Translate this page into:
Uncommon suspect: A case report of a rare renal neoplasm
*Corresponding author: Anupran Ghosh, Department of Radiology, Lady Hardinge Medical College, New Delhi, Delhi, India. anupran94@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Amina N, Ghosh A, Prakash A, Ravina. Uncommon suspect: A case report of a rare renal neoplasm. Case Rep Clin Radiol. doi: 10.25259/CRCR_188_2023
Abstract
Primitive neuroectodermal tumors (PNETs) are a group of rare and aggressive malignancies primarily found in children and young patients. Primary renal PNETs are very much uncommon and share clinical and radiological features with renal cell carcinoma (RCC), thus posing a significant diagnostic and therapeutic challenge. This case report presents the clinical, radiological, and pathological findings of a primary renal PNET in an adult female patient, mimicking the radiological appearance of RCC.
Keywords
Renal primitive neuroectodermal tumor
Primitive neuroectodermal tumor
Radiology
Imaging
INTRODUCTION
Primitive neuroectodermal tumors (PNETs) are highly malignant neoplasms belonging to a group of small round blue cell tumors primarily encountered in pediatric and young adult patients with no gender preponderance. They originate from neural crest cells and exhibit aggressive behavior with a poor prognosis. While they are frequently seen in bones, soft tissues, and the central nervous system, primary renal PNETs are exceptionally rare (comprise <1% of all adult primary renal tumors). We present a case of a primary renal PNET, highlighting the significance of radiological assessment in the diagnosis and management of this rare tumor.
CASE REPORT
A 28-year-old female presented to our institution with complaints of the right-sided flank discomfort and hematuria of 2 months duration. The routine blood examination did not show any significant abnormality except for mild anemia. Urine analysis was positive for red blood cells. On clinical evaluation, there was a palpable lump in the right lumbar region which raised suspicion of a renal mass.
The patient was referred to the radiology department for further investigation where an initial ultrasound revealed a large irregular heterogeneous iso- to hypoechoic mass lesion arising from the upper part of the right kidney with significant internal vascularity on Doppler scan. For further evaluation of mass, a magnetic resonance imaging (MRI) study was performed on a 1.5 Tesla magnetic resonance scanner system (Sonata, Siemens; Erlangen; Germany), using a phased array body coil.
MRI revealed a large mass, measuring approximately 13 × 11.6 × 11cm (CC × AP × TR) arising from the upper and mid part of the right kidney accompanied by parenchymal infiltration and expansion. The mass showed heterogeneous signal intensity on both T1-weighted and T2-weighted images with areas of necrosis and hemorrhage [Figure 1]. On post-contrast images, there was moderate enhancement of the mass [Figure 2]. There was involvement of perirenal fat with the presence of retroperitoneal collaterals and tumor thrombus in the renal vein and inferior vena cava (IVC) [Figures 1 and 2]. No abnormality was seen in other visceral organs.
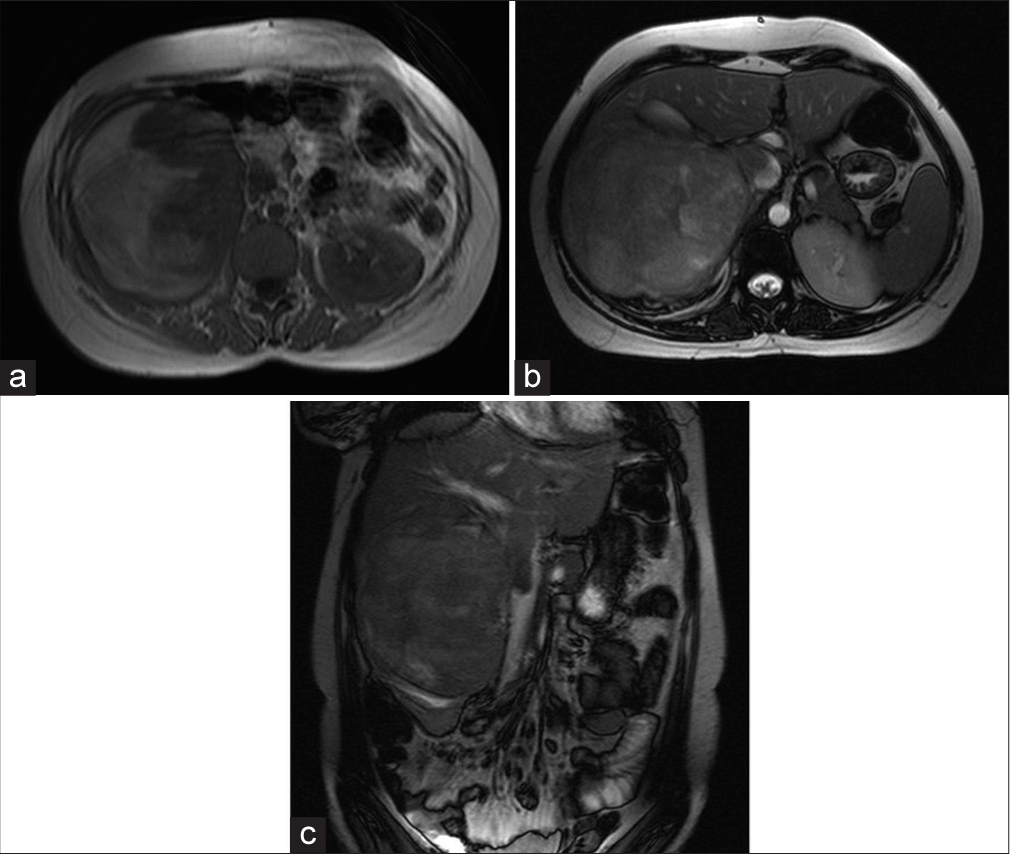
- A 28-year-old female presented with complaints of right sided flank discomfort and hematuria: Primitive neuroectodermal tumor. (a) Axial T1 weighted MR image, (b) axial T2 weighted MR image and (c) coronal T2 weighted MR image show a large heterogeneous right renal mass with tumor extension along the right renal vein and into the inferior vena cava, seen as filling defect within the same.
