Translate this page into:
Perineal fistulation secondary to retained appendicolith: A rare complication of the unaccounted calculus
*Corresponding author: Pia F. P. Charters, Department of Radiology, Musgrove Park Hospital, United Kingdom. pia.charters@nhs.net
-
Received: ,
Accepted: ,
How to cite this article: Charters PFP, Lowe AS, Burn P, Vickery C. Perineal fistulation secondary to retained appendicolith: A rare complication of the unaccounted calculus. Case Rep Clin Radiol. doi: 10.25259/CRCR_70_2024
Abstract
An approximately 30-year-old male patient presented with perianal fistula disease. Examination under anesthetic revealed a complex extrasphinteric tract with internal opening in the region of the anterior inferior rectum, although an internal opening was not clearly identified. This failed to heal despite defunctioning procedure and packing of the perineal tract. Specialist center review of computed tomography and magnetic resonance imaging revealed a small cavity anterior to the rectum containing a small calcific density with a long tract extending down into the perineum. Seven years earlier, the patient had presented with clinical features of appendicitis. On retrospective review, an appendicolith can be seen on ultrasound and abdominal X ray (AXR). At surgery, the appendix had disintegrated leaving an abscess cavity. The appendicolith was not appreciated or removed and subsequently migrated into the pelvis acting as a source of infection which fistulated to the perineum. Subsequent removal of the calculus resulted in complete healing.
Keywords
Case report
Acute appendicitis
Complications of appendicitis
Extrasphincteric fistula
Dropped appendicolith
INTRODUCTION
Appendicitis is a common clinical condition. Extra sphincteric perineal fistula tracts are uncommon and suggest a cause other than cryptoglandular sepsis, such as pelvic inflammation related to inflammatory bowel disease or pelvic sepsis (e.g., diverticulitis or pelvic abscess). Dropped appendicolith is a rare complication following appendicectomy and may be a cause of pelvic sepsis with significant time delay. This possibility should have been considered sooner as a cause for unhealing extra sphincteric perineal fistulation, given the imaging findings that showed a small appendicolith in the deep pelvis related to the fistula tracts.
CASE REPORT
An approximately 30-year-old male presented with a short history of perianal fistulation. He had a medical history of coeliac disease and childhood asthma but took no regular medication. Examination under anesthesia (EUA) revealed a long cavity extending superiorly through the levators and approximating the anterosuperior wall of the rectum on the left. The complex sinus extended proximally 8 cm beside the rectum. No internal opening was identified. He underwent 3 further EUA’s within a 12 month period for the large discharging perianal abscess that, in spite of packing, failed to heal. An unenhanced 3 Tesla magnetic resonance (MR) study confirmed an extensive left-sided fluid tract in the ischioanal fossa, abutting the external sphincter on the left side. The tract was elongated in the anteroposterior plane measuring 47 × 7 mm and extended anterosuperiorly across the pelvic floor to occupy a 13 mm cavity anterior to the lower rectum. This cavity contained a small low signal focus, suggested to be gas or calcification [Figure 1]. Contrast-enhanced computed tomography (CT) of the abdomen and pelvis did not demonstrate an intra-abdominal cause for the fistulous tract, nor was free fluid seen.
Following local regional specialist referral, the working diagnosis was fistulation secondary to Crohn’s disease however, subsequent colonoscopy did not demonstrate luminal disease from his anus to his terminal ileum, MR study of his small bowel was normal, and a gastroscopy showed no evidence of inflammatory bowel disease. Biopsies taken around the fistula did not show Crohn’s and a CT sinogram did not demonstrate a rectal communication with the tract. A further EUA of the left rectal wall defect did not demonstrate full-thickness breach; therefore, 12 months after perineal symptoms began the patient underwent laparoscopic formation of a temporary defunctioning endcolostomy. The local gastroenterologists were unwilling to commence immunosuppression and biologic agents due to the lack of endoscopic, radiological, or biopsy evidence of Crohn’s disease.
A national specialist center referral 2 years after primary fistulation prompted review of the original radiology. A calcified “lith” was identified on serial magnetic resonance imaging studies as a small low signal focus within the anterosuperior tract where it occupied a small cavity anterior to the lower rectum [Figure 1]. Review of the CT and sinogram [Figure 2] revealed a 9 mm densely calcified calculus anterior to the rectum whereby the sepsis can be seen tracking from the nidus through the pelvic floor to the perineum.
