Translate this page into:
Decoding the dilemma of antenatal ventral body wall defects: A case report and literature review
*Corresponding author: Chandan Kumar Pal, Department of Radio-diagnosis, University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, Delhi, India. drchandanpal93@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta A, Pal CK, Prakash S, Bhatt S. Decoding the dilemma of antenatal ventral body wall defects: A case report and literature review. Case Rep Clin Radiol. doi: 10.25259/CRCR_12_2024
Abstract
We are presenting the case of a rare fetal polymalformative syndrome known as the limb body wall complex (LBWC) and its antenatal diagnosis. The level II Anomaly ultrasound of a primigravida female detected exencephaly, thoracoabdominoschisis, club foot, kyphoscoliosis, fetoplacental adherence, and a deficient umbilical cord, classically described in LBWC. It is imperative for radiologists to be familiar with this rare fatal entity of sporadic occurrence and to differentiate it from other non-lethal counterparts for appropriate maternal counseling and timely termination of pregnancy.
Keywords
Limb body wall complex
Body stalk anomaly
Exencephaly
Thoracoabdominoschisis
Club foot
INTRODUCTION
Limb body wall complex (LBWC) also known as Body Stalk anomaly was first described by Van Allen et al. in 1987.[1] It is characterized by severe body-wall defects with evisceration of the organs caused by the failure to form a body stalk.[2] It is a rare disorder with very few reported cases worldwide. It is universally fatal and termination of pregnancy is the mainstay, thus necessitating antenatal ultrasound and early recognition.
CASE REPORT
We are reporting the case of a 31-year-old lady who visited our antenatal ultrasound clinic for a level II ultrasound at a period of gestation of 21 weeks and 5 days. The patient was unable to conceive for 6 years post-marriage and was undergoing treatment for primary infertility. Medical history was significant for hypothyroidism, controlled on medication. She had a past surgical history of undergoing laparoscopic ovarian cystectomy in 2011 and was asymptomatic thereafter. Menstrual history was unremarkable. The patient was a non-smoker and non-alcoholic. The current precious pregnancy was conceived as a result of ovulation induction. She was simultaneously taking Ayurvedic medicines. The patient underwent a first-trimester ultrasound from an outside center at a period of gestation of 11 weeks which showed a single live intrauterine fetus with a crown-rump length of 42.9 mm corresponding to 11 weeks. Cardiac activity was present. No other information was provided. A consequent second trimester Level II anomaly scan was performed at our outpatient antenatal clinic which revealed the following findings:
The ultrasound showed a live fetus with cardiac activity and a femoral length corresponding to 20 weeks and 5 days. The calvarial bones were absent and the cerebral tissue was herniating and exposed to the amniotic fluid suggesting exencephaly [Figure 1a]. No facial cleft defect was seen in our case [Figure 1b]. A similar bulging and protrusion of the heart and abdominal organs (liver, stomach bubble, and intestinal loops) was seen with visualization of a membrane covering it [Figure 1c and d]. There was no amniotic fluid between the membrane and the placenta which raised suspicion for an abnormal fetoplacental adherence [Figure 1c and d green arrow]. An umbilical cord could not be visualized with the possibility of it being either deficient or absent. The spinal curvature was grossly abnormal and suggestive of kyphoscoliosis [Figure 2a]. One of the lower limbs showed a club foot [Figure 2b]. Such a constellation of findings was highly rare and classical for LBWC. After proper maternal counseling, a medical termination of pregnancy was performed by the obstetrician. Postnatal images of the stillborn fetus confirmed our antenatal sonographic findings [Figure 3].

- Antenatal sonographic images (a and b) show absence of cranial bones and cerebral tissue exposed to the amniotic fluid (red arrows). Note the bilateral normal orbits and absence of facial defects. Antenatal sonographic image (c) shows a large ventral wall defect with herniation of heart (red arrow) and liver (blue arrow). Also note the thin membrane covering the herniated organs (white arrow) and the site of suspicious abdominal-placental adherence (green arrow). Antenatal sonographic image (d) shows same ventral wall defect at a different angle showing herniated stomach bubble (pink arrow), small intestine (yellow arrow). Also note the thin membrane covering the herniated organs (white arrow) and the site of suspicious abdominal-placental adherence (green arrow).
