRI in ensuring a comprehensive evaluation. Early and accurate diagnosis through advanced imaging can prevent severe complications, guide appropriate treatment, and avoid repeated surgical interventions. Early and accurate diagnosis can prevent complications such as uterine rupture, infection, or heavy bleeding, which are common with mismanaged scar pregnancies.
MCQS
-
Which of the following is a characteristic imaging finding in cesarean scar ectopic pregnancy (CSEP)?
A fluid-filled lesion in the adnexa
A mass in the lower uterine segment embedded in the myometrium
Thickened endometrial stripe without mass effect
Bilateral ovarian enlargement
Answer key: b
-
What is the most important role of MRI in the evaluation of cesarean scar ectopic pregnancy?
Identification of uterine anomalies
Accurate localization of the gestational sac and assessment of myometrial integrity
Detection of ovarian torsion
Evaluation of tubal patency
Answer key: b
-
Which of the following complications is most commonly associated with a delayed diagnosis of cesarean scar ectopic pregnancy?
Bilateral tubal blockage
Severe uterine hemorrhage and rupture
Asherman’s syndrome
Placental insufficiency
Answer key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cesarean scar pregnancy: Issues in diagnosis and management. Ultrasound Obstet Gynecol. 2004;23:247-53.
- [CrossRef] [PubMed] [Google Scholar]
- Cesarean scar ectopic pregnancies: Etiology, diagnosis, and management. Obstet Gynecol. 2006;107:1373-81.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy in a cesarean scar. Ultrasound Obstet Gynecol. 2000;16:592-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cesarean scar pregnancy. Ultrasound Obstet Gynecol. 2016;47:154-60.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic markers of cesarean scar pregnancy. Ultrasound Obstet Gynecol. 2007;30:765-70.
- [Google Scholar]
- Scar ectopic pregnancy: Imaging and diagnostic challenges. J Radiol Case Rep. 2014;8:7-12.
- [Google Scholar]







