Translate this page into:
Delving into an uncommon etiology of Mammoth ovaries
*Corresponding author: Rupa Renganathan, Division of Breast and Women’s Imaging and Interventions, Department of Diagnostic and Interventional Radiology, Kovai Medical Center and Hospital, Coimbatore, Tamil Nadu, India. drrrupa@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Renganathan R, Kini DV, Subramaniam P, Dhandapani S. Delving into an uncommon etiology of Mammoth ovaries. Case Rep Clin Radiol. doi: 10.25259/CRCR_26_2024
Abstract
Ovarian hyperstimulation syndrome (OHSS) is an unusual clinico-radiological entity with a risk of developing life-threatening complications which have various etiologies. Radiological imaging helps image the typical features of enlarged ovaries and also helps rule out associated complications. Based on the severity of the clinical manifestations and corresponding radiological findings, grading systems have been devised as well. In this case report, we wish to highlight the features of this rare entity, that is, spontaneous OHSS, secondary to primary hypothyroidism in a young female who presented with acute abdomen.
Keywords
Enlarged ovaries
Ovarian hyperstimulation syndrome
Primary hypothyroidism
Ultrasound
Multiple cysts
INTRODUCTION
Ovarian hyperstimulation syndrome (OHSS) is an unusual clinico-radiological entity with a risk of developing life-threatening complications. It is primarily characterized by enlarged multicystic ovaries secondary to stimulation by various iatrogenic and non-iatrogenic triggers. Radiological imaging with various available modalities helps in assessing the primary pathology, its severity, and morphology in addition to ruling out other etiologies. In this case report, we wish to highlight the features of this rare entity, that is, spontaneous OHSS, secondary to primary hypothyroidism in a young female presenting with acute abdomen.
CASE REPORT
A 19-year-old female presented to our outpatient department with complaints of severe abdominal pain and non-projectile vomiting for the past 2 days. Her menstrual cycles were regular. On examination, she was found to have tenderness in the lower abdomen with no obvious mass that was palpable. Systemic examination was otherwise unremarkable and vitals were stable. Following this, in view of the abdominal pain, she was advised to have an ultrasound of the abdomen and pelvis. Ultrasound abdomen and pelvis (performed using GE Voluson E8, USA) demonstrated enlarged bilateral ovaries with multiple unilocular cysts within; no ascites, pleural effusion, or pericardial effusion was seen (the right ovary measured 157 cc and left ovary measured 202 cc) [Figure 1a and b]. Based on the ultrasound findings, a provisional diagnosis of OHSS was made. Corroborative magnetic resonance imaging (MRI) (3.0 T MRI, Siemens Healthineers, Germany) limited sections of the pelvis were performed to rule out ovarian torsion and it depicted and confirmed the ultrasound findings of OHSS with no features of ovarian torsion [Figure 1c]. A provisional diagnosis of spontaneous ovarian hyperstimulation was made and a blood work-up was sent for further detailed analysis. Detailed scrutiny of the patient’s history was done and possible etiologies such as pregnancy and iatrogenic causes such as ovarian stimulant drugs and hormone supplement intake were eliminated. Complete blood counts disclosed no significant abnormality; however, serum hormone level analysis revealed elevated serum estradiol (198.8 pg/mL, normal values 2.5–166 pg/mL), prolactin (121 ng/mL, normal values 0–30 ng/mL), and thyroid-stimulating hormone (TSH) (100 μU/mL, normal values 0.27–4.2 μU/mL) with a severely reduced free thyroxine levels (0.153 ng/dL). Beta-human chorionic gonadotropin (βHCG) levels were also assessed and found to be normal (<0.100 MIU/mL). A diagnosis of spontaneous OHSS secondary to primary hypothyroidism was made on assessment of the serum hormone levels in combination with the sonographic findings. Following this, the patient was then advised of thyroxine supplements (Tab THYRONORM 100 mcg) and was placed on regular follow-up with serial serum TSH level assessment and ultrasound abdomen to assess the ovarian volume. Clinical examination of her thyroid gland revealed diffusely enlarged gland with no obvious nodularity. The TSH levels exhibited a decreasing trend with the last recorded TSH level at 1 year follow-up being 3.44 μU/mL. The ovarian volumes were noted to reduce serially with volumes of 18 cc (right ovary) and 9 cc (left ovary) documented on the 5-month follow-up scan [Figure 2a-d].
