Translate this page into:
Twists and turns: Unraveling unusual cervical instability in a case of prior neck infection
*Corresponding author: Aanchal Gupta, Department of Radio-Diagnosis, University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, India. aanchal14534@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta A, Tandon A. Twists and turns: Unraveling unusual cervical instability in a case of prior neck infection. Case Rep Clin Radiol. doi: 10.25259/CRCR_52_2024
Abstract
This case report describes a 17-year-old girl presenting with headaches, neck pain, and restricted neck movements, ultimately diagnosed with Grisel syndrome (GS) concurrent with basilar impression (BI). On initial admission, she was found to have retropharyngeal and paravertebral abscesses. Empirical treatment led to clinical recovery, but subsequent stiffness and restricted neck movements prompted further investigation. Imaging revealed rotatory atlantoaxial subluxation along with BI. This case underscores the importance of considering GS and/or BI in patients with neck infections and emphasizes early recognition and appropriate management to prevent neurological complications.
Keywords
Grisel syndrome
Basilar impression
Rotatory atlantoaxial subluxation
Retropharyngeal abscess
Torticollis
INTRODUCTION
Grisel syndrome (GS) is a rare condition characterized by non-traumatic rotatory subluxation of the atlas (C1) over the axis (C2), often associated with cervical infection or inflammation. Basilar impression (BI), or acquired basilar invagination, can result from protrusion of the odontoid process into the foramen magnum, leading to compression of posterior fossa structures and the cervical spinal cord. We present a unique case of GS with concurrent BI in a young patient with a history of multiple retropharyngeal and paravertebral abscesses.
CASE REPORT
We report the case of a 17-year-old girl who came to us for a follow-up computed tomography (CT) scan of the head and neck for unremitting headache and neck stiffness.
Six months before this follow-up, the patient initially presented with complaints of fever, headache, restricted neck movements, bulging of eyes, vomiting, and ear and neck pain. The patient was anemic with a hemoglobin count of 7.7 g/dL. Total leukocyte count was raised (17000/m3). Cerebrospinal fluid analysis showed a glucose count of 47 mg/dL, protein count of 116 mg/dL, and a total leukocyte count of 486/mm3. The tuberculosis work-up was negative. Imaging findings at that time were as follows: A lateral radiograph of the neck revealed increased thickness of the prevertebral soft tissue [Figure 1a], while the chest radiograph showed no abnormalities. Contrast-enhanced CT scan of the head and neck showed sulcogyral enhancement inferring meningitis [Figure 1b] and non-opacifying areas in bilateral cavernous, left sigmoid, and transverse sinuses suggesting cerebral venous sinus thrombosis (CVST) [Figure 1c]. Multiple rim enhancing collections were seen in the retropharyngeal and paravertebral soft tissues [Figure 1d-f]. A diagnosis of retropharyngeal and paravertebral abscesses, meningitis, and CVST was established. The patient was empirically started on antibiotics, steroids, and anticoagulants. She showed clinical recovery and was discharged on medication. Anticoagulation was continued due to residual CVST.