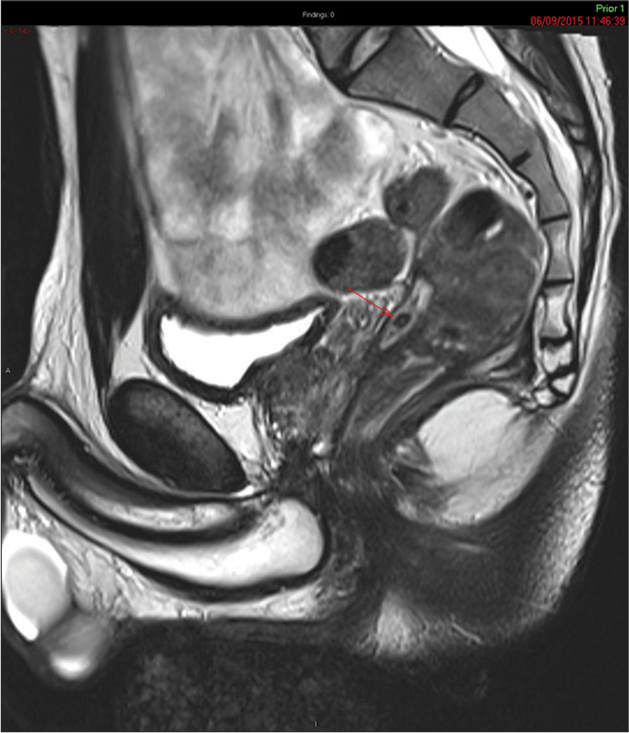
- Sagittal plane T2-weighted pelvic magnetic resonance imaging showing signal void of appendicolith (red arrow) in a high T2 signal fluid tract in the pouch of Douglas.
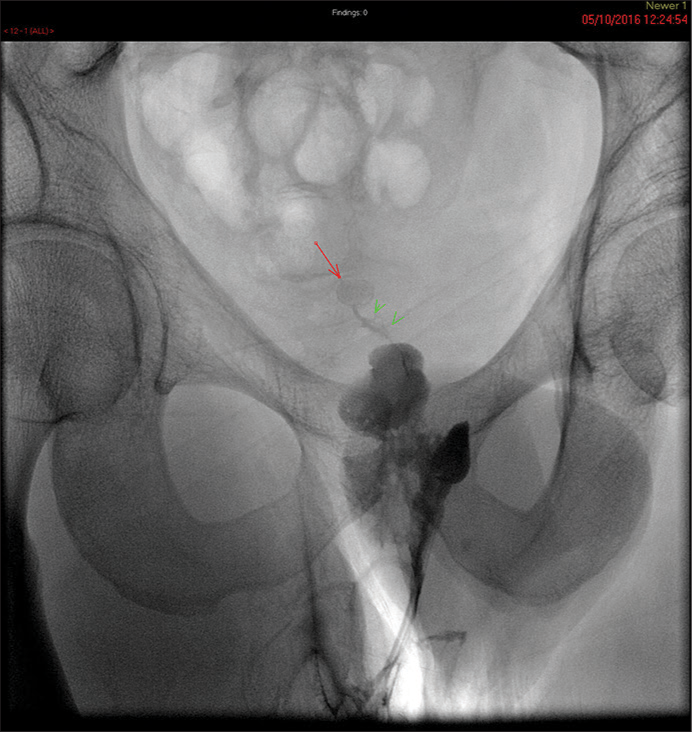
- Water soluble contrast fistulogram performed through perineal catheter outlining an irregular extrasphincteric tract and cavity with small fistula (green arrow heads) leading to calcified dropped appendicolith (red arrow) in the pouch of Douglas which was the source of the infection.
Seven years earlier, the patient had presented to the emergency department with clinical features of appendicitis. On retrospective review, the plain radiograph of the abdomen performed on admission revealed 10 × 8 mm hyperdense laminated calculus projected over the over the right iliac fossa and proximal ascending colon. An abdominal ultrasound at presentation demonstrated a 9 cm ill-defined mass of mixed echogenicity in the right iliac fossa, most likely to represent an appendix mass or abscess. Within the inflammatory mass, a 9 mm hyperechoic area was seen with posterior acoustic shadowing, favored to represent an appendicolith.
