Translate this page into:
Mineralizing microangiopathy: A rare cause of stroke in pediatric patients
*Corresponding author: Sayani Mahal, Department of Radiology, Lady Hardinge Medical College, New Delhi, India. sayanimahal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahal S, Puri S, Amina N. Mineralizing microangiopathy: A rare cause of stroke in pediatric patients. Case Rep Clin Radiol. doi: 10.25259/CRCR_1_2025
Abstract
Mineralizing microangiopathy is an under-recognized etiology of pediatric stroke. In the years, trivial head trauma and its association with basal ganglia infarct have been frequently reported. We report a case of an infant presenting with neurological deficits following trivial head trauma. Computed tomography scan of the head was done which showed an infarct in the right lentiform nucleus and linear calcification along the lenticulostriate arteries in bilateral basal ganglia.
Keywords
Lenticulostriate arteries
Microangiopathy
Pediatric stroke
INTRODUCTION
Although basal ganglia stroke following trivial trauma has been described in several case reports,[1-4] in the past years, no consensus could be reached upon about the exact etiopathogenesis. Cytomegalovirus (CMV) infection and basal ganglia calcification were touted as the major risk factors contributing to pediatric strokes following trivial head trauma in infants in some studies.[5] Lingappa et al.[6] in his study described a distinct clinicoradiological entity of basal ganglia stroke associated with mineralization in the lenticulostriate arteries.
CASE REPORT
A developmentally normal, 1-year-old female child presented with reduced movements of left upper and lower limbs for 2 days along with right facial deviation. This was preceded by a fall at her house which was not associated with loss of consciousness, seizures, or bleeding. No similar family history was reported. Non-contrast computed tomography (CT) was done which showed patchy area of hypodensity in the right lentiform nucleus and internal capsule suggesting acute infarct [Figure 1a and b]. Typical sharply marginated, linear hyperdensity was seen emerging vertically through the inferior part of the lentiform nucleus [Figures 1c and 2]. The course of these hyperdensities was similar to that described in anatomical literature about lenticulostriate arteries in infants and thus presumed to correspond to mineralized lenticulostriate arteries. The mineralized arteries were variable in number on each side. The clinicoradiological presentation was consistent with mineralizing microangiopathy with basal ganglia stroke.
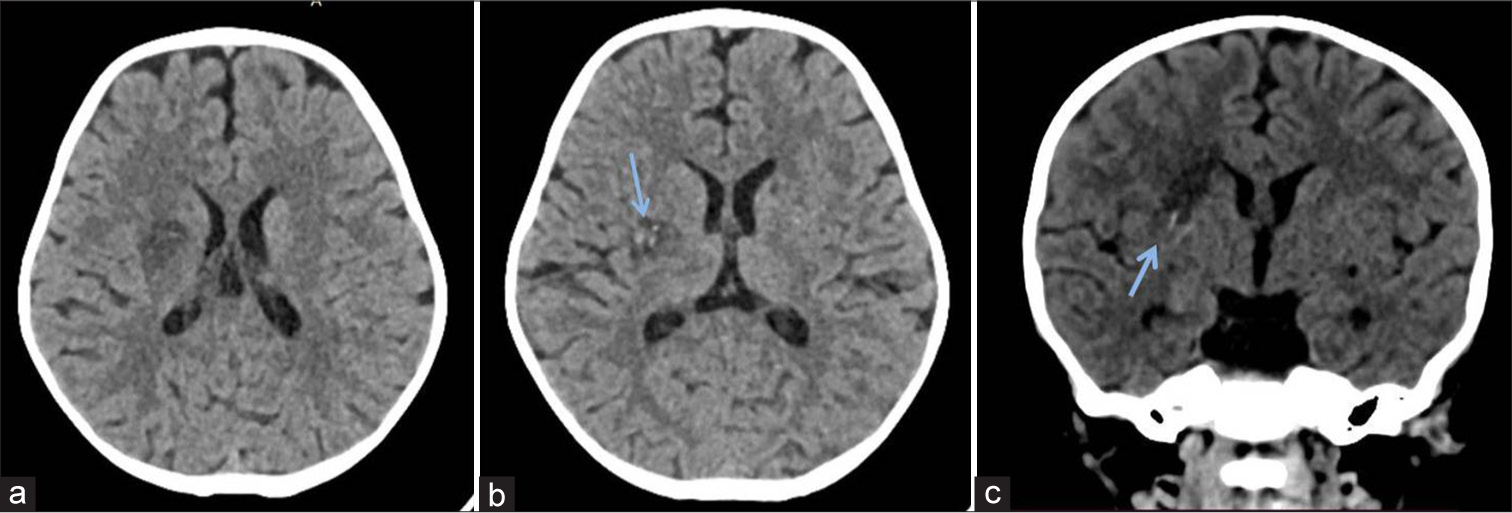
- (a and b) Computed tomography (CT) images of the brain axial CT images of the brain at the level of the lateral ventricles show well-defined hypodensity in the right lentiform nucleus suggesting acute infarct. (b) Axial CT image of the brain at the level of basal ganglia shows punctate foci of calcification within the infarct in the right lentiform nucleus (blue arrow). (c) Coronal CT image shows wedge-shaped infarct in the right lentiform nucleus with linear calcification in the right basal ganglia along the course of the lenticulostriate arteries (blue arrow).