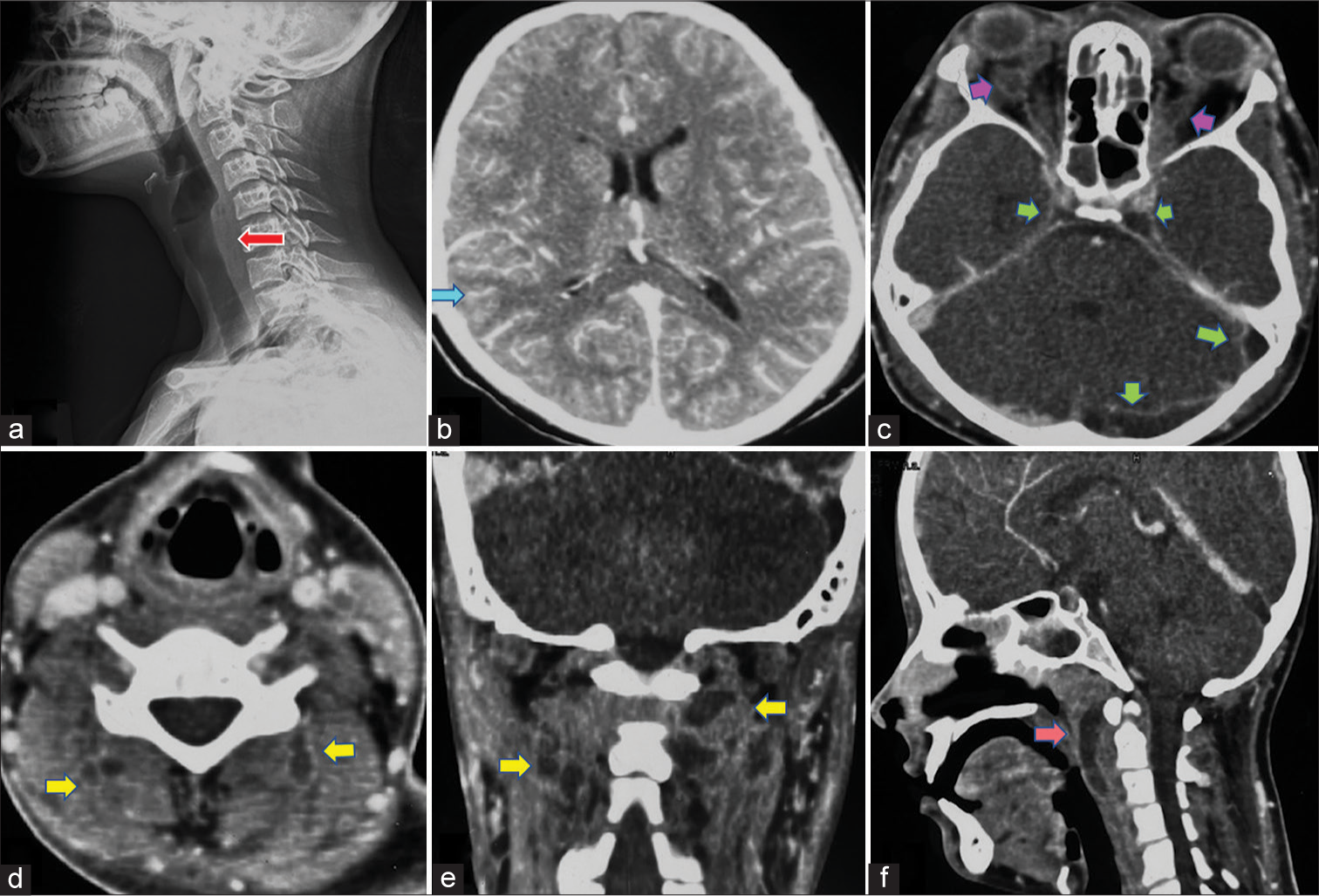
- Imaging at initial presentation shows, (a) lateral projection of neck radiograph showing increased prevertebral soft-tissue thickness (red arrow). (b) Axial section of contrast enhanced computed tomography (CT) scan of head, delayed phase showing sulcogyral enhancement (blue arrow). (c) Axial contrast enhanced computed tomography (CECT) head, venous phase showing filling defect in the left transverse, sigmoid, and bilateral cavernous sinuses (green arrows) suggestive of cerebral venous sinus thrombosis. Also note thrombosis of bilateral superior ophthalmic veins (purple arrows). (d) Axial and (e) coronal sections of contrast CT showing rim enhancing collections in bilateral paravertebral soft tissues (yellow arrows). (f) Sagittal section of contrast CT showing rim enhancing collection in prevertebral soft tissue (pink arrow) suggestive of retropharyngeal abscess. Note the tip of odontoid process is below an imaginary Chamberlain’s line at this stage.
