Translate this page into:
Imaging in adult presentation of congenital intrapericardial diaphragmatic hernia
*Corresponding author: Aruna R. Patil, Department of Radiology, Apollo Hospitals, Bengaluru, Karnataka, India. dr.arunarpatil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tamanna A, Patil AR, Alam S, Nandikur S. Imaging in adult presentation of congenital intrapericardial diaphragmatic hernia. Case Rep Clin Radiol. doi: 10.25259/CRCR_3_2025
Abstract
Intrapericardial diaphragmatic hernia is a rare non-hiatal diaphragmatic hernia that occurs due to a traumatic or congenital defect in the pericardial portion of the central tendon of the diaphragm. It is characterized by the herniation of abdominal viscera into the pericardial cavity. A high index of suspicion and appropriate radiological investigations are key to diagnosis, as this condition can clinically mimic other gastrointestinal or cardiorespiratory conditions.
Keywords
Barium meal
Computed tomography
Intrapericardial diaphragmatic hernia
INTRODUCTION
Intrapericardial diaphragmatic hernia (IPDH) is a rare condition characterized by herniation of abdominal contents into the pericardial cavity, most commonly through a defect in the central tendon of the diaphragm. It can be traumatic, congenital, or very rarely iatrogenic. It is a rare complication of diaphragmatic rupture, occurring in <1% of cases. Congenital IPDH occurs due to developmental abnormality of the retrosternal septum transversum and is commonly encountered in children; however, they can be asymptomatic until adulthood. IPDH often presents with non-specific cardiorespiratory or gastrointestinal symptoms in adults. Timely diagnosis and intervention are necessary to avoid complications such as life-threatening necrosis, perforation of the herniated contents, and cardiac tamponade. The current patient is a 62-year-old male with a known case of chronic renal disease, presented with non-specific respiratory symptoms and was diagnosed to have IPDH on radiological investigations.
CASE REPORT
A 62-year-old male was referred to our institution with suspected sepsis and a history of cough, dyspnea, and fever for 4 days. The patient was a known case of chronic kidney disease on regular dialysis. On clinical evaluation, the patient was conscious and oriented. He was tachypneic (24 min) with oxygen saturation of 92% on room air. The patient exhibited fever (99.0°F), tachycardia (112 bpm), and low blood pressure (100/80 mmHg).
Posteroanterior chest radiograph [Figure 1] demonstrated an enlarged cardiac silhouette with airlucencies projecting over the cardiac shadow obliterating the left and right cardiac borders. A sharp interface with the adjacent lung was seen. Barium meal study [Figure 2] revealed herniation of the stomach into the thoracic cavity with the lateral view confirming its anterior location ruling out hiatal hernia. Herniated stomach showed organoaxial position without volvulus. Non-opacified small bowel loops were seen adjacent.
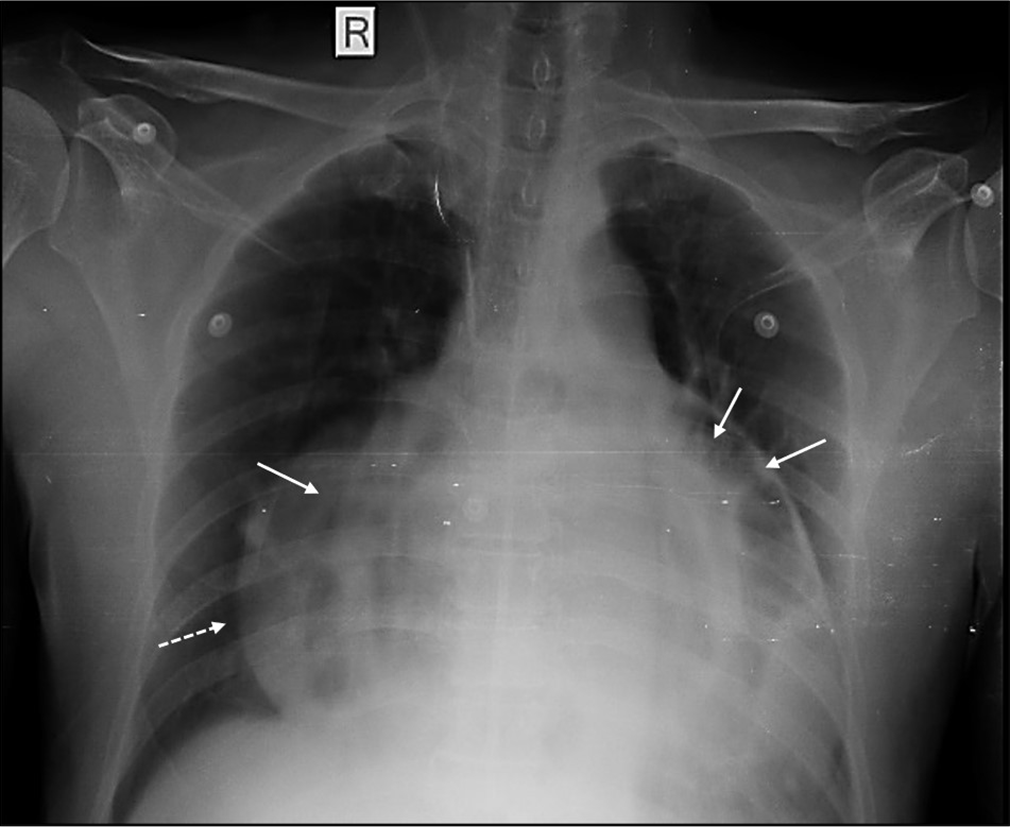
- Posteroanterior chest radiograph showing enlarged cardiac silhouette with air-filled bowel loops projecting over the heart and superimposing the left and right cardiac borders (white arrows). Note sharp interface with the lung (white dotted arrow). R: Right.