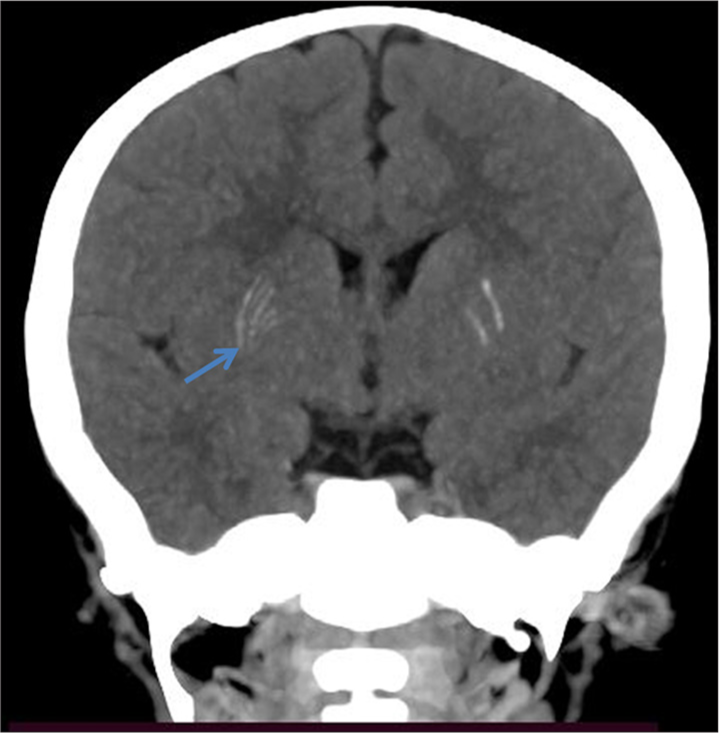
- Coronal maximum intensity projection image of the brain shows linear calcification along the course of bilateral leniculostriate arteries (right>left) (blue arrow).
DISCUSSION
Mineralizing microangiopathy resulting in basal ganglia infarct is a rare entity in itself occurring in <2% of all childhood strokes. The common presenting age group is between 6 months and 24 months of age. The presenting symptoms include hemiparesis following trivial trauma and increased occurrence of hemidystonia. The prognosis of these children is usually good. The hypothesized mechanisms are primarily transient arterial spasm and mechanical disruption in the flow of the perforating arteries. Intimal trauma with subsequent thrombosis has also been thought to be a chief cause. The perforating arteries arise from the middle cerebral artery in children at acute angles. This predisposes these vessels to stretching and distorting forces even after trivial head injury.[7] Furthermore, the shearing forces are stronger in pediatric skull due to elasticity. Although the specific cause of mineralization is not clear, sonographic lenticulostriate vasculopathy and CMV infection are thought to be contributory factors. On imaging, non-contrast CT scan shows linear calcification in bilateral basal ganglia along the course of the lenticulostriate arteries. In unilateral stroke, the outcomes are good, whereas infants with bilateral (recurrent) strokes had significant long-term disability.[6] On magnetic resonance imaging, restricted diffusion identifies areas of the infarct. On T2* sequences, particularly susceptibility-weighted imaging linear magnetic susceptibility artifacts are seen along the lenticulostriate arteries.
This case described here showed significant clinical improvement and follow-up imaging showed small area of gliosis in the right lentiform nucleus.
DIFFERENTIAL DIAGNOSIS
The major differentials include the conditions that lead to basal ganglia calcifications in children like congenital infections (cytomegalovirus, toxoplasmosis), Fahr disease, and other vascular conditions.
CONCLUSION
Mineralizing microangiopathy may be associated with pediatric basal ganglia stroke, although uncommon in occurrence. This is particularly precipitated by trivial trauma. We have described the clinicoradiological entity of mineralizing microangiopathy causing lentiform nucleus stroke after minor trauma in infants.
TEACHING POINTS
Mineralizing microangiopathy involving lenticulostriate arteries, a rare entity, is an uncommon cause of strokes.
It is precipitated mainly after trivial trauma.
Recurrent strokes are usually associated with long-term disability.
Transient hemidystonia is seen in a vast majority of patients.
CT is the imaging modality of choice.
MCQs
-
Mineralizing angiopathy involves which arteries predominantly?
Posterior circulation
Lenticulostriate arteries
Middle cerebral artery
Pial collaterals
Answer key: b
-
The common presenting age group is
5–6 years of age
6 months and 24 months of age
Neonates
Adolescents
Answer key: b
-
The presenting symptoms are:
Visual disturbance
Hemidystonia and hemiparesis
Hemiballismus
Movement disorders
Answer key: b
-
Classic imaging finding is:
Calcified lenticulostriate arteries with basal ganglia stroke
MCA thrombus
Posterior circulation infarct
Multiterritorial infarcts
Answer key: a
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Mineralizing angiopathy with basal ganglia stroke in an infant. Ann Indian Acad Neurol. 2015;18:233-4.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral basal ganglia infarction after mild head trauma. Pediatr Int. 2009;51:829-31.
- [CrossRef] [PubMed] [Google Scholar]
- Posttraumatic infarction in the basal ganglia after a minor head injury in a child: Case report. Turk Neurosurg. 2008;18:415-9.
- [Google Scholar]
- Pediatric traumatic putamenal strokes: Mechanisms and prognosis. Surg Neurol Int. 2011;2:51.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features and risk factors of cerebral infarction after mild head trauma under 18 months of age. Pediatr Neurol. 2013;48:220-6.
- [CrossRef] [PubMed] [Google Scholar]
- Mineralizing angiopathy with infantile basal ganglia stroke after minor trauma. Dev Med Child Neurol. 2014;56:78-84.
- [CrossRef] [PubMed] [Google Scholar]
- Some observations on the anatomy of the middle cerebral artery. Can J Surg. 1964;7:134-9.
- [Google Scholar]