The 1 month follow-up CT showed resolution of collections in neck [Figure 2a]. The patient was largely symptom free except for occasional headache and neck pain. Physiotherapy was commenced alongside analgesic treatment.
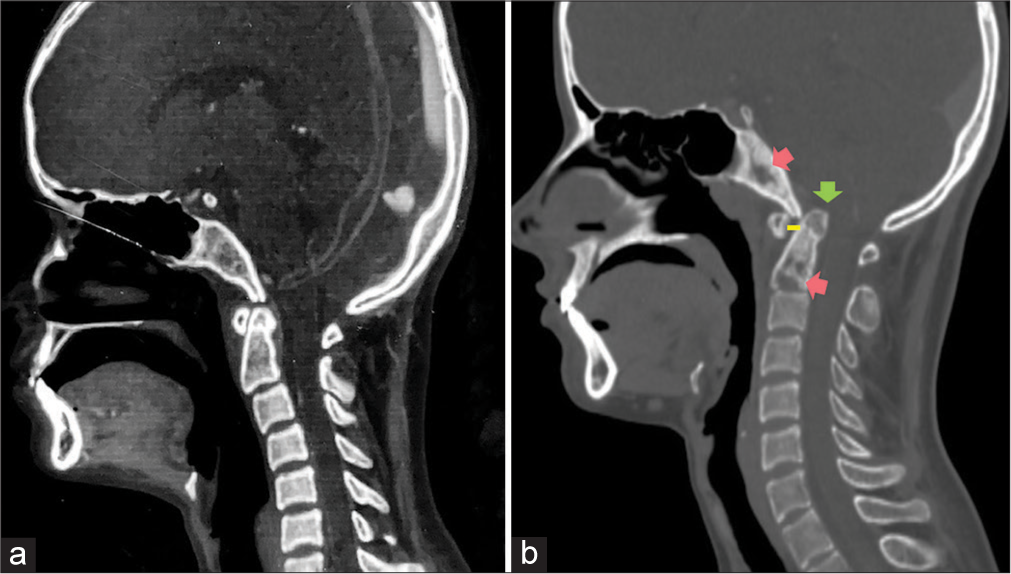
- Comparative computed tomography (CT) images sagittal sections of the same patient (a) taken 1 month after diagnosis of retropharyngeal abscesses showing resolution of collections. Note the normal position of the tip of odontoid process and the normal atlanto-axial distance. (b) CT taken 4 months after the aforementioned scan showing lytic permeative erosions in odontoid process and clivus (pink arrows) suggestive of osteomyelitis. The tip of odontoid process is above the imaginary chamberlain’s line and projecting into the foramen magnum (green arrow). Also note the increase in atlanto-axial distance (yellow line) in comparison to (a). These findings are suggestive of basilar impression or acquired basilar invagination secondary to infection of the cervical region.
After that, the patient gradually developed increasing stiffness in the neck and an inability to perform rotational movements at the neck. No neurological deficits or other complaints were reported. The patient was referred for the current CT scan to evaluate the current status of CVST and to look for any recurrent/residual disease that could explain her neck pain and stiffness.
While reading the current CT scan, the tip of odontoid process was above the Chamberlain’s line inferring Basilar Impression (BI). Furthermore, lytic permeative bony erosions in the clivus and odontoid process were evident, indicative of osteomyelitis. The intervertebral C2-C3 disc space was also reduced [Figure 2b]. We also could identify a Cock-Robin Position of the head on Volume Rendered CT images [Figure 3a-c] indicating the development of torticollis in the patient. The distances between the dens and the articular facets of atlas (C1) were grossly asymmetrical [Figure 3d] and the atlas (C1) was rotated in relation to the axis (C2) [Figure 3e] suggesting a diagnosis of nontraumatic rotatory C1-C2 subluxation. Such constellation of imaging findings in conjunction with the patient’s clinical history of rotational neck movements limitations following a retropharyngeal abscess were in concordance with the diagnosis of Grisel Syndrome along with Basilar Impression. After diagnosis, the patient received immediate counseling emphasizing the importance of avoiding aggressive neck movements and ceasing physiotherapy. The patient is now scheduled for an elective spine fixation surgery.