Appendicoliths are calculi formed within the lumen of the appendix and composed of calcium salts and firm fecal particulate. The relationship between appendicolith and appendicitis is complex, when an appendicolith is noted in the evaluation of a child with abdominal pain, the diagnosis of appendicitis is confirmed.[1] It is generally thought that appendicitis in the presence of an appendicolith has a more rapidly deteriorating trajectory and is associated with early perforation.[1] Imaging plays a key role in identifying the presence of an appendicolith ahead of surgical intervention and the appendicolith should be removed with the inflamed appendix.[2]
When an appendicolith is found outside of the appendix, it is pathognomonic of perforation.[3] A retained or “dropped” appendicolith is a rare complication of appendectomy or appendix perforation whereby the intra-abdominal appendicolith acts as an infective nidus and is associated with intra-abdominal abscess formation.[3] Percutaneous CT-guided drainage of an abscess formed secondary to a retained appendicolith is only successful in the short term and definitive treatment requires surgical drainage and removal of the appendicolith.[4] We present the case of perforated appendicitis with a retained appendicolith that remained in situ for 7 years, caused gravitational sepsis to the left side of the pelvis and a fistulating exterior tract through the left ischiorectal fossa.
There was no biopsy or endoscopic evidence of inflammatory bowel disease.
The patient had undergone an emergency open laparotomy which revealed an appendicular abscess causing subhepatic displacement of the caecum. The appendix had completed disintegrated into the necrotic abscess cavity which partially obliterated the appendix root. Attempts to remove the appendix were unsuccessful and the abscess was drained intraoperatively. An appendicolith was not identified at the time of surgery and not included in the histology sample. Failure to remove the appendicolith was not appreciated at the time. Review of post-operative radiographs demonstrated the appendicolith to have remained in situ and migrated into the pelvis. After a short uneventful admission and recovery, the patient was discharged.
Once the dropped appendicolith was identified as the likely cause of persistent perineal sepsis and removed, the clinical picture significantly improved. Within 6 months, his colostomy was successfully reversed and he returned to a normal diet with normal bowel function and near-total healing of the pararectal tract.
DISCUSSION
Appendicoliths form from calcified fecal material or foreign bodies and minerals in the appendix lumen. They are seen in 40% of patients subsequently going on to develop appendicitis.[4] The presence of an appendicolith has been identified as an independent prognostic risk factor for treatment failure in non-operative management of uncomplicated acute appendicitis, and it has also been shown to be associated with increased rate of appendiceal perforation.[5] A retained or “dropped” appendicolith is a rare complication of appendix perforation or appendectomy; fewer than 30 cases have been reported in the past 40 years relating to appendicular abscess.[6] Symptoms such as perineal fistulation can be attributed to Crohn’s disease and has led to incorrect diagnosis and treatment.[4] In this case, a vigilant investigatory work up and high clinical suspicion of an alternative diagnosis led to imaging review and subsequent correct diagnosis. The case demonstrates the classic appearance of a retained appendicolith on multiple modalities thus provides an excellent imaging reference compendium.
Radiological investigations take advantage of the hyperdense calcified nature of the calculus. On plain film an appendicolith is radiopaque, ovoid, or rounded calculus that is often laminated with a smooth border. Before appendectomy, the appendicolith is typically projected over the right iliac fossa; however, in the context of appendicitis and appendicular abscess, there may be ectopic displacement of the caecum. In our patient, the caecum was in a subhepatic location meaning that the appendicolith was projected over the right lumbar region [Figure 3]. Following appendicectomy, the intra-abdominal appendicolith will often move to the most dependent region within the abdominal cavity, the pelvis [Figure 2]. Other cases of perforation have observed the appendicolith in Morrisons pouch. CT is more sensitive at identifying and localizing the hyperattenuating calculus. Features such as appendicitis, abscess formation, and fistulation can also be identified. On transabdominal ultrasound imaging, the calculus will strongly absorb ultrasonic waves due to its closely packed molecular density. This typically casts a posterior acoustic shadow. Signal void on MR is typical for gas or calcium [Figure 1]. The persistent void on subsequent MR studies favors calcification.
