Translate this page into:
Heavy eye syndrome as a cause of recurrent strabismus
*Corresponding author: Cyruz Jan Beltran David, Department of Radiology, University of the Philippines - Philippine General Hospital, Metro Manila, Philippines. cyruzjandavid@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: David CJB, Cayetano CDB, Felizardo RN, Mendoza KIR, Galsim RJG. Heavy eye syndrome as a cause of recurrent strabismus. Case Rep Clin Radiol. 2025;3:29-31. doi: 10.25259/CRCR_92_2023
Abstract
This is the case of a 69-year-old female with strabismus. She had a corrective surgery; however, 20 years later, progressive esotropia and hypotropia occurred. Magnetic resonance imaging (MRI) of the orbits showed increased dislocation angles of the bilateral lateral recti (LR) and superior recti (SR). Both LR-SR bands were not clearly appreciated. Other findings are staphyloma and irregular borders of the medial recti. MRI findings are suggestive of heavy eye syndrome.
Keywords
Heavy eye syndrome
Dislocation angle
Lateral recti and superior recti band
Magnetic resonance imaging
Strabismus
INTRODUCTION
Heavy eye syndrome (HES) or strabismus fixus convergence is a rare cause of acquired esotropia in the setting of high myopia.[1] HES usually presents with diplopia because of progressive esotropia and hypotropia, causing limited eye movements.[2] Imaging is suggested to demonstrate anatomical abnormalities to confirm definite diagnoses and exclude differential diagnoses.[3]
CASE REPORT
A 69-year-old Filipino female presented with progressive esotropia and hypotropia for almost 20 years, accompanied by bilateral poor visual acuity. She noted previous corrective surgery; however, there is a recurrence of signs and symptoms.
Both globes exhibit increased anteroposterior dimension relative to their width with a note of focal bulging of its posterolateral portions [Figure 1a]. These also exhibit severe superotemporal shifts and inferomedial deviations [Figure 1b]. There is apparent superolateral stretching of the intraocular and intraorbital segments of the bilateral optic nerves; these nerves exhibit no gross evidence of atrophy. There is an inferior shift of the lateral rectus muscle and a nasal shift of the superior rectus muscle. The dislocation angle measures 139.5° on the right and 131.3° on the left [Figure 1c]. The bilateral lateral rectus-superior rectus bands are not delineated, maybe severely thinned out. Also peculiar to this case is the wavy contour of the bilateral medial recti [Figure 1d]. The rest of the ocular contents show normal signal characteristics. The orbital apices, optic chiasm, sella, and extrasellar structures appear normal. The imaged cranial nerves are intact.
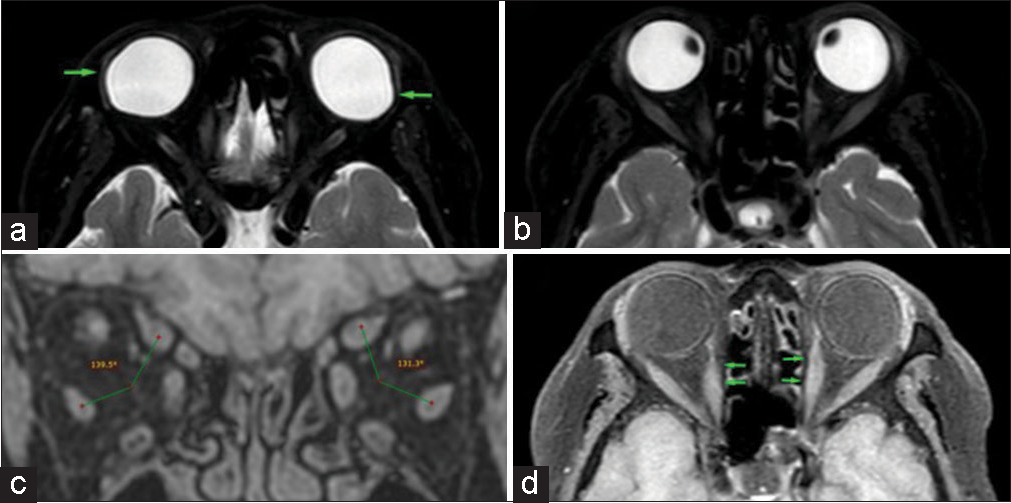
- (a) Axial T2 fat-saturated images show focal bulging of the posterolateral portions of both globes, pointed by the green arrows. (b) These also show the increased anteroposterior dimensions of both globes. (c) Coronal T1 fat saturated image shows the displacement of the superior and lateral recti with resultant increased dislocation angles, bilaterally. (d) Axial T1 DIXON image shows the wavy contours of both medial recti, as pointed by the green arrows.