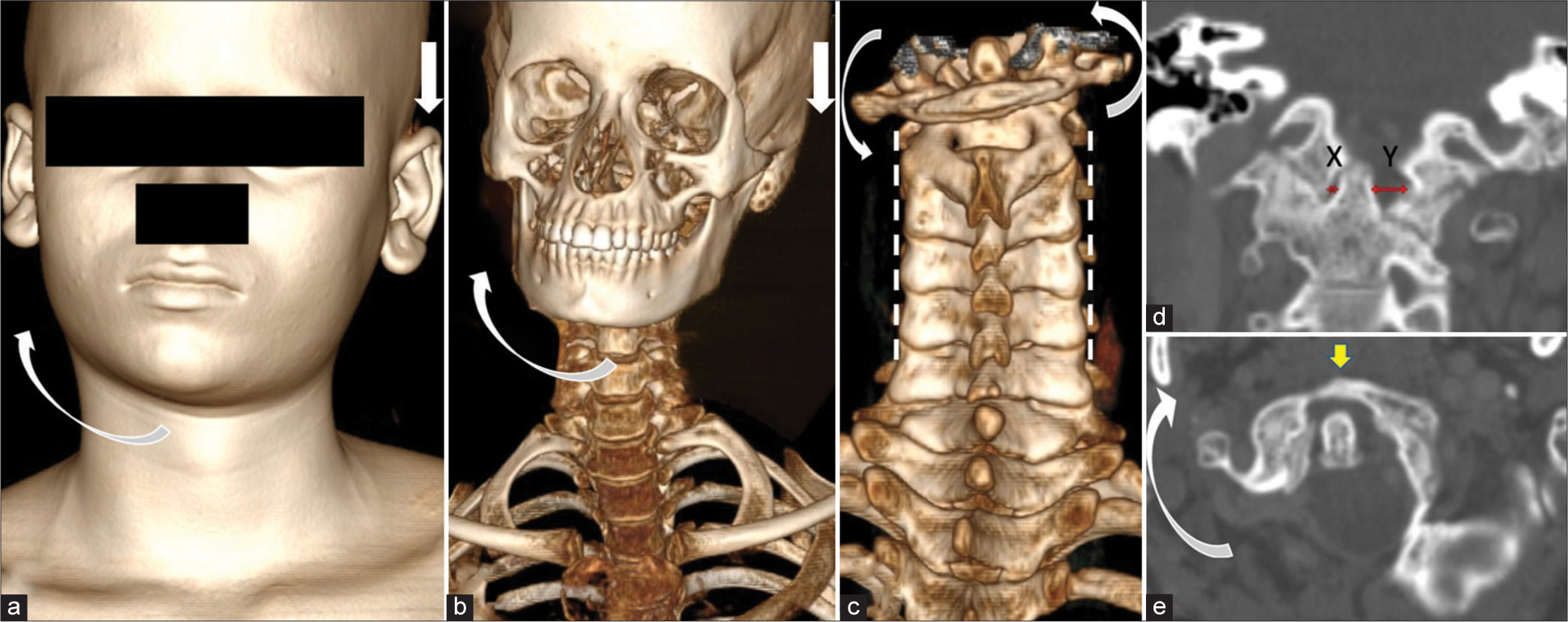
- Imaging at later stage shows (a) Shaded surface display of head and neck of the patient showing Cock-Robin position of head (head is tilted towards left side and chin is rotated to the contralateral side, demonstrated by straight and curved white arrows respectively) indicating torticollis. (b) Volume rendered 3 Dimensional CT images showing similar aforementioned findings (head is tilted towards left side and chin is rotated to the contralateral side, demonstrated by straight and curved white arrows respectively) (c) Volume rendered 3 Dimensional CT images from the posterior aspect of spine showing rotation of C1 (Atlas) over C2 (Axis), represented by curved white arrows. (d) Sagittal images of CT scan, bone window showing an asymmetry in the atlas-axis distance with a greater distance between dens and atlas on the left side (Y > X, red arrows denoting X and Y). (e) Axial images of CT scan, bone window showing rotation of atlas (yellow arrow) in relation to the axis, curved white arrow.
