Translate this page into:
TIPIC-al neck pain?
*Corresponding author: Zubin Vicky Driver, Department of Radiology, Seth GS Medical College, KEM Hospital, Mumbai, Maharashtra, India. driverzubin9@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adke SB, Driver ZV. TIPIC-al neck pain? Case Rep Clin Radiol. 2025;3:46-9. doi: 10.25259/CRCR_114_2023
Abstract
Transient perivascular inflammation of the carotid artery (TIPIC) is a benign unilateral self-limiting vascular condition that presents with neck pain, swelling, and increased pulsations just below and over the carotid bifurcation without structural vascular abnormality. TIPICs are frequently overlooked because they present with mild symptoms that resolve in a short period, both clinically and on imaging. Here, we present a case of a 32-year-old man who had neck pain for which ultrasound and magnetic resonance imaging was performed and later diagnosed with TIPIC syndrome on resolution of the symptoms.
Keywords
Transient perivascular inflammation of the carotid artery
Fay syndrome
Carotidynia
Focal neck pain
Case report
INTRODUCTION
First reported by Fay in 1927, Transient perivascular inflammation of the carotid artery (TIPIC), also known as idiopathic carotiditis, carotidynia, or Fay syndrome, is an unusual transient condition where the patient presents with unilateral or bilateral neck pain localized to the carotid artery region that is aggravated with coughing, sneezing, swallowing, and head movement.[1] It was first introduced in the International Classification of Headache Disorder (ICHD) in 1988 as carotidynia and was later removed in 2004 as a mere non-distinct neck pain syndrome.[2] The hypothesis was further supported with the advent of cross-sectional imaging, as one of the distinct inflammations of the carotid bifurcation and named TIPIC. In 2017, Lecler argued the inclusion of TIPIC syndrome instead of carotidynia in the new ICHD based on the fact that there is thickening and infiltration of the perivascular fat at the carotid bifurcation.[3]