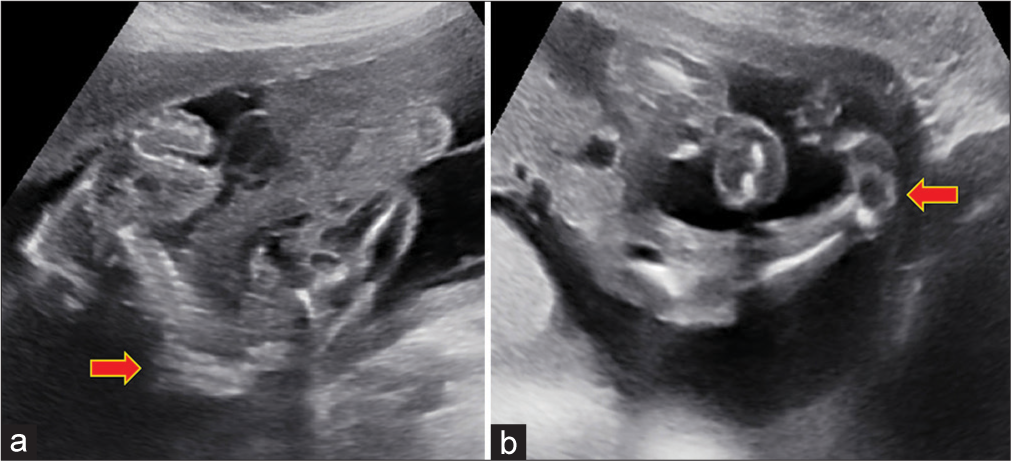
- Antenatal sonographic image (a) shows an intrauterine fetus with abnormal kyphoscoliotic spinal curvature (red arrow). Antenatal sonographic image (b) shows the foot of the fetus showing medial inversion and plantar flexion suggestive of club foot (red arrow).
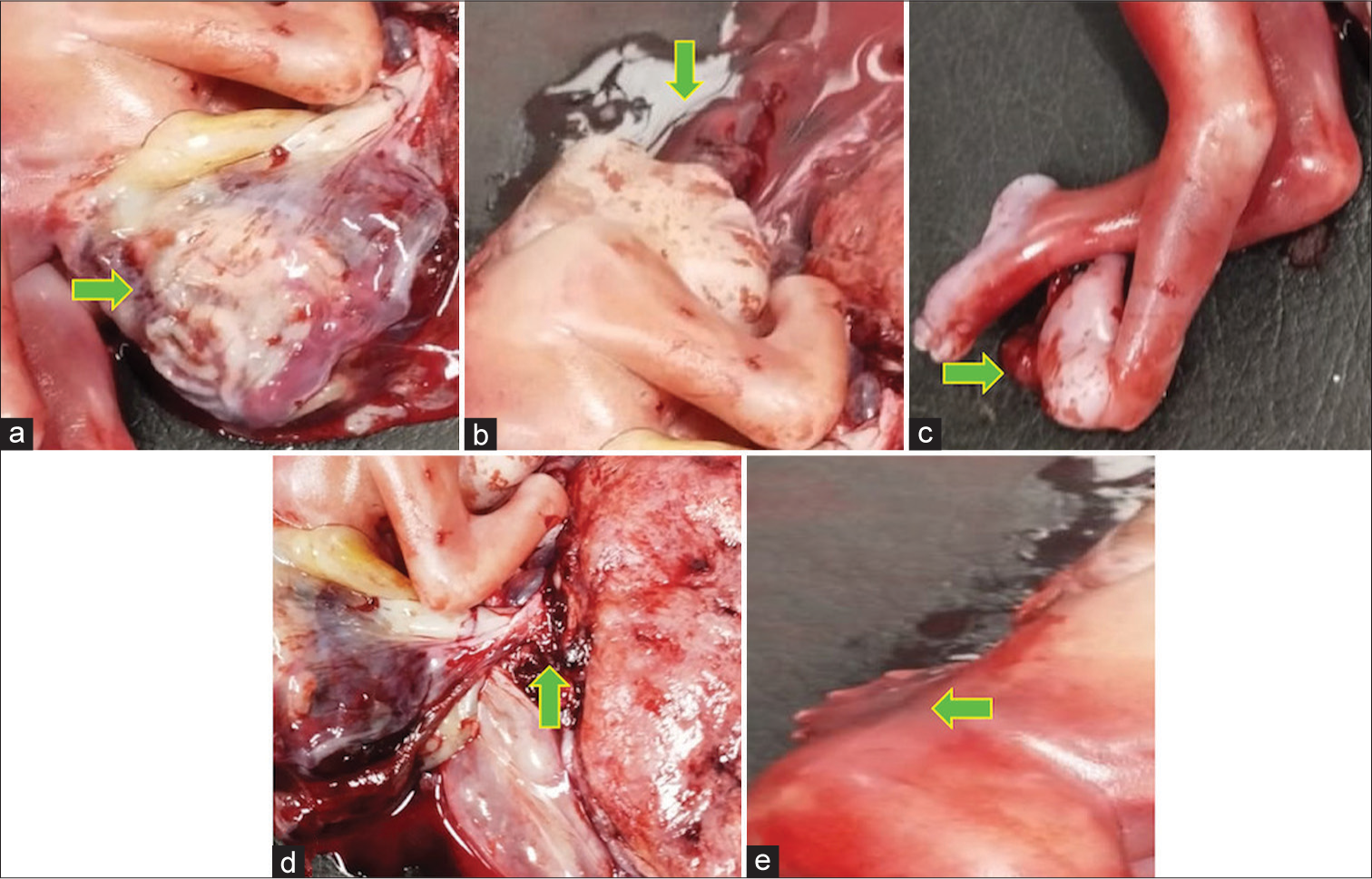
- Postnatal images of the stillborn show (a) a large left sided ventral wall defect with eviscerated organs covered by a thin membrane(green arrow); (b) absence of cranial bones and herniated cerebral tissue (green arrow); (c) club foot in one of the lower limbs (green arrow); (d) abnormal adherence between the herniated viscera and the placenta with a very short/deficient umbilical cord (green arrow); and (e) an abnormal kyphoscoliotic spinal curvature (green arrow).
DISCUSSION
LBWC, also known as Body Stalk anomaly, is a rare fetal polymalformative disorder first described by Van Allen et al.[1] in 1987. It is a sporadic fatal disorder with a reported prevalence of 0.12 cases/10,000 births (including both live and stillbirths).[3] The etiology is not known and no genetic abnormality has been identified.[4] There is no sex or familial predilection or known recurrence risk.[5,6] Extremely elevated levels of alpha fetoprotein have been reported.[7] Because LBWC is incompatible with life, early diagnosis is crucial for parental counseling and timely termination of pregnancy.
Various theories exist regarding the pathogenesis of body stalk anomaly; with the most plausible one attributing it to aberrant lateral body folding, leading to the non-formation of the coelom. Consequently, the abdominal wall fails to develop, leaving the peritoneal cavity exposed to the extraembryonic coelom, and the fetus becomes attached to the placenta. In addition, the failure of body stalk fusion is associated with a shortened or absent umbilical cord.[8,9]
Several classification systems have emerged, with the conventional diagnostic Van Allen et al. criteria[1] relying on the identification of two out of three specific anomalies: (1) Exencephaly or encephalocele accompanied by facial clefts, (2) thoraco and/or abdominoschisis, and (3) limb defects. Limb anomalies can include club foot, polydactyly, syndactyly, oligodactyly, brachydactyly, and amelia.[8] A conundrum of other findings such as severe kyphoscoliosis, short/absent umbilical cord, single umbilical artery, and abnormal fetoplacental adherence are associated with this disorder.[2,5] Death is usually due to severe pulmonary hypoplasia and respiratory failure.[5]