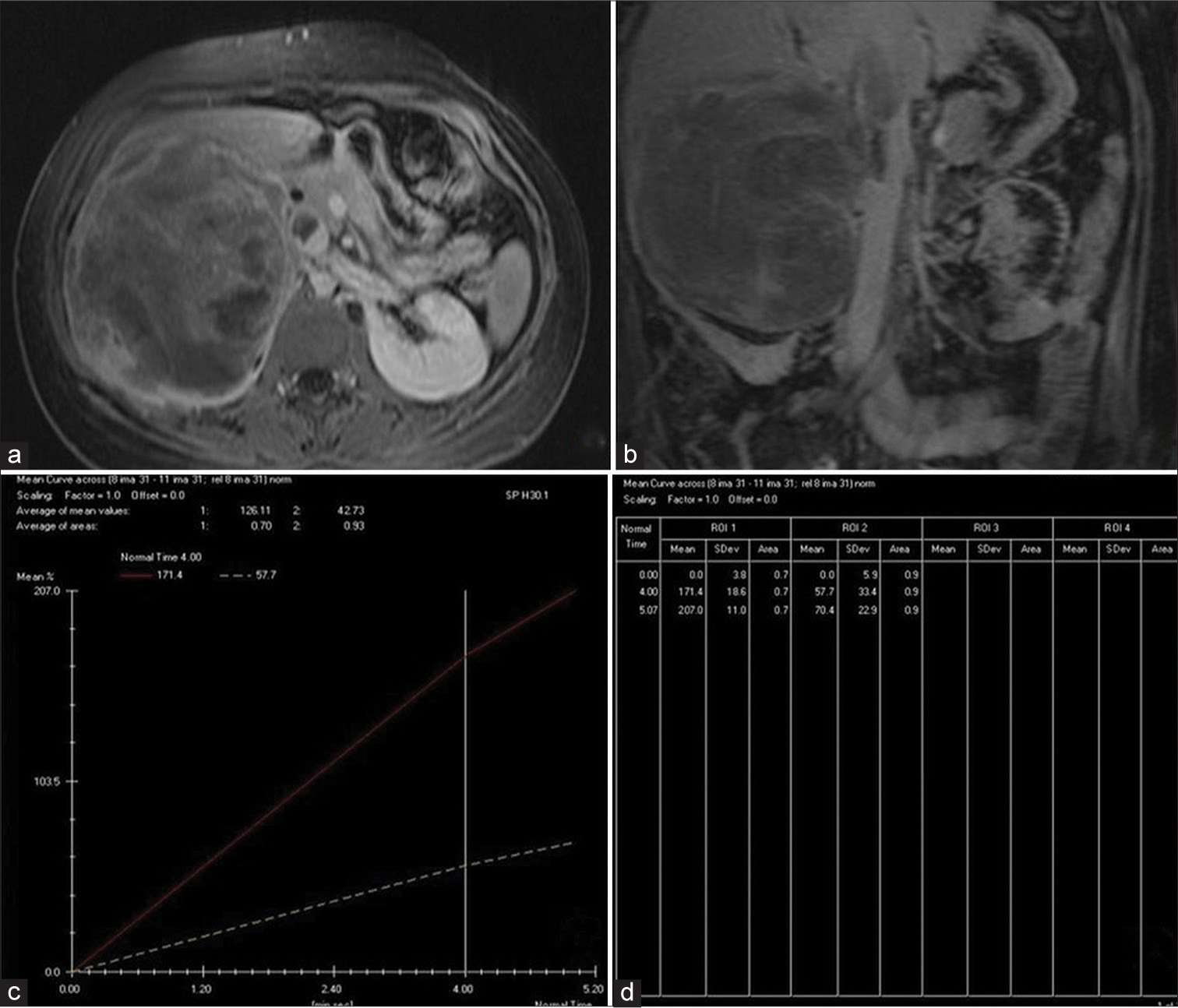
- (a) Post-gadolinium axial and (b) coronal magnetic resonance images demonstrate a heterogeneously enhancing mass with necrotic areas within. The thrombus within the distended right renal vein and inferior vena cava demonstrates similar enhancement as that of the mass. (c) Graph shows median percentage enhancement (signal intensity change) of the lesion (2) versus that in normal renal cortex (1) before and after contrast agent administration. (d) Percentage signal intensity changes in corticomedullary and nephrographic phases, respectively, were 57.7% and 70.4% for tumor and 171.4% and 207.0% for cortex.