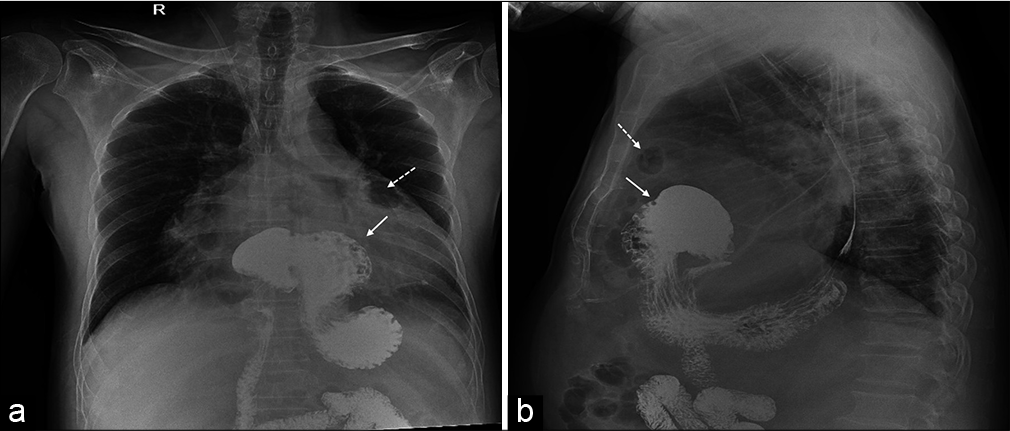
- (a) Anteroposterior and (b) lateral views of upper gastrointestinal barium study showing supradiaphragmatic location of the stomach (solid white arrows) in the anterior mediastinum along with air-filled bowel loops (white dashed arrows).
Plain computed tomography (CT) study of the chest and upper abdomen [Figure 3] confirmed the presence of stomach and bowel loops herniating into the pericardial cavity. The contents were lined by smooth pericardium compressing and displacing the heart toward the left. Communication of bowel loops with the peritoneal cavity was seen, with no evidence of obstruction.