Whenever an evisceration of intra-abdominal contents is encountered while doing an antenatal ultrasound, the search for an associated syndrome should begin. Given the considerable overlap of this syndrome with other lethal and non-lethal ventral abdominal wall defects, it is imperative to be familiar with the differentials of this entity, as shown in Table 1.[3,10]
| Classical features | Differentiating features | |
|---|---|---|
| LBWC | Presence of 2/3 according to Van Allen Criteria: Exencephaly or encephalocele with facial clefts Thoraco and/or abdominoschisis Limb defects |
VWD is left lateral in most cases Adherence of fetal abdominal structures to placenta Scoliosis is universally present Pulmonary hypoplasia Short/absent umbilical cord High incidence of a single umbilical artery |
| Pentalogy of Cantrell | Ventral wall defect Ectopia cordis Diaphragmatic hernia Pericardial defects Structural heart defects such as VSD, ASD, and TOF |
Supraumbilical defect Craniofacial and limb abnormalities +/− Scoliosis +/− |
| OEIS complex | Omphalocele Exstrophy of bladder Imperforate anus Spina bifida |
Infraumbilical defect Absence of intrapelvic bladder MRI may be required for visualization of anal orifice and genital structures. Craniofacial abnormalities/limb defects are not described. |
| Amniotic band syndrome | Amniotic bands Limb abnormalities like amputated digits |
Less commonly involves externalization of thoracoabdominal contents Umbilical cord and vessels are normal |
| Omphalocele | Membrane-covered herniation of intra-abdominal viscera into the base of the umbilical cord | Defect is midline Usually associated with other congenital abnormalities |
| Gastroschisis | Paraumbilical defects with herniation of free-floating viscera | Defect is usually right sided No covering membrane Usually isolated defect |
LBWC: Limb body wall complex, MRI: Magnetic resonance imaging, VSD: Ventricular septal defect, ASD: Atrial septal defect, TOF: Tetralogy of Fallot, VWD: Ventral wall defect
Although omphalocele, ectopia cordis, exencephaly, and club foot, can also be seen in Pentalogy of Cantrell, the presence of adherence of fetal abdominal structures to the placenta helped us to reach the diagnosis of LBWC with certainty. Furthermore, the presence of a deficient umbilical cord in our case helped us to rule out amniotic band syndrome, another differential of LBWC which shows a normal umbilical cord.[3,10]
CONCLUSION
