Translate this page into:
A rare case of nasal anomaly
*Corresponding author: K. Nadanasadharam, Department of Radiology, Meenakshi Hospital, Thanjavur, Tamil Nadu, India. nadanasadharam912@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nadanasadharam K, Shanmuga Jayanthan S, Rupesh G, Yuvaraj N. A rare case of nasal anomaly. Case Rep Clin Radiol. doi: 10.25259/CRCR_121_2024
Abstract
Proboscis lateralis is a rare craniofacial anomaly. It describes a rudimentary nasal structure or appendage that consists of a soft, tubular nose-like structure that originates from the medial portion of the orbital roof. It may be associated with a number of facial and cerebral anomalies. The characteristics of the lesion and associated anomalies, along with the relationship of the lesion to the adjacent structures, must be known before the patient undergoes surgical correction. The patient should undergo multi-modality neuroimaging besides clinical evaluation to determine the exact details of the lesion. Computed tomography and magnetic resonance imaging are used as primary modalities before corrective surgery.
Keywords
Proboscis lateralis
Craniofacial anomaly
Rudimentary nasal structure
INTRODUCTION
Proboscis lateralis (PL) is a rare craniofacial anomaly with a reported incidence of <1 in 100,000 births. It is characterized by a soft, tubular, nose-like rudimentary nasal structure, or appendage that originates from the medial portion of the orbital roof. This trunk-like appendage is usually 2–3 cm in length and 1 cm in diameter, and it has a central tract which is lined with respiratory epithelium. The tract drains with a dimpled opening at the distal end of the proboscis, and in some cases, proximally it may be continuous with the paranasal sinuses. A number of facial and cerebral anomalies may be associated with PL. Usually, ipsilateral nasal wall anomaly is often associated, varying from total absence (aplasia), heminasal hypoplasia, to small tissue defect. In rare cases, the nose is normal. We report a case of PL in a 10-year-old male patient who presented with a tubular swelling near the medial canthus of the right eye since birth.
CASE REPORT
A 10-year-old boy presented with a pedunculated tubular swelling near the medial canthus of the right eye since birth. For the past 2 years, there was occasional mucinous discharge from the swelling. K/c/o cleft lip with palate (operated). On examination, there was a tubular swelling near the medial canthus of the right eye with punctum and mucinous discharge on compression. The patient had a normal intelligence quotient (IQ). The patient was advised to undergo a computed tomography (CT) brain scan.