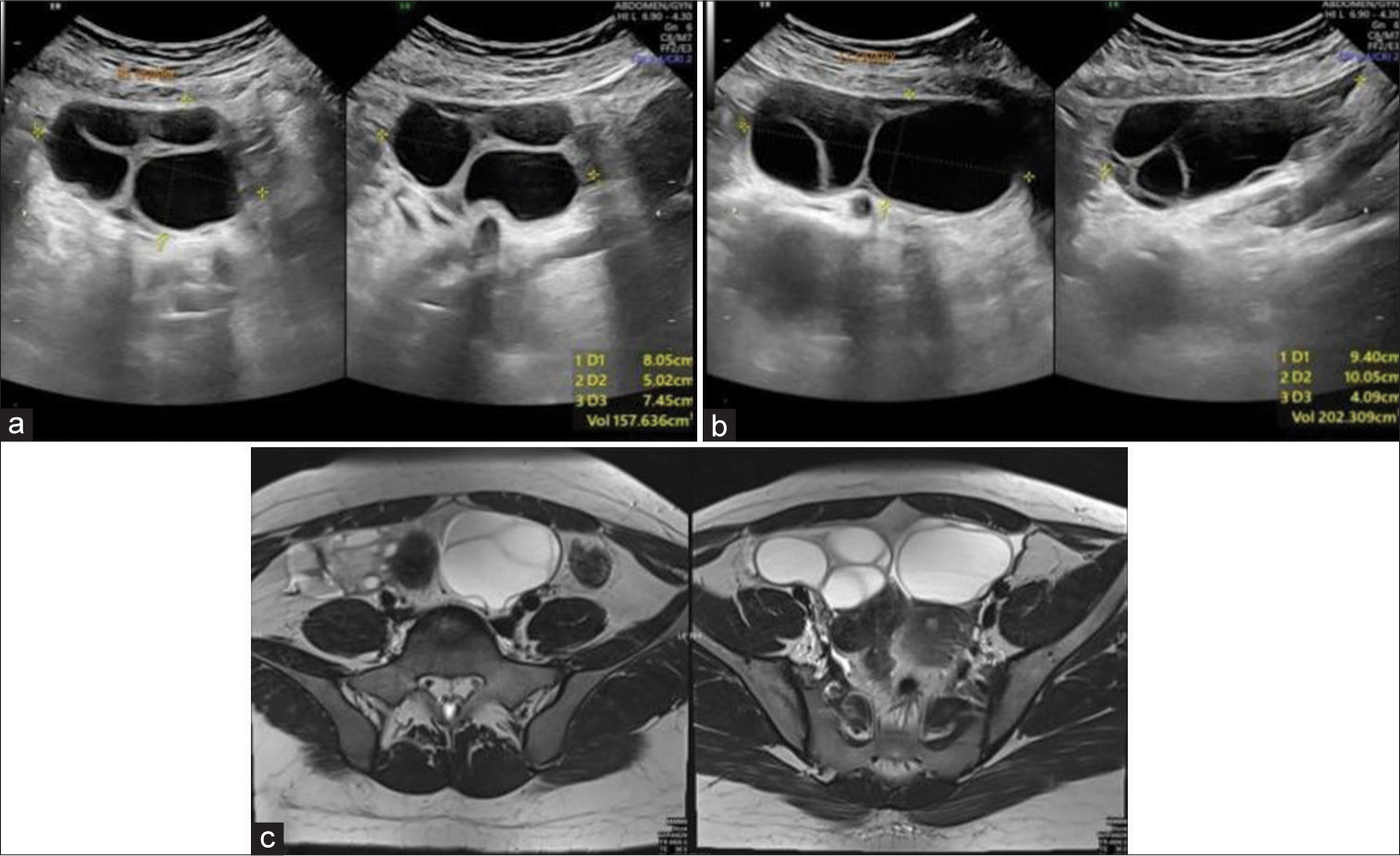
- A 19-year-old female presented with ovarian hyperstimulation syndrome who presented with severe abdominal pain (a and b) ultrasound images showing bulky bilateral ovaries with multiple enlarged follicles and (c) axial T2-weighted magnetic resonance imaging section of the pelvis re-demonstrating the ultrasound findings of bulky ovaries with multiple follicles. No e/o torsion was noted.