DISCUSSION
The most recognized pathophysiologic theory of HES is the inferior shift of the lateral rectus muscle and nasal shift of the superior rectus muscle produces an increased dislocation angle.[4] The dislocation angle refers to the angle formed by the centers of the lateral recti (LR) and superior recti (SR) muscles in relation to the globe.[2,4] Resultant limited elevation and depression of the eyes are observed, as well as abduction.
According to previous literature, connective tissues may have a role in the pathogenesis of HES. Like the patients in the study of Maiolo et al., degeneration of the LR-SR band is noted in our patient, suggesting a possible role in the pathogenesis of HES. It has a consequential inferior displacement of the lateral rectus present as esotropia and hypotropia.[4] However, according to Rutar et al., this may not explain severe cases such as in our patient.[1]
The elongation of both globes predisposes their posterior aspects to be dislocated out of their respective muscle cones,[5] explaining their fixed position in our patient.
It is important to note that cranial nerve palsies may present like HES. A previous report states that abducens nerve palsy mimics HES.[6] Otherwise, the imaged cranial nerves are radiologically intact.
With high soft tissue contrast, magnetic resonance imaging (MRI) provides a satisfactory assessment of the abovementioned muscles and connective tissues. Key findings, in this case, are the increased dislocation angle, elongated globes, and thinned-out LR-SR bands, confirming the diagnosis of HES.
DIFFERENTIAL DIAGNOSES
Differential diagnoses for HES are the following: Sagging eye syndrome, cranial nerve palsies, especially abducens nerve, and Graves orbitopathy.
CONCLUSION
Routine orbital and cranial MRI are advised in the assessment of patients with progressive esotropia and hypotropia for adequate evaluation of possible etiologies. In addition, it offers essential pre-operative information, which ultimately benefits possible surgical management.
TEACHING POINTS
MRI is a vital tool in possible cases of HES, for definite diagnosis and satisfactory elimination of differential diagnoses.
Displacement of the superior and lateral recti with resultant increased dislocation angle confirms the diagnosis of HES in patients presenting with progressive esotropia and hypotropia.
LR-SR band degeneration may be a compounding factor in the pathogenesis of HES.
MCQs
-
MRI findings of a patient with esotropia show increased lateral rectus – superior rectus dislocation angle and thinned out LR-SR band. Which among the following is the most possible diagnosis?
Sagging eye syndrome
Abducens nerve palsy
Graves orbitopathy
Heavy eye syndrome
Answer Key: d
-
Which among the following are differential diagnoses of the following?
Sagging eye syndrome
Abducens nerve palsy
Graves orbitopathy
All of the above
Answer Key: d
-
Which of the modalities may offer the most information in the assessment and management of HES?
X-ray
Ultrasound
CT
MRI
Answer Key: d
Declaration of patient consent
Patient‘s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- "Heavy Eye" syndrome in the absence of high myopia: A connective tissue degeneration in elderly strabismic patients. J AAPOS. 2009;13:36-44.
- [CrossRef] [PubMed] [Google Scholar]
- Heavy eye syndrome versus sagging eye syndrome in high myopia. J AAPOS. 2015;19:500-6.
- [CrossRef] [PubMed] [Google Scholar]
- Yokoyama procedure for a woman with heavy eye syndrome who underwent multiple recession-resection operations: A case report. World J Clin Cases. 2022;10:11517-22.
- [CrossRef] [PubMed] [Google Scholar]
- Role of magnetic resonance imaging in heavy eye syndrome. Eye (Lond). 2017;31:1163-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical procedure for correcting globe dislocation in highly myopic strabismus. Am J Ophthalmol. 2010;149:341-6.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Heavy eye syndrome mimicking abducens nerve palsies. Can J Neurol Sci. 2020;47:683-4.
- [CrossRef] [PubMed] [Google Scholar]