CASE REPORT
A 32-year-old man presented with acute right neck pain and tenderness without neurological symptoms. There was no history of trauma. The inflammatory markers and fever profile were negative. On the ultrasonogram [Figure 1], there was a well-defined eccentric perivascular iso to hypoechoic lesion along the carotid bulb [Figure 1a and b]. To rule out dissection or intramural hematoma, magnetic resonance imaging (MRI) was ordered. On MRI, the perivascular lesion was T2 hyperintense (axial and sagittal plane) [Figure 2a and b], T1 hypointense [Figure 2c] and showed high signal on diffusion-weighted imaging without drop on apparent diffusion coefficient sequence [Figure 2d]. The caliber of the vessel was normal and the flow voids were maintained. There were no T1 hyperintensity or atherosclerotic changes, and the patient was started on nonsteroidal anti-inflammatory drugs (NSAIDs). Two weeks later, a follow-up scan performed [Figure 1c and d] showed a mild resolution of perivascular imaging and the diagnosis of TIPIC syndrome was confirmed.
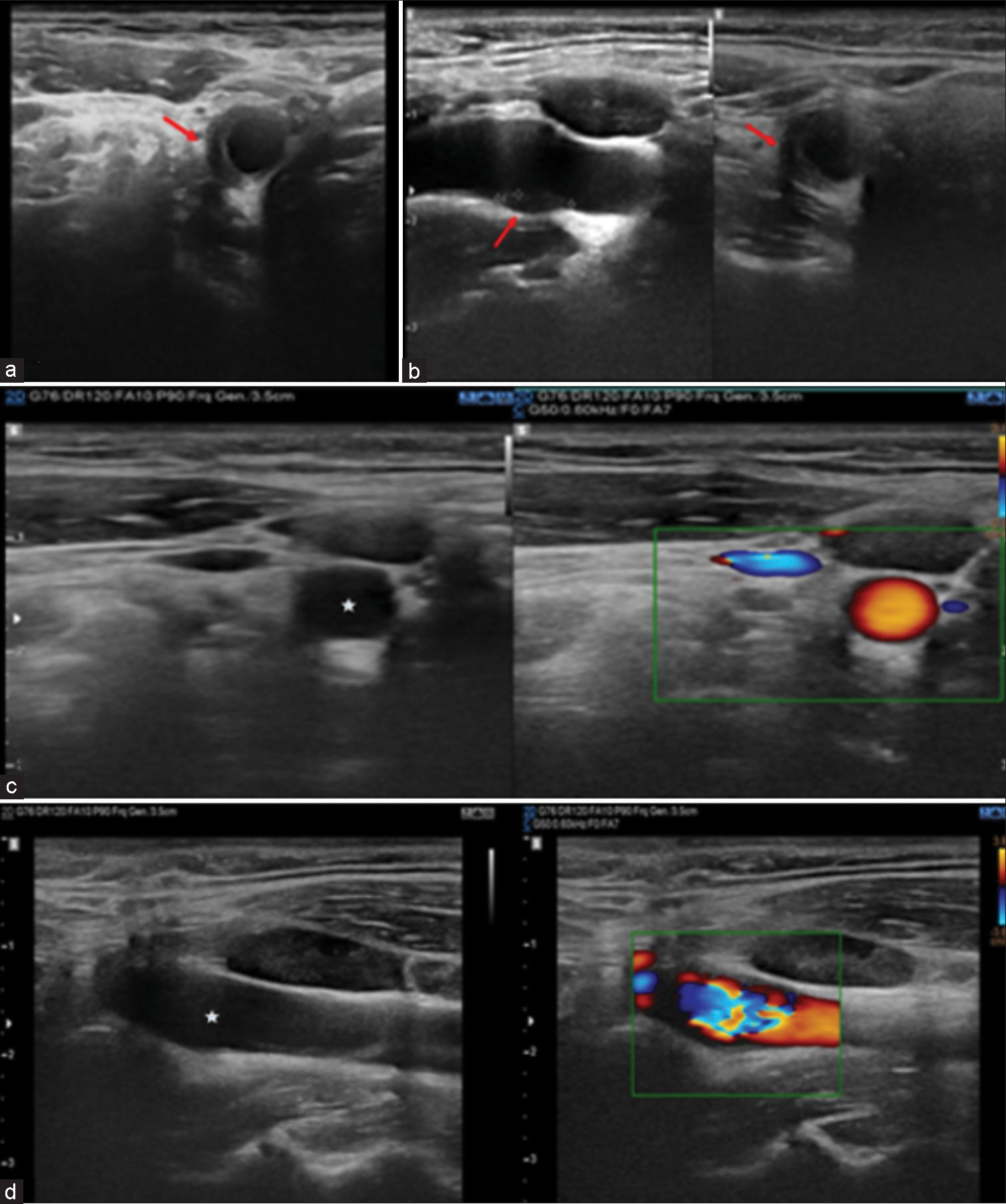
- Ultrasound images demonstrating eccentric perivascular hyperechoic soft tissue (red arrows) in the right distal common carotid artery at bifurcation level in (a and b) axial and sagittal plane. Follow-up ultrasound images (c and d) after 2-week post-non-steroidal anti-inflammatory drugs treatment complete resolution of eccentric perivascular hyperechoic soft tissue in the right distal common carotid artery at bifurcation level (white stars).
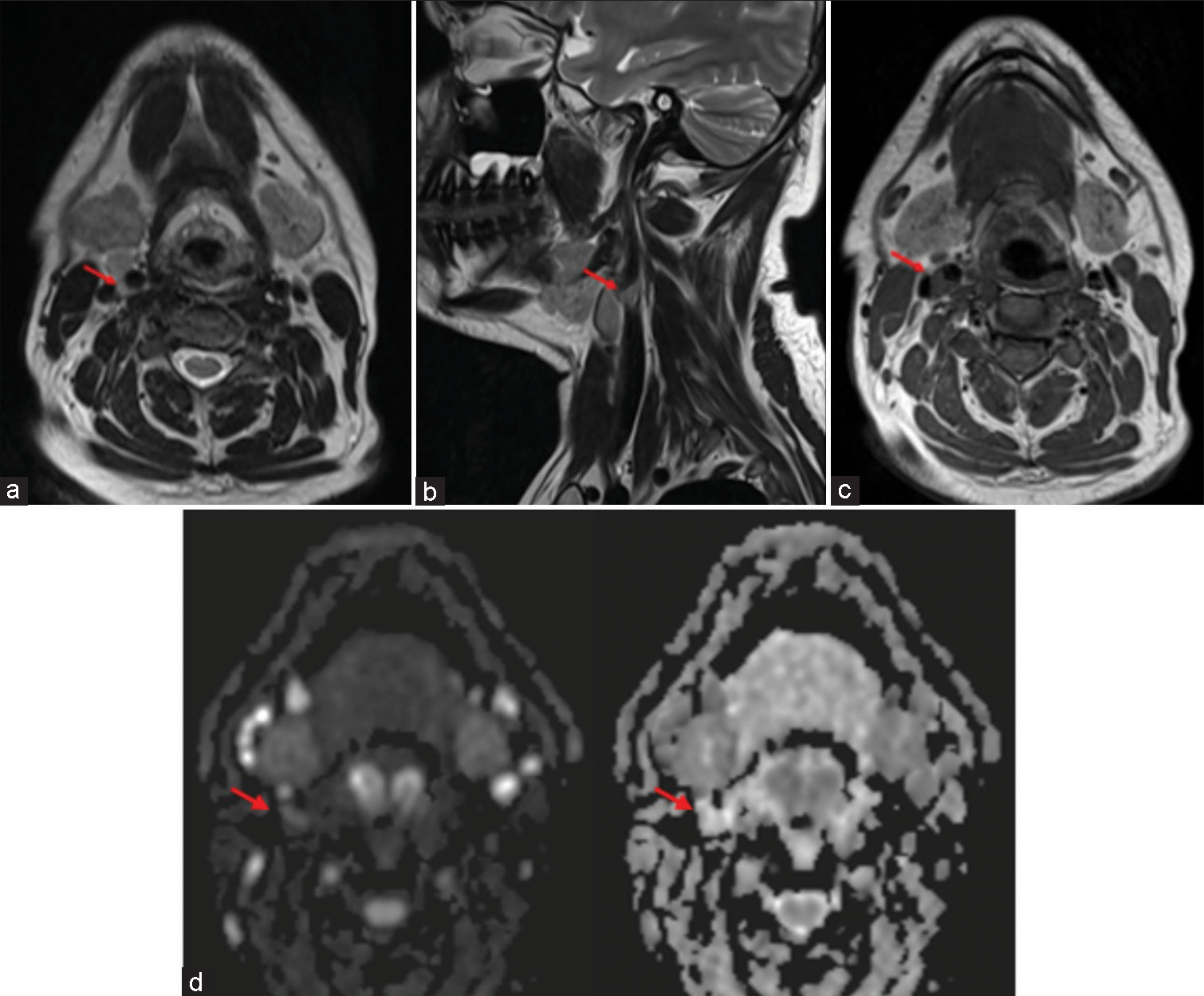
- (a) Axial T2-weighted image, (b) sagittal T2-weighted image, (c) axial T1-weighted image, and (d) axial diffusion-weighted images T2 hyperintense, T1 hypointense (red arrows) eccentric adventitial thickening with high signal on diffusion-weighted imaging without drop on apparent diffusion coefficient.