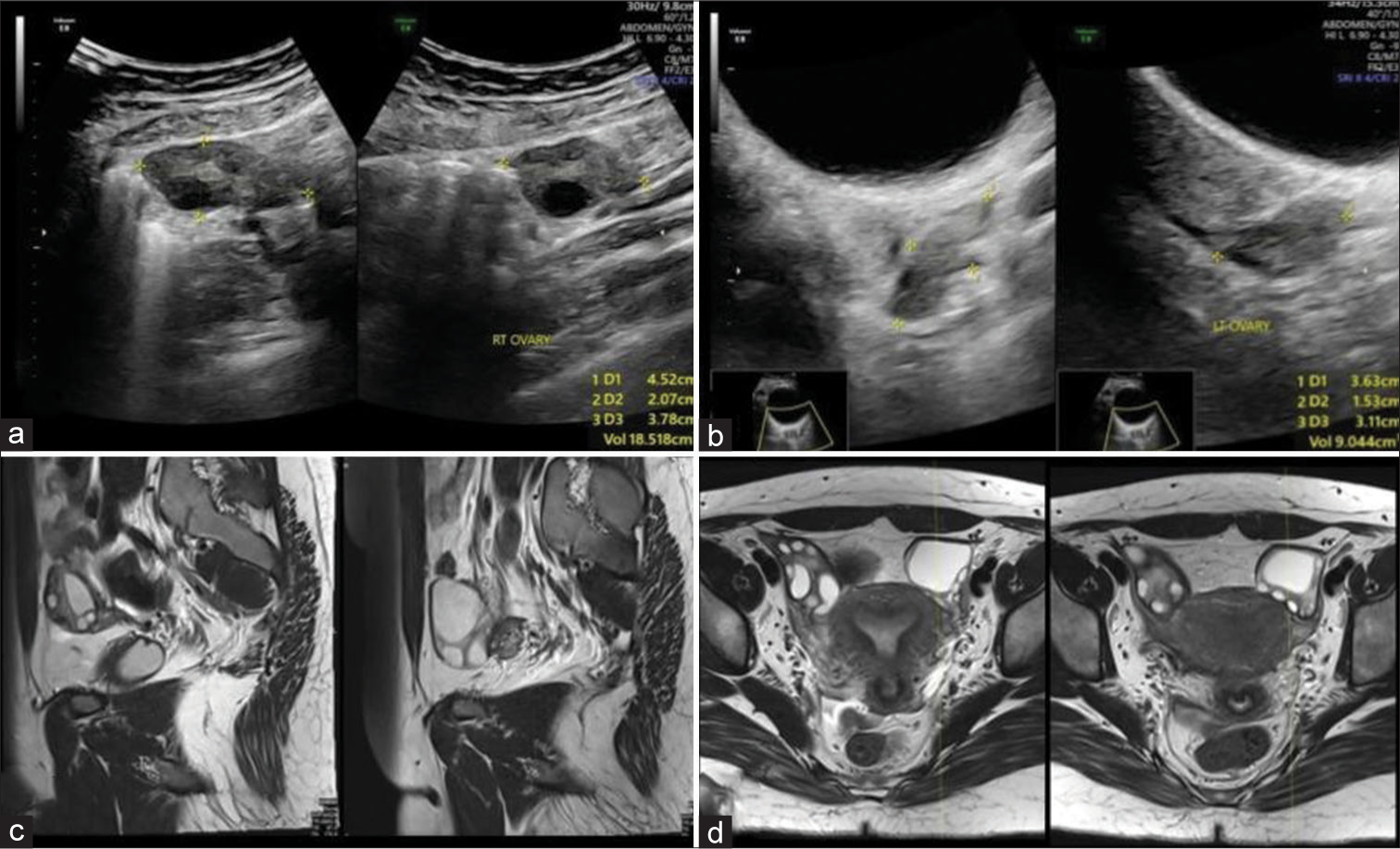
- A 19-year-old female presented with ovarian hyperstimulation syndrome (OHSS) who had presented with severe abdominal pain, diagnosed as OHSS, on follow-up (a and b) Ultrasound images demonstrating the normal size and morphology of both ovaries at 5 month follow-up (c and d) sagittal and axial T2-weighted magnetic resonance imaging section of the pelvis re-demonstrating ultrasound findings suggesting complete resolution.