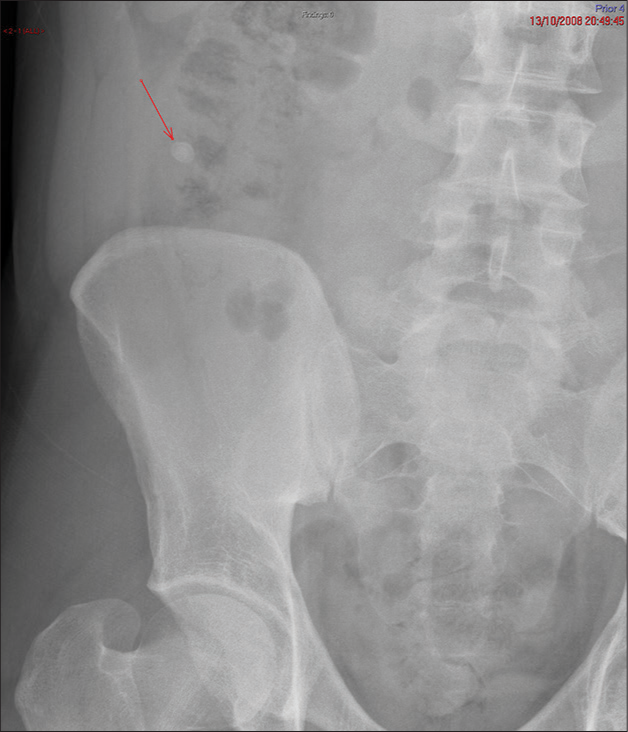
- AXR performed at presentation of appendicitis showing a calcified appendicolith (red arrow) in the right iliac fossa. AXR: Abdominal X Ray.
Clinical features that suggest an alternative diagnosis to Crohn’s disease are lack of synchronous pathology on MR small bowel, histological samples, and failure to improve despite defunctioning colostomy. When the bowel is bypassed, an inflammatory bowel process beyond the colostomy is expected to improve.
There is currently debate as to whether incidental appendicoliths should be removed with an elective appendectomy in children given that up to 90% are thought to subsequently develop appendicitis.[1,2]
CONCLUSION
Surgeons and pathologists should check the number of appendicoliths visible on pre operative imaging are accounted for in the operative specimen. Radiologists should consider dropped appendicolith as a potential cause for chronic extrasphincteric perianal fistulation.
TEACHING POINTS
When appendicitis is suspected, pre-procedural imaging is useful to quantify the presence and number of appendicoliths. If present, the number and site should be reported, then subsequently checked by the surgeon and histopathologist to ensure all are accounted for. A discrepancy between the number of calculi on imaging and the histopathological specimen should be investigated
If calcification is seen in the pelvis in the context of pelvic sepsis, the radiologist should review the past medical history for appendicitis or appendectomy and consider appendicolith. The CT appearance of dropped appendicolith may also be mimicked by other conditions such as dropped gallstones, dropped surgical clips or calcified phleboliths.
MCQs
-
Focal calcification in the pouch of Douglas may be caused by
Dropped appendicolith
Dropped gallstone
Calcified foreign body (e.g., surgical clip)
All of the above
Answer Key: d
-
Extrasphinteric fistulas are associated with which of the following?
Pelvic inflammatory process, infection or tumor
Pilonidal sinus
Hidradenitis suppurativa
Crytoglandular infection
Answer Key: a
-
The presence of appendicoth in the context of acute appendicitis
Carries a worse prognosis for non-operative management
Makes appendix perforation more likely
Is associated with malignant transformation
May be responsible for late complications
Answer Key: a, b, d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Nelson textbook of pediatrics (20th ed). Netherlands: Elsevier - Health Science; 2015. p. :1894.
- [Google Scholar]
- Applied radiological anatomy. Cambridge, UK: Cambridge University Press; 2012.
- [CrossRef] [Google Scholar]
- A complication of a dropped appendicolith misdiagnosed as Crohn's disease. Ann R Coll Surg Engl. 2011;93:e117-8.
- [CrossRef] [Google Scholar]
- Prevalence of appendicoliths detected at CT in adults with suspected appendicitis. AJR. 2021;216:677-82.
- [CrossRef] [Google Scholar]
- Appendicolith appendicitis is clinically complicated acute appendicitis-is it histopathologically different from uncomplicated acute appendicitis. Int J Colorectal Dis. 2019;34:1393-400.
- [CrossRef] [Google Scholar]
- The usefulness of CT guided drainage of abscesses caused by retained appendicoliths. Eur J Radiol. 2006;60:80-3.
- [CrossRef] [Google Scholar]