The patient underwent radical nephrectomy. Renal parenchymal, pelvicalyceal infiltration, perirenal fat, and sinus invasions as well as tumor thrombus in renal vein and IVC were confirmed in histopathological evaluation of the surgical specimen.
Histopathological examination of the biopsy specimen showed characteristic features of a renal PNET, which included monomorphic round cells separated by fibrovascular septae displaying round to oval nuclei with a single prominent nucleolus and scanty cytoplasm. At places, perivascular pseudo-rosettes were also identified without any architectural arrangement [Figure 3]. On immunohistochemical staining, the tumor was positive for CD99, focally positive for transmembrane glycoprotein CD99, vimentin, and CD117, and negative for cytokeratin which further, confirmed the diagnosis.
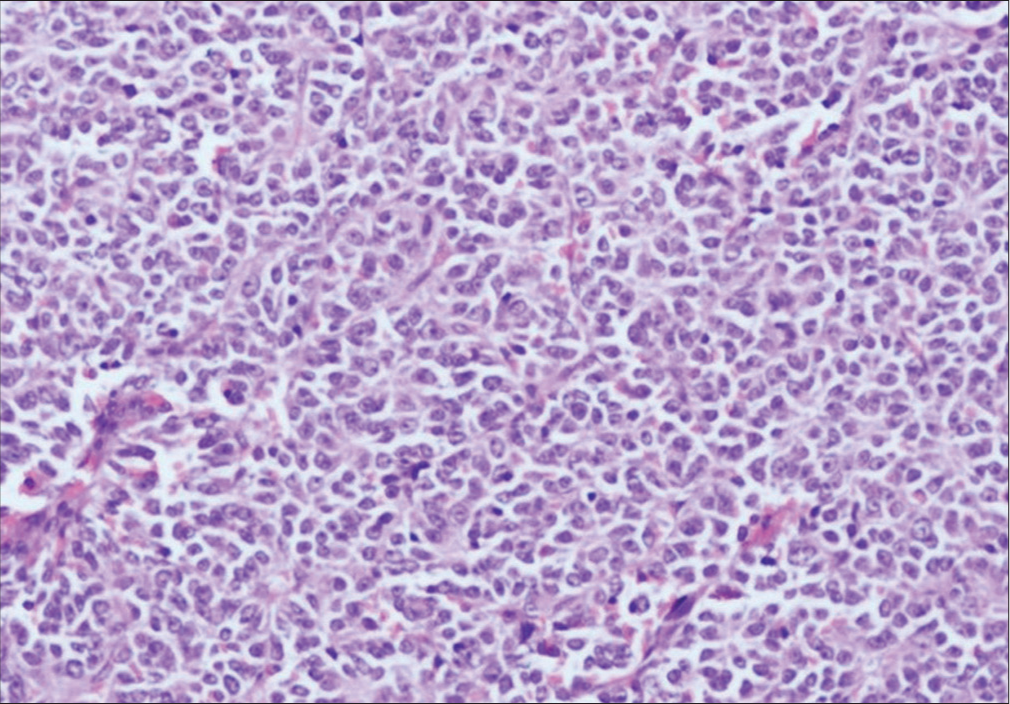
- Photomicrograph (histopathological) of the mass shows monomorphic round cells separated by fibrovascular septae displaying round to oval nuclei with a single prominent nucleolus with scanty cytoplasm. At places, perivascular pseudo rosettes could also be identified but there is no architectural arrangement (400 dpi).