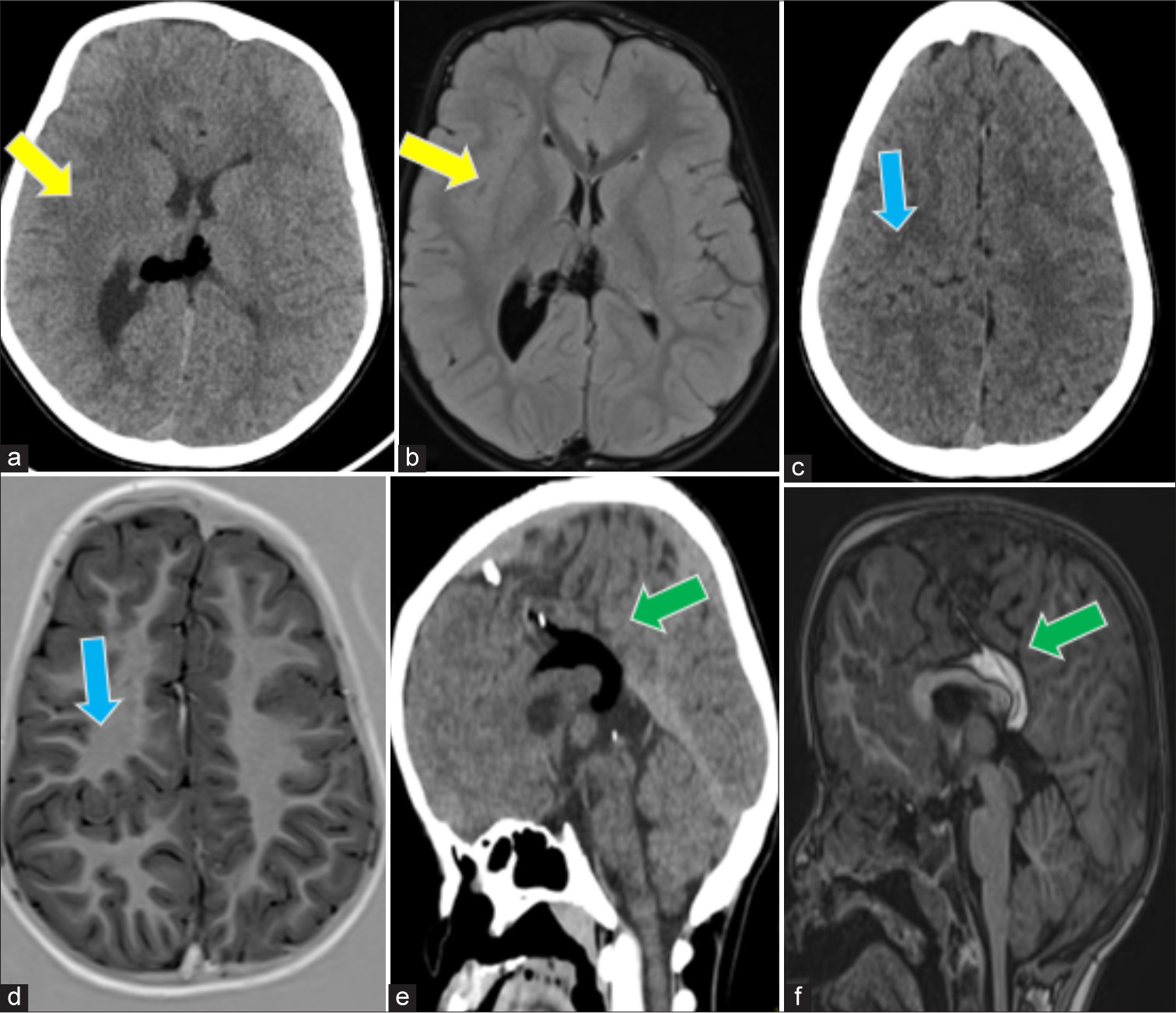
CT brain axial and coronal sections in soft-tissue window, and axial section in bone window, showed the bony and soft-tissue components of PL. No intracranial communication was seen. Magnetic resonance imaging (MRI) T2-weighted (T2W) coronal imaging showed a mixed T2 hyperintense lesion protruding from the roof of the right peri-orbital region. No demonstrable intracranial communication was observed. A 3D volumetric reconstructed image of the skull showed the osseous component of PL attached to the roof of the right orbit. CT brain axial section in soft-tissue window showed an exophytic fat-dense lesion from the right frontal region. MRI brain T1w sagittal section showed a T1 hyperintense fibro-fatty stalk (hamartoma) arising from the right frontal region [Figure 1].

- (a-c) CT brain axial soft tissue window, axial section bone window and coronal sections soft tissue window, shows bony and soft tissue component of proboscis lateralis. No intracranial communication was seen (yellow arrows). (d) MRI T2w coronal shows mixed T2 hyperintense lesion protruding from roof of right peri-orbital region. No demonstrable intracranial communication (yellow arrow). (e) 3d volumetric reconstructed image of skull shows osseous component of proboscis lateralis attached to roof of right orbit (yellow arrow). (f) CT brain axial section soft tissue window shows an exophytic fat dense lesion from right frontal region (green arrow). (g) MRI brain T1w sagittal section shows T1 hyperintense fibrofatty stalk (hamartoma) arising from right frontal region (green arrow). (h) Clinical picture of the patient. CT: Computed tomography, MRI: Magnetic resonance imaging.
CT brain axial and MRI brain fluid-attenuated inversion recovery axial sections showed a large right cerebral hemisphere with a prominent lateral ventricle – s/o hemimegalencephaly. CT brain axial and MRI brain T1w axial sections showed a grey matter-lined cleft in the right parietal lobe with closely approximated cleft walls – s/o closed lip schizencephaly. CT brain coronal and MRI brain T1w coronal sections showed mild corpus callosum hypoplasia with a T1 hyperintense/CT fat-dense lesion in the pericallosal region – s/o pericallosal lipoma [Figure 2].