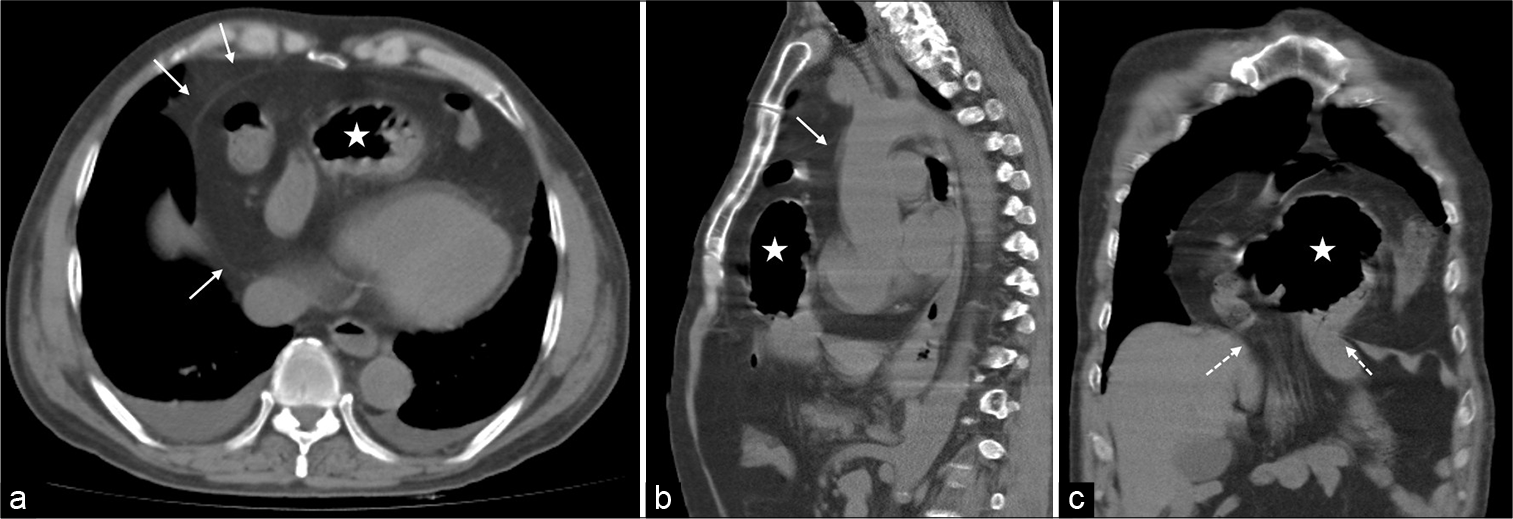
- (a) Axial (b) sagittal and (c) coronal images of non-contrast computed tomography study of chest and upper abdomen shows the presence of air-filled stomach (white stars) and bowel loops herniating anterior to the cardia (Ca) lined by smooth pericardial layer (solid white arrows). Dashed white arrows demonstrate the central tendon defect.
The patient denied any history of prior trauma or surgery. A diagnosis of adult presentation of congenital IPDH was made. Surgical repair of the IPDH was recommended, but the patient refused intervention. He was subsequently explained with possible complications in the future and discharged following medical management.
DISCUSSION
IPDH is an abnormal communication between the peritoneal cavity and the pericardium and is also referred to as peritoneopericardial diaphragmatic hernia.[1,2] It is the rarest type of non-hiatal diaphragmatic hernia[3] whose prevalence is unknown with only few case reports available in the literature. IPDH can occur from a traumatic or congenital diaphragmatic defect of the pericardial portion of the central tendon [Figure 4] or can be iatrogenic.[4] They usually present with non-specific cardiorespiratory or gastrointestinal complaints that can delay the diagnosis.[5,6] In adults, the presentation can be variable, from being asymptomatic to being symptomatic with associated complications, including visceral strangulation, ischemic bowel, or cardiac tamponade, indicating emergency intervention.[7] The time interval from the presumed origin of the IPDH to the time of diagnosis is quite variable for both traumatic and congenital etiologies.
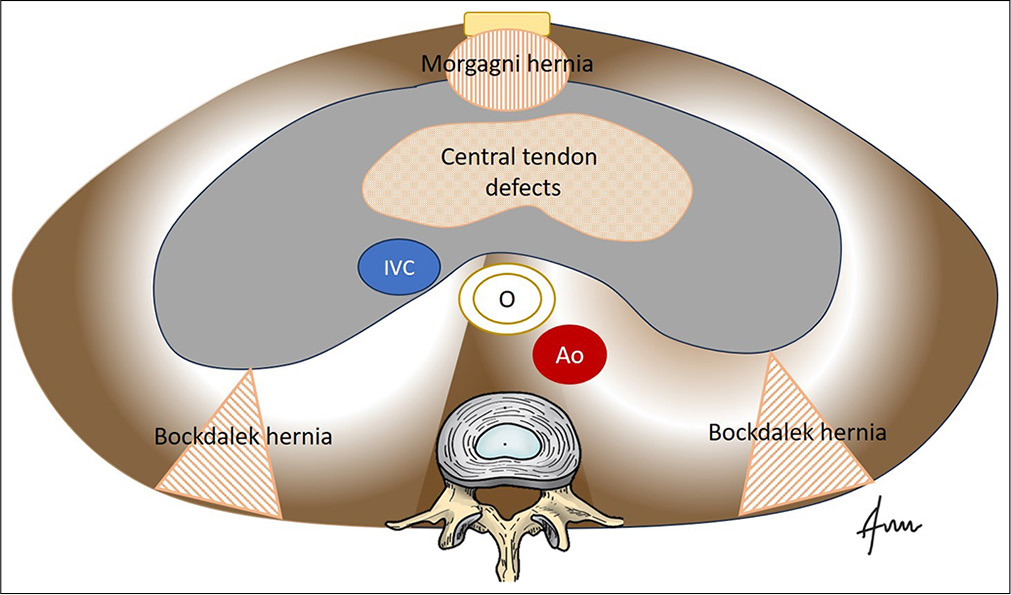
- Illustration depicting the embryology of diaphragm with various hernial sites. IVC: Inferior vena cava, O: Oesophagus, Ao: Aorta.