LBWC is a rare polymalformative abnormality comprising of thoraco and/or abdominoschisis, spinal and limb deformities with abnormal fetoplacental adherence, and a short/absent umbilical cord. Given its fatal nature and poor outcome, it is prudent for both radiologists and obstetricians to be familiar with this entity for appropriate parental counseling and timely intervention.
TEACHING POINTS
LBWC is one differential to be considered whenever abdominoschisis is encountered on antenatal ultrasound
Two/three criteria should be met: exencephaly with or without craniofacial defects, thoraco and/or abdominoschisis, and limb abnormalities
Associated commonly encountered anomalies include kyphoscoliosis, single umbilical artery, short/deficient umbilical cord, and abnormal fetoplacental adhesion.
MCQs
-
Which of the following is not a diagnostic criterion for diagnosing limb body wall complex?
Exencephaly
Thoraco/abdominoschisis
Kyphoscoliosis
Club foot
Answer Key: c
-
Which of the following syndrome complex is always associated with an infra umbilical ventral wall defect?
Pentalogy of Cantrell
OEIS Complex
Limb body wall complex
Gastroschisis
Answer Key: b
-
Which of the following is not seen in Pentalogy of Cantrell?
Pericardial defects
Diaphragmatic hernia
Fetoplacental adherence
Structural heart defects
Answer Key: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Limb body wall complex: I. Pathogenesis. Am J Med Genet. 1987;28:529-48.
- [CrossRef] [PubMed] [Google Scholar]
- Complex abdominal wall defects: Appearances at prenatal imaging. Radiographics. 2015;35:636-49.
- [CrossRef] [PubMed] [Google Scholar]
- Limb body wall complex in a still born fetus: A case report. Cases J. 2008;1:86.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal sonographic diagnosis of limb body wall complex: A rare lethal fetal anomaly. Sahel Med J. 2019;22:226.
- [CrossRef] [Google Scholar]
- Limb-body wall complex: A compound anomaly pattern in body-wall defects. Pediatr Surg Int. 2001;17:486-90.
- [CrossRef] [PubMed] [Google Scholar]
- Limb body wall complex. Med J Armed Forces India. 2004;60:77-80.
- [CrossRef] [PubMed] [Google Scholar]
- Prenatal diagnosis of body stalk complex: A rare entity and review of literature. Indian J Radiol Imaging. 2015;25:67-70.
- [CrossRef] [PubMed] [Google Scholar]
- Body stalk anomaly diagnosed in the 2nd trimester. Fetal Diagn Ther. 2003;18:342-4.
- [CrossRef] [PubMed] [Google Scholar]
- An algorithmic approach to complex fetal abdominal wall defects. AJR Am J Roentgenol. 2020;214:218-31.
- [CrossRef] [PubMed] [Google Scholar]