DISCUSSION
GS is a rare condition involving non-traumatic rotatory subluxation of the atlas (C1) over the axis (C2), initially described by Bell in 1830 in association with syphilitic pharyngeal ulceration. The atlanto-axial joint allows for 50–60% of cervical lateral rotation, with GS occurring when the anterior facet of C1 becomes fixed to the facet of C2 due to cervical infection or inflammation.[1]
About 90% of the cases of GS are seen in patients under the age of 21 without any gender predilection; however, rare occurrences in adulthood also exist.[2]
Various theories have been proposed; yet, the etiopathogenesis of GS remains unclear. A plausible explanation is the occurrence of cervical lymphadenitis due to a nasopharyngeal infection, resulting in spastic contraction of suboccipital and paravertebral muscles, leading to torticollis. Manipulation of the neck during surgical or anesthetic procedures resulting in GS has been described. Cases of GS with underlying Juvenile Idiopathic Arthritis, anomalies of the occipito-atlas-axis complex, and Trisomy 21 are also reported. All pathogenic processes share a common feature: an increase in inflammation and hyperemia leading to ligament laxity at the atlanto-axial articulation, resulting in subsequent joint subluxation.[1,3]
Common symptoms of GS include cervical pain, neck stiffness, and torticollis, with pain potentially radiating to the occipital region, face, and ears. Torticollis may result in the cock-robin position, where the head is rotated to one side and tilted to the other. Neurological symptoms are typically absent in most cases due to the wide vertebral canal at this level. Prognosis and management are guided by the Fielding and Hawkins classification [Table 1].[1,4]
| Fielding– Hawkins classification | Description | Therapeutic strategy |
|---|---|---|
| Type I | Pure rotation of the atlas in relation to the axis without anterior displacement | Conservative treatment: Soft collar, NSAIDs, muscle relaxants. |
| Type II | Rotated atlas with anterior displacement of 3–5 mm | Conservative treatment, reduction, Philadelphia brace |
| Type III | Atlas rotated with anterior displacement>5 mm | Surgical treatment, open reduction, fusion of C1–C2 |
NSAIDs: Non-steroidal anti-inflammatory drugs
Acquired basilar invagination, also known as BI, results from protrusion of the tip of the odontoid process into the foramen magnum. This can occur in the context of laxity of cervical ligaments.[5] The protrusion of the odontoid process into the foramen magnum can lead to compression of the contents of the posterior fossa and the high cervical spinal cord, compromised circulation, or impairment of the flow of cerebrospinal fluid. Neck movements are typically not restricted in isolated BI.[6]
GS in association with BI constitutes a clinical-surgical emergency. Radiological modalities are crucial for diagnosis. While CT with 3D reconstruction is mandatory for detecting the degree of cervical instability, it has limited sensitivity in early stages. At present, magnetic resonance imaging (MRI) is the modality of choice due to its lack of radiation and its ability to detect edema in the C1–C2 complex. MRI is also valuable in identifying compression of the spinal cord and posterior fossa structures.[1]
A diagnostic delay exceeding 1 month can significantly worsen the prognosis, as reducing a dislocated atlantoaxial joint becomes increasingly challenging, and chronic changes may develop in the alar and transverse ligaments. In untreated cases, pathological adhesion between C1 and C2 may occur, further complicating the condition.[7]
Our case stands out as a rarity, with only a few reported instances of concurrent rotatory atlantoaxial subluxation alongside BI documented in the literature.[6,8] The diagnosis was incidental, prompted by the patient’s investigation to rule out any residual or recurrent infection as the cause of her neck pain. Notably, the patient was already undergoing physiotherapy for the same issue, and it was during this treatment that a restriction of rotational neck movements was observed to emerge. The physiotherapy likely exacerbated the subluxation and BI in the context of the patient’s recovery from a retropharyngeal abscess and ongoing neck infection/inflammation.