Traumatic herniation usually results from a high-force blunt injury or penetrating trauma to the chest or abdomen.[8] A sudden rise in intra-abdominal pressure during blunt abdominal trauma results in diaphragmatic rupture that extends into the pericardium.[9] Since the pericardial diaphragm is a single, tightly fused layer, a laceration affects its entire thickness, permitting herniation without a sac.[8]
Congenital IPDH occurs due to a developmental failure of the septum transversum, creating a pericardio-peritoneal defect.[3,10] They can be highly symptomatic in newborns, with severe respiratory distress and cyanosis secondary to massive pleural effusion or pulmonary hypoplasia.[10] Congenital lesions may remain unnoticed and can manifest in adulthood[1,2] and hence, the lack of a history of trauma should not rule out IPDH.[8]
The key to diagnosis is a high index of suspicion coupled with the appropriate investigations. A chest X-ray in frontal and lateral views is used as the initial diagnostic tool, which reveals an enlarged cardiac silhouette due to extraneous bowel gas and heterogeneous opacities overlying the cardiac shadow depending on the abdominal content. The upper gastrointestinal barium study demonstrates opacification of intrapericardial bowel loops located anteriorly within the confines of cardiac shadow; however, the diagnosis can remain unclear if only the omentum is herniated.[8] A CT scan is the most effective imaging technique for visualizing the herniated contents. The key to diagnosis is the demonstration of the pericardium surrounding the contents and mass effect on the cardiac structures. CT scan also aids in the diagnosis of associated complications which include strangulation resulting in perforation pericarditis, cardiac tamponade, and acute respiratory distress.
A close differential of IPDH is Morgagni’s hernia, where the abdominal contents herniate into the anterior mediastinum through a congenital defect in the diaphragm known as the foramen of Morgagni [Figure 5]. It can be distinguished from IPDH by its lack of conformity with the pericardium.[8] Bochdalek hernias occur in the posterolateral aspect of the diaphragm commonly on the left side sparing the central portion and do not show continuity with the pericardial cavity. Hiatal hernias are posterior and central secondary to enlargement of the diaphragmatic hiatus and generally contain stomach as sliding or para esophageal presentations.
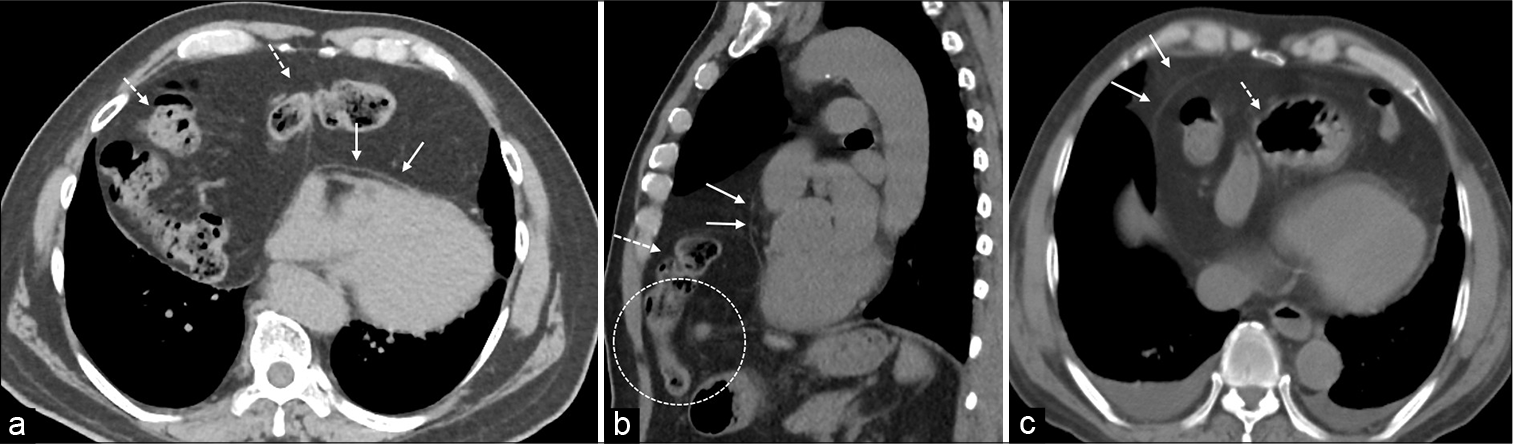
- Plain computed tomography (a) axial and (b) sagittal section in a patient with Morgagni hernia demonstrating herniation of bowel (dashed white arrows) into the chest through the foramen of Morgagni (white circle). Note the herniation is anterior to the pericardium (solid white arrows). (c) In contrast to intrapericardial hernia where the contents (dashed white arrow) are within pericardium (solid white arrows)
Prompt surgical reduction is mandatory to prevent secondary complications. A thoracic approach is recommended by most authors in cases of delayed IPDH, as this allows for easier removal of pericardial adhesions, whereas a transabdominal approach is preferred for surgical closure in acute presentations to provide good access to the tear in the diaphragm.[8]
DIFFERENTIAL DIAGNOSIS
Table 1 summarizes the differential diagnosis.