DISCUSSION
TIPIC is the diagnosis of exclusion and should be considered if the following other criteria are met:
Acute cervical neck pain (may or may not radiate elsewhere)
On imaging, there is eccentric perivascular inflammation
-
Resolution of the symptoms in 2 weeks[4]
In some patients, upper respiratory tract infection precedes neck pain, suggesting a possible autoimmune reaction.[3] It is commonly seen at 37 years of age (range: 15–78 years) with unilateral presentation (10% of cases are bilateral)[1] and a 1.5: 1 female-to-male ratio.[3]
Radiological finding of TIPIC: Ultrasound is used for the initial assessment and routine evaluation. There is eccentric hypoechoic perivascular thickening with mild luminal narrowing at the level of carotid bifurcation without dissection. On MRI, there is a T2 hyperintense and T1 hypointense perivascular lesion with intense post-contrast enhancement due to inflammation. Computed tomography, digital subtraction angiography, and positron emission tomography (PET) scans are not routinely performed for TIPIC because they provide little or no added value in the diagnosis and expose the patient to the harmful effects of contrast and radiation.[1] Recently, a PET scan has been used, which shows a focus on hypermetabolism of glucose in the region of carotid bifurcation.[3]
TIPIC involves the carotid sheath and vascular adventitia, whereas vasculitis involves inflammation of all layers of the vessel wall.[3] Atherosclerosis and vasculitis diffusely involve the carotid vessels, unlike TIPIC, in which there is a focal involvement.[2] Atherosclerotic plaques show concentric thickening with calcification, whereas in TIPIC, there is eccentric thickening. The carotid dissection is associated with Horner syndrome, whereas TIPIC has no neurological association.[3] Table 1 summarizes the pathology and radiological characteristics of TIPIC and its differentials.