- (a and b) Computed tomography (CT) brain axial and MRI brain FLAIR axial sections shows large right cerebral hemisphere with prominent lateral ventricle – s/o hemimegalencephaly (yellow arrows). (c and d) CT brain axial and magnetic resonance imaging (MRI) brain T1w axial sections shows a gray matter lined cleft in the right parietal lobe with closely approximated cleft walls – s/o closed lip schizencephaly (blue arrows). (e and f) CT brain coronal and MRI brain T1w coronal sections show mild corpus callosum hypoplasia with T1 hyperintense/CT fat dense lesion in pericallosal region – s/o pericallosal lipoma (green arrows). FLAIR: Fluid attenuated inversion recovery. s/o: Suggestive of.
MRI brain T2W coronal section showed absent bilateral olfactory bulbs (purple arrow). CT brain coronal bone window showed hypoplastic right middle and inferior turbinates, hypoplastic ethmoid bone and cribriform plate of the ethmoid, and asymmetry of the right orbit. X-ray dorsolumbar spine posteroanterior view and MRI T2W whole spine showed no vertebral abnormalities [Figure 3].
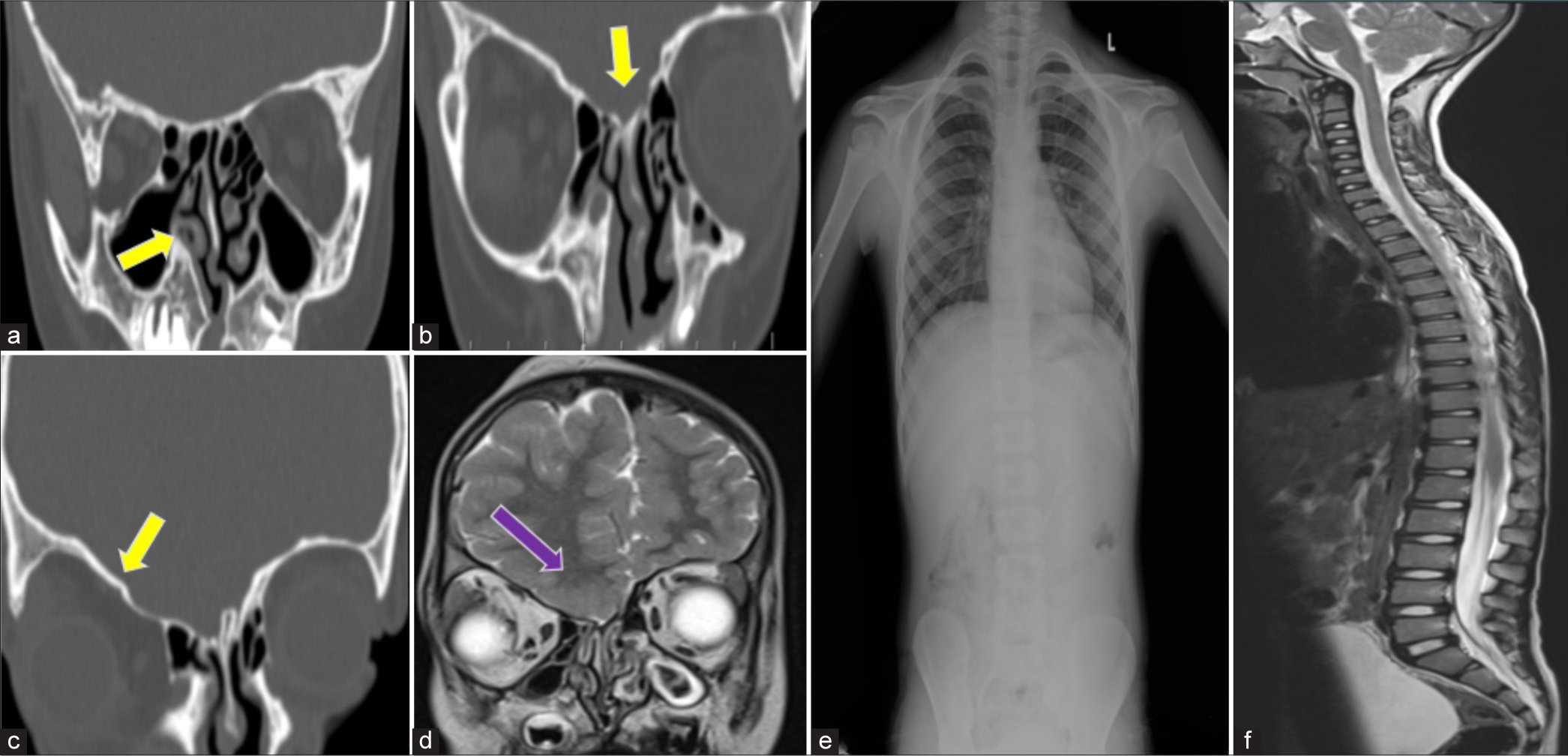
- Computed tomography brain coronal bone window (a-c) shows hypoplastic right middle and inferior turbinate’s, hypoplastic ethmoid bone and cribriform plate of ethmoid and asymmetry of right orbit (yellow arrows). Magnetic resonance imaging (MRI) brain T2-weighted (T2W) coronal section (d) shows absent bilateral olfactory bulbs (purple arrow). (e) X-ray dorsolumbar spine – PA view and (f) MRI T2W whole spine shows no vertebral abnormalities. PA: Posteroanterior, L: Left side.