A high index of suspicion for GS and BI is imperative for treating clinicians, surgeons, and radiologists. These conditions often coexist with neck infections, and the common presenting symptoms of neck and occipital region pain may be erroneously treated with mere analgesics if detailed knowledge and a high index of suspicion are lacking. Equally crucial is the ability of physiotherapists to recognize early signs of neurological compromise and to rule out any sinister underlying causes before initiating therapy. Failure to do so can lead to rapid deterioration of neurological symptoms, especially if physiotherapy is commenced under the assumption of benign musculoskeletal pain associated with cervical issues.
In summary, a high index of suspicion, early diagnosis, appropriate analgesia, and prevention of neurological deficits is the key to optimize outcomes in GS with concurrent BI.
CONCLUSION
GS and BI present diagnostic challenges but require prompt identification to prevent neurological sequelae. A high index of suspicion among clinicians, radiologists, and physiotherapists is essential for timely diagnosis and optimal patient outcomes. Radiological modalities such as CT and MRI are indispensable for diagnosis and assessing severity. Early recognition of neurological compromise and avoidance of inappropriate therapies is crucial for effective management.
TEACHING POINTS
GS and BI can present with varied symptoms, from neck pain to neurological deficits, making diagnosis challenging
A high index of suspicion among clinicians, surgeons, and radiologists is crucial for early detection
Diagnostic tools such as CT and MRI are inevitable for prompt diagnosis and for assessing associated complications.
MCQs
-
What is the primary mechanism underlying GS?
Traumatic injury to the cervical spine
Infection and inflammation leading to ligament laxity
Congenital malformation of the cervical vertebrae
Degenerative changes in the atlanto-axial joint
Answer Key: b
-
Which of the following is not true about GS?
It is acquired Basilar Invagination.
MRI is very sensitive for detection in early stages
Fielding-Hawkins classification is used for management.
Commonly seen in pdiatric age group
Answer Key: a
-
Which of the following is not true regarding biomechanics of C1–C2?
The transverse ligament stabilizes the odontoid against the anterior arch of C1
Alar ligaments are paired
Intervertebral discs are present between the atlas and axis
It allows 50–60% of cervical lateral rotation
Answer Key: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- C1-C2 rotatory subluxation in adults 'a narrative review' Diagnostics (Basel). 2022;12:1615.
- [CrossRef] [PubMed] [Google Scholar]
- Grisel's syndrome: A rare cause of torticollis with subluxation of the atlantoaxial joint secondary to a retropharyngeal abscess. Interdiscip Neurosurg. 2020;22:100872.
- [CrossRef] [Google Scholar]
- Inflammatory atlanto-axial subluxation (Grisel's syndrome) in children: Clinical diagnosis and management. Childs Nerv Syst. 2003;19:342-7.
- [CrossRef] [PubMed] [Google Scholar]
- Spine fusion for Atlanto-axial instability. J Bone Joint Surg Am. 1976;58:400-7.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of basilar impression. BMJ Case Rep. 2012;2012:bcr0220125851.
- [CrossRef] [PubMed] [Google Scholar]
- Basilar impression as complication of Grisel's syndrome. Clin Case Rep. 2017;6:185-8.
- [CrossRef] [PubMed] [Google Scholar]
- Grisel's syndrome: Non-traumatic atlantoaxial rotatory subluxation-report of five cases and review of the literature. Acta Neurochir Suppl. 2019;125:279-88.
- [CrossRef] [PubMed] [Google Scholar]
- Open reduction and decompression of atlantoaxial subluxation with basilar impression due to grisel syndrome using the cervical management base unit. World Neurosurg. 2020;138:129-36.
- [CrossRef] [PubMed] [Google Scholar]