DISCUSSION
The pathogenesis of OHSS is less-understood and a wide range of hypotheses exist, of which the most accepted is that of the role of glycoprotein hormones as a causative factor in genesis of spontaneous OHSS.[1] Glycoproteins such as serotonin, histamine, and prostaglandins influence the functioning of various existent mediators and vasoactive substances resulting in increased vascular permeability. This subsequently leads to the varied complications of OHSS such as deep vein thrombosis, ascites, pleural effusion, and hypercoagulability. In severe cases, organ dysfunction has also been noted.[2]
Multiple triggers have been noted to be associated with the occurrence of OHSS which may be classified as iatrogenic and non-iatrogenic causes.[1] Most common iatrogenic causes are secondary to ovulation therapy utilized for assisted reproductive techniques while some of the causes for non-iatrogenic causes resulting in spontaneous OHSS are pregnancy-related complications, gestational trophoblastic tumors, pituitary adenomas, and hypothyroidism.[3,4]
The association of OHSS with primary hypothyroidism has been noted in a few cases, such as in the report by Alzebidi et al. Although the pathogenesis of OHSS and its association with hypothyroidism is unclear, few theories in relation to modifications in the hydroxylation pathway and feedback regulation have been noted.[5]
Role of imaging in OHSS is vital with the availability of rapid and accurate modalities such as ultrasonography to make the diagnosis and also to detect its complications.[1] The typical imaging feature is that of enlarged bilateral ovaries with multiple cysts of varying sizes within. The cysts may be secondarily complicated with hemorrhage; however, the presence of solid components or vascularity within the cysts is not seen. In addition, other features such as ascites, pleural effusion, pericardial effusion, and deep vein thrombosis can also be efficiently detected.[1]
Based on the severity of the clinical manifestations and corresponding radiological findings, a grading system has been devised by Golan to categorize OHSS into mild, moderate, and severe [Table 1].[1,6,7] However, based on the etiology of OHSS, the modified Deleneers classification is widely used which was modified by Panagiotopoulou et al. based on the presence of follicle-stimulating hormone receptor (FSHR) mutation and levels of βHCG, TSH, follicle-stimulating hormone, and luteinizing hormone levels [Table 2].[8,9]
| Category | Grade | Clinical Features |
|---|---|---|
| Mild OHSS | Grade 1 | Abdominal distention and discomfort |
| Grade 2 | Grade 1+Vomiting, Nausea+Ovarian size of 5–12 cm | |
| Moderate OHSS | Grade 3 | Mild OHSS+Ascites |
| Severe OHSS | Grade 4 | Moderate OHSS+Pleural/Pericardial effusion |
| Grade 5 | Grade 4+Biochemical imbalance |
OHSS: Ovarian hyperstimulation syndrome
| Modified Deleneers classification | Pathology | Trigger |
|---|---|---|
| I | Mutated FSHR | Pregnancy |
| II | Elevated β-HCG | Multiple pregnancies |
| Gestational trophoblastic disorders | ||
| βHCG secreting tumors | ||
| III | Elevated TSH | Hypothyroidism |
| IV | Elevated FSH/LH | FSH/LH secreting pituitary adenomas |
| Ectopic FSH secreting tumors |
OHSS: Ovarian hyperstimulation syndrome; FSHR: Follicle-stimulating hormone receptor; βHCG: Beta-human chorionic gonadotropin, TSH: Thyroid-stimulating hormone; FSH: Follicle-stimulating hormone; LH: Luteinizing Hormone
An important and clinically similar entity that is imperative to be ruled out is the possibility of ovarian torsion – isolated or superadded. This is a possible complication as well as a close differential and use of ultrasound, an easily accessible tool, helps decipher this. Ovarian torsion in association with OHSS is found to be more commonly seen in pregnancy with an incidence of up to 16%.[10]
OHSS, due to its rarity, is a less understood concept in the medical literature. Moreover, with the increasing number of individuals utilizing assisted reproductive techniques in the present day, its incidence has been noted to be in higher numbers. However, the possibility of the existence of this pathology even in cases not presenting with a typical clinical history is to be made aware to clinicians and radiologists alike as only then will a search for other possible etiologies be made. To conclude, acquiring a detailed history and corroborating it with appropriate imaging techniques and confirmatory hormonal analysis is a necessary prerequisite to any case presenting with suspected OHSS. Thus, the prompt diagnosis of the same by a radiologist is vital in planning early intervention thereby delivering efficient patient care.