DISCUSSION
PL is an extremely rare congenital craniofacial anomaly with an estimated incidence of 1 in 100,000 live births, showing a higher prevalence in males compared to females. This condition arises during the early stages of embryologic nasal development due to a defect in the nasal placode, which serves as a primary organizer for the formation of the nasal region of the midface. The abnormal development of the nasal placode can lead to midfacial anomalies. Specifically, PL is the result of developmental failure or absence of the medial and lateral nasal processes, leading to the fusion of the maxillary process with the contralateral frontal process. This condition is typically associated with the absence of the nose on the affected side but can sometimes present as an accessory nasal placode.[1-3] The classification of lateral proboscis suggested by Khoo (1985) and later modified by Sakamoto et al. is described in Table 1.[4,5]
| Group I | Lateral proboscis with normal nose (least common) |
| Group II | Lateral proboscis with an ipsilateral deformity of the nose (second in frequency) |
| Group III | Lateral proboscis with ipsilateral deformity of the nose, eye and or ocular adnexa (the most common type) |
| Group IV | Lateral proboscis with ipsilateral deformity of the nose, eye and or ocular adnexa, plus cleft lip and/or palate |
| Group V | Lateral proboscis with hypertelorism and encephalocele, a nasal, eye, and ocular adnexa defect, with either cleft lip or palate |
| Group VI | Lateral proboscis with holoprosencephaly |
Ocular-associated manifestations of PL include anophthalmia, lid cleft, cyclopia, choroidal cleft, microphthalmia, microcornea, hypoplastic optic nerve, and colobomas of the choroid, retina, and eyelids.
Facial-associated manifestations (38%) of PL include cleft lip and/or palate, lateral facial cleft, unilateral lipoma, cebocephaly, and facial bone abnormalities.[6]
Nasal-associated manifestations (44%) of PL include choanal atresia, abnormalities in the vomer and ethmoid bones, abnormal nasal pyramid, absent nasal bone, and heminasal aplasia/hypoplasia spectrum, along with nasolacrimal duct anomalies and olfactory bulb/tract anomalies.
Cardiovascular system (CVS)-associated manifestations of PL include double outlet right ventricle (RV), malposition of great arteries, patent ductus arteriosis, atrial septal defect, and RV outflow obstruction.[6]
Central nervous system-associated manifestations (19%) of PL include meningoencephalocele, hydrocephalus, sphenoorbital basal cephalocele, corpus callosum agenesis, arachnoid cyst, brain stem asymmetry, holoprosencephaly, colpocephaly, and hemivertebra.[6-8]
Gross anomalies of PL can be identified by proper clinical examination. However, the characteristics of the lesion and associated anomalies, along with its relationship to adjacent structures, cannot be fully known through clinical examination alone. These details must be known before the patient undergoes surgical correction.