| Differential diagnosis | Differentiating features |
|---|---|
| Morgagni hernia | Lack of conformity of the herniated contents to the pericardium. Pneumopericardium after inducing pneumoperitoneum is not seen as in IPDH. |
| Pericardial effusion | Homogenous fluid collection within the pericardium with the absence of abdominal contents. |
| Esophago- pericardial fistula | Disrupted contour of esophageal wall with leak of oral contrast into the pericardial cavity. Pneumopericardium and pneumomediastinum demonstrate a “continuous diaphragm sign” on the chest radiograph. Hydropneumopericardium was also seen. |
| Pericardial cyst | Fluid-filled cystic lesion with smooth borders abutting the pericardium at cardiophrenic angle showing no connection with the abdominal viscera. |
IPDH: Intra pericardial diaphragmatic hernia.
CONCLUSION
IPDH is a rare type of diaphragmatic hernia that should be considered in the differential diagnosis when dealing with cases of anterior diaphragmatic hernia. This condition can be challenging to diagnose, as its clinical symptoms often overlap with those of more common conditions and can be non-specific.
TEACHING POINTS
IPDH is a rare type of non-hiatal hernia, where the abdominal viscera herniates into the pericardial cavity through a defect in the central tendon portion anterior diaphragm.
IPDH can be traumatic, congenital, or rarely iatrogenic. Congenital IPDH usually presents in the perinatal period but can remain variably symptomatic in adults.
Conformity of the herniated contents within the pericardial sac is the key to the diagnosis and differentiates it from Morgagni hernia.
MCQs
-
What is the primary characteristic of an intrapericardial diaphragmatic hernia?
Herniation of abdominal organs through the posterior diaphragm into the pleural cavity
Herniation of abdominal organs into the pericardial sac
Herniation of the heart into the abdominal cavity
-
Herniation of the lungs into the pericardial sac
Answer key: b
-
Which of the following is a potential complication of an intrapericardial diaphragmatic hernia?
Cardiac tamponade
Acute pancreatitis
Gastrointestinal bleeding
-
Pulmonary embolism
Answer key: a
-
What is the most common diagnostic imaging method for detecting an intrapericardial diaphragmatic hernia?
MRI of the heart
Chest X-ray
Abdominal ultrasound
-
Cardiac catheterization
Answer key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Peritoneopericardial diaphragmatic hernia. Ann Surg. 1958;148:798-804.
- [CrossRef] [PubMed] [Google Scholar]
- A case of peritoneo-pericardial diaphragmatic hernia treated surgically. Thorax. 1957;12:68-72.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal Septum transversum diaphragmatic defects. Am J Surg. 1984;147:481-5.
- [CrossRef] [PubMed] [Google Scholar]
- Intrapericardial diaphragmatic hernia into the pericardium after esophagectomy: A case report. Surg Case Rep. 2018;4:94.
- [CrossRef] [PubMed] [Google Scholar]
- Asymptomatic congenital intrapericardial diaphragmatic hernia in a woman becoming symptomatic after childbirth. J Surg Case Rep. 2019;2019:rjz281.
- [CrossRef] [PubMed] [Google Scholar]
- Iatrogenic intrapericardial diaphragmatic hernia diagnosed by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2010;12:3.
- [CrossRef] [PubMed] [Google Scholar]
- Iatrogenic intrapericardial diaphragmatic hernia associated with cardiac tamponade. J Trauma. 2001;50:136-9.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodality imaging of congenital intrapericardial diaphragmatic hernia. Radiol Cardiothorac Imaging. 2024;6:e240137.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-sectional CT of strangulating intrapericardial diaphragmatic hernia. AJR Am J Roentgenol. 2001;177:686-8.
- [CrossRef] [PubMed] [Google Scholar]