DIFFERENTIAL DIAGNOSIS
Although comprising typical imaging features, when cases are of the milder variety few possible differentials [Table 3]:
| Polycystic ovaries |
|
| Ovarian torsion |
|
| Theca lutein cysts associated with GTT |
|
| Mucinous ovarian neoplasm |
|
GTT: Gestational trophoblastic disease, OHSS: Ovarian hyperstimulation syndrome, USG: Ultrasound, MRI: Magnetic resonance imaging, β-HCG: Beta human chorionic gonadotropin
CONCLUSION
Ovarian hyperstimulation syndrome is an entity comprising typical imaging features that warrant an immediate spot diagnosis. Also, as a clinical radiologist, familiarising ourselves with remote causes helps us make a complete diagnosis.
TEACHING POINTS
Enlarged ovaries with multiple cysts are a typical imaging feature of OHSS and should guide a prompt diagnosis from the radiologist. It should also direct them to obtain a detailed history pertaining to the etiological triggers for OHSS.
Thorough assessment of the patient for possible complications related to OHSS such as extravascular fluid accumulation, hypercoagulability, and thromboembolism.
MCQs
-
OHSS is not associated with
Gestational trophoblastic tumors
Pituitary adenomas
Hypothyroidism
Diabetes mellitus
Answer key: d
-
Differential for OHSS is
Polycystic ovaries
Theca lutein cysts associated with GTT
Mucinous ovarian tumors
All the above
Answer key: d
-
Following are the criteria for staging of OHSS
Golan
Modified Deleneers
a and b
None of the above
Answer key: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Radiological illustration of spontaneous ovarian hyperstimulation syndrome. Pol Przegl Radiol Med Nukl. 2015;80:217-27.
- [CrossRef] [PubMed] [Google Scholar]
- New insights in prediction of ovarian hyperstimulation syndrome. Acta Clin Croat. 2011;50:281-8.
- [Google Scholar]
- Spontaneous ovarian hyperstimulation syndrome (OHSS): A rare but important differential diagnosis for abdominal distension in early pregnancy. J Obstet Gynaecol. 2011;31:338-9.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous ovarian hyperstimulation syndrome and pituitary adenoma: Incidental pregnancy triggers a catastrophic event. Fertil Steril. 2009;92:390.e1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous ovarian hyperstimulation syndrome associated with primary hypothyroidism. Cureus. 2023;15:e33247.
- [CrossRef] [PubMed] [Google Scholar]
- Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS) Hum Reprod Update. 2003;9:77-96.
- [CrossRef] [PubMed] [Google Scholar]
- Ovarian hyperstimulation syndrome: An update review. Obstet Gynecol Surv. 1989;44:430-40.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of the first germline mutation in the extracellular domain of the follitropin receptor responsible for spontaneous ovarian hyperstimulation syndrome. Hum Mutat. 2008;29:91-8.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous ovarian hyperstimulation syndrome: Case report, pathophysiological classification and diagnostic algorithm. Eur J Obstet Gynecol Reprod Biol. 2013;169:143-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ovarian torsion due to ovarian hyperstimulation syndrome diagnosed by sonographic whirlpool sign in the first trimester of pregnancy: A case report. Radiol Case Rep. 2023;18:3386-9.
- [CrossRef] [PubMed] [Google Scholar]