CT and MRI are the imaging methods of choice to identify associated anomalies and the lesion’s relationship to adjacent structures. CT is useful for demonstrating the details of bony anatomy. PL may contain a bony portion, which is best revealed by CT. Details of the nasal cavity and the relationship of the proboscis with the orbit can be shown by CT. CT also shows cribriform plate defects better. However, it is technically difficult to obtain coronal CT images in very small babies.[9]
MRI is useful for understanding the relationship between the proboscis, the orbit, and associated soft-tissue abnormalities. Possible associated cerebral anomalies can also be excluded. The caudal orientation of the gyrus rectus, which may be secondary to cribriform plate defects at the lesion site, can be evaluated by coronal MRI.
Due to multisystem involvement, a multidisciplinary approach is required for proper management. Complete surgical excision at the base of the proboscis is desirable as a primary procedure if there is adequate ipsilateral nasal development or as a delayed excision if the proboscis is used in nasal reconstruction.[9,10]
Radiology plays a critical role in the surgical management of PL, a rare congenital facial anomaly. The primary role of radiology includes diagnosis, pre-surgical planning, and post-surgical assessment. The main purpose of imaging is to identify the absence, hypoplasia, or abnormality of nasal structures, assess associated anomalies such as holoprosencephaly (commonly linked to PL), and evaluate the position and patency of the nasolacrimal duct system. Advanced imaging creates 3D models of the craniofacial skeleton, aiding surgeons in visualizing the deformity and planning reconstructive techniques.[10,11]
CONCLUSION
Each case of PL presents unique challenges due to its rarity and potential associated anomalies. Early detection and comprehensive planning are vital for effective treatment, promoting improved patient outcomes and quality of life. Continued documentation and research on such rare cases are essential to enhance our understanding, refine treatment techniques, and guide clinicians in the future management of this complex condition.
TEACHING POINTS
Proboscis lateralis is a rare congenital malformation characterized by the presence of an abnormal protrusion or “proboscis” located laterally on the face, often accompanied by other craniofacial anomalies. This condition may present unique challenges for both diagnosis and management.
Early surgical intervention may be required to improve facial aesthetics and prevent functional impairments. Detailed genetic testing may be necessary to identify underlying syndromes or chromosomal abnormalities.
MCQs
-
What is PL?
A congenital facial anomaly characterized by a tubular structure on one side of the face
A genetic disorder causing limb malformation
An infection affecting the nasal cavity
A type of insect proboscis
Answer Key: a
-
PL is most commonly associated with which of the following conditions?
Cleft palate
Hypoplasia or absence of the nasal cavity on the affected side
Neural tube defects
Enlarged nasal septum
Answer Key: b
-
Which imaging modality of choice is used to diagnose PL and assess its associated anomalies?
Ultrasound
MRI
CT scan
X-ray
Answer Key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Clinicopathologic reports, case reports, and small case series. Proboscis lateralis. Arch Ophthalmol. 2001;119:1071-80.
- [Google Scholar]
- Lateral proboscis (elephant tusk) with orofacial clefts: A report of a rare case. Case Rep Pediatr. 2018;2018:6820972.
- [CrossRef] [PubMed] [Google Scholar]
- The proboscis lateralis--a 14-year follow-up. Plast Reconstr Surg. 1985;75:569-77.
- [CrossRef] [PubMed] [Google Scholar]
- New classification scheme of proboscis lateralis based on a review of 50 cases. Cleft Palate Craniofac J. 2012;49:201-7.
- [CrossRef] [PubMed] [Google Scholar]
- Proboscis lateralis: Clinical and radiological features. J Laryngol Otol. 2005;119:158-60.
- [CrossRef] [PubMed] [Google Scholar]
- The arrhinias: Proboscis lateralis literature review and surgical update. J Craniomaxillofac Surg. 2019;47:1410-3.
- [CrossRef] [PubMed] [Google Scholar]
- Proboscis lateralis: Evaluation of the anomaly and a review of two cases. Plast Reconstr Surg. 2006;117:140e-6.
- [CrossRef] [PubMed] [Google Scholar]
- Proboscis lateralis: Case report and review. Arch Otolaryngol Head Neck Surg. 2007;133:1051-3.
- [CrossRef] [PubMed] [Google Scholar]
- Proboscis lateralis: A unique case with choanal atresia and bilateral ophthalmopathy. Otolaryngology. 2015;5:183.
- [Google Scholar]