DISCUSSION
PNET of the kidney is an extremely rare neoplasm with <150 reported cases in the literature.[1] The first case was described by Mor et al.[2] in 1994 in a 61-year-old patient. Some authors suggested that the origin of PNET in the kidney could be neural cells invaginated into the kidney during their development or embryonic neural crest cells migrating into the kidney and undergoing tumorigenesis. Karnes et al.,[3] in 2000, reported the first case of a renal PNET with vena cava tumor thrombus. Hari et al.[4] and Chea et al.[5] described the imaging appearance of PNET of the kidney as a large moderately enhancing heterogeneous mass with central low-density areas due to necrosis and areas of high attenuation within the tumor, presumably due to hemorrhage. Involvement of the renal vein and IVC, perinephric fat, and retroperitoneal lymphadenopathy occur commonly.
It is very difficult to radiologically predict a renal PNET preoperatively since it has a non-specific variegated imaging appearance which can closely resemble other malignancies of renal origin such as renal cell carcinoma (RCC) in most cases; however, certain imaging characteristics like the heterogeneous appearance of mass with ill-defined margins infiltrative growth pattern, showing areas of necrosis or hemorrhage along with moderate contrast enhancement in the solid portions, can raise suspicion toward a PNET.[6] In our case, diffusion-weighted imaging was not done; however, significant diffusion restriction with lower apparent diffusion coefficient values reflecting high cellularity may be seen in cases of PNET as suggested in some previous case reports.[7,8] Diagnosis needs to be confirmed on a post-operative histopathological study including immunohistochemistry. Other differentials may include renal lymphoma which may present as multifocal or focal renal masses, usually bilaterally, diffusely bulky kidneys or perinephric masses, and rarely metastasis to kidneys which may show variegated appearance depending on the primary tumor or medullary carcinomas or transitional cell carcinoma which are usually centrally located tumors without distortion of the renal contour (bean type).
The treatment strategy of renal PNET is multimodal including surgery, chemotherapy, and radiotherapy. Due to the difficulty in pre-operative diagnosis, neoadjuvant chemotherapy before surgery is not usually applicable. In case of local invasion of perinephric tissue or positive surgical margins, post-operative radiotherapy is recommended.
CONCLUSION
This case report underscores the importance of considering rare entities like PNET in the differential diagnosis of renal masses. Early identification of key radiological features, such as heterogeneous enhancement, lymphadenopathy, and renal vein thrombosis can aid in clinical suspicion, guide the appropriate management protocol and prompt surgical intervention, as the prognosis and available treatment options for these two types of renal tumor differ significantly. Given the rarity of renal PNETs, increased awareness and interdisciplinary collaboration are essential for optimal patient outcomes.
TEACHING POINTS
In the era of targeted therapeutics for malignancies, pre-treatment diagnosis of different subtypes of neoplasms is the need of the hour.
Despite the pre-treatment diagnostic difficulty relating to the non-specific imaging appearance of renal PNETs, certain key imaging characteristics when correlated with age and other clinical attributes may point toward this specific diagnosis. However, histopathological correlation is a must.
The possibility of PNET needs to be considered in a case of an ill-defined heterogeneous renal mass, with areas of necrosis or hemorrhage, showing slight contrast enhancement in the solid portions, especially in a young adult or adolescent patient in addition to other more common renal masses like RCC.
MCQs
-
Most common neoplastic mass in kidneys:
Angiomyolipoma
RCC
Metastasis
PNET
Answer Key: b
-
Renal PNETs show:
Avid post-contrast enhancement
Heterogeneous post-contrast enhancement with necrosis
No appreciable enhancement
Variable
Answer Key: b
-
RCC shows:
Propensity to invade renal vein.
IVC thrombus
Regional lymphadenopathy
All of the above
Answer Key: d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ewing's sarcoma/primitive neuroectodermal tumor of the kidney: A case report and literature review. Transl Androl Urol. 2019;8:562-6.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant peripheral primitive neuroectodermal tumor (PNET) of the kidney. Med Pediatr Oncol. 1994;23:437-40.
- [CrossRef] [PubMed] [Google Scholar]
- Primitive neuroectodermal tumor (extraskeletal Ewing's sarcoma) of the kidney with vena caval tumor thrombus. J Urol. 2000;164:772.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging features of peripheral primitive neuroectodermal tumours. Br J Radiol. 2008;81:975-83.
- [CrossRef] [PubMed] [Google Scholar]
- Primitive neuroectodermal tumour of the kidney: Radiologic-pathological correlations. Hong Kong Med J. 2008;14:240-3.
- [Google Scholar]
- Primary primitive neuroectodermal tumor of the urinary tract. J Formos Med Assoc. 2006;105:1008-12.
- [CrossRef] [PubMed] [Google Scholar]
- CT and MRI findings in a rare case of renal primitive neuroectodermal tumor. Pol J Radiol. 2016;81:401.
- [CrossRef] [PubMed] [Google Scholar]
- Renal masses: Characterization with diffusion-weighted MR imaging-a preliminary experience. Radiology. 2008;247:458-64.
- [CrossRef] [PubMed] [Google Scholar]