| TIPIC syndrome | Atherosclerosis | Acute aortic syndrome: Dissection, intramural hematoma | Vasculitis |
|---|---|---|---|
| Transient non-specific inflammation of the adventitia and carotid sheath. | Cholesterol, fat deposition, and inflammation in the initial layer. | Dissection – tear in the intima and media layer of the vessel. Intramural hematoma – contained hemorrhage from vasa vasorum without the intimal tear. |
Autoimmune-mediated inflammation of all layers. |
| T2 hyperintense T1 hypointense eccentric lesion surrounding the vessel with post-contrast-enhancement without luminal narrowing or loss of flow void. | Concentric thickening of the intima with calcification causes luminal narrowing. Seen in old age. | T1W hyperintensity in the involved vessel due to blood products. | Diffuse involvement with luminal narrowing and post-contrast wall enhancement on MRI. |
TIPIC: Transient perivascular inflammation of the carotid artery, MRI: Magnetic resonance imaging
On gross examination, there is a fibrinous gray exudate, seen as an outward thickening of the vessel wall, which is different from the atherosclerotic plaque in which there is a thickening of the intima.[3] Histopathological confirmation is rarely performed due to the risk of carotid vessel injury.[5] However, on histopathology, pericarotid tissues and carotid adventitia show non-specific chronic inflammation with the proliferation of fibroblasts, leukocytes without granuloma formation. Small vessel proliferation embedded in a fibromyxoid stroma is a characteristic.[2]
TIPIC resolves spontaneously within 2 weeks or the resolution can be expedited with medications such as NSAIDs or steroids. In some patients, there is a relapse of symptoms every 1–6 months.[3]
CONCLUSION
Younger populations presenting with acute unilateral neck pain without any vascular or neurological cause should be screened on ultrasound. TIPIC syndrome should be one of the differentials in acute neck pain. TIPIC is an imaging diagnosis and should not be missed as patients can be counseled for the benign nature and quicker resolution with anti-inflammatory medications.
TEACHING POINTS
TIPIC on imaging shows a focal eccentric perivascular lesion confined to the carotid sheath and adventitial layer, while atherosclerosis involves intima causing luminal narrowing, and vasculitis involves all the layers of the vessel. Dissection and intramural hematoma can be differentiated from TIPIC using the T1W sequence.
It is a self-limiting non-specific inflammation that resolves spontaneously or with anti-inflammatory medications.
MCQs
-
Which of the following is not true about TIPIC syndrome?
Transient condition that resolves spontaneously
NSAIDs or steroids are used for the treatment
Associated with pain, tenderness, and pulsation at carotid bifurcation
Raised inflammatory markers are one of the major criteria for diagnosis
Answer Key: d
-
Which of the following statement(s) is/are true for TIPIC syndrome?
This involves concentric thickening of the adventitial layer
Pain resolves over a period of 4 weeks
Perivascular thickening with mild or no luminal narrowing of the carotid artery
Also known as Frey syndrome
Answer Key: c
-
What are the imaging characteristics of TIPIC syndrome?
Eccentric perivascular hypoechoic thickening on USG and T1/T2 hypointense on MRI
Eccentric perivascular hypoechoic thickening on USG and T2 hyperintense/T1 hypointense on MRI
Eccentric perivascular hyperechoic thickening on USG and T2 hyperintense/T1 hypointense on MRI
Eccentric perivascular hyperechoic thickening on USG and T1/T2 hyperintense on MRI
Answer Key: b
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Transient perivascular inflammation of the carotid artery syndrome assessed by ultrasound and CT. 2021.
- [Google Scholar]
- Carotidynia: A rare diagnosis for unilateral neck pain revealed by cross-sectional imaging. Case Rep Radiol. 2017;2017:7086854.
- [CrossRef] [PubMed] [Google Scholar]
- Carotidynia In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: http://www.ncbi.nlm.nih.gov/books/NBK560841 [Last accessed on 2022 Jul 26]
- [Google Scholar]
- Transient perivascular inflammation of the carotid artery syndrome. BMJ Case Rep. 2022;15:e248637.
- [CrossRef] [PubMed] [Google Scholar]
- TIPIC-A newly recognized syndrome: Multimodality imaging of a rare clinicoradiological entity. Indian J Radiol Imaging. 2021;31:488-91.
- [CrossRef] [PubMed] [Google Scholar]







