Translate this page into:
Decoding chronic subcutaneous mysteries
*Corresponding author: Seetharaman Cannane, Department of Radiology, Kovai Medical Center and Hospitals, Coimbatore, Tamil Nadu, India. drcseetharaman@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gomathy B, Sugumar R, Cannane S. Decoding chronic subcutaneous mysteries. Case Rep Clin Radiol. doi: 10.25259/CRCR_63_2024
Abstract
Phaeohyphomycosis, a fungal infection caused by dematiaceous fungi, presents diagnostic challenges due to clinical similarity with other conditions. Advanced imaging, especially magnetic resonance imaging, is crucial for assessing tissue involvement. This report highlights a case of subcutaneous phaeohyphomycosis, emphasizing the importance of multimodal diagnostics including histopathology and culture. In this case report, we wish to highlight the features of this rare entity in a 41-year-old male who presented with the left knee swelling with multiple draining sinuses and nodules for the past 6 months.
Keywords
Subcutaneous abscess
Phaeohyphomycosis
Dematiaceous fungi
INTRODUCTION
Phaeohyphomycosis is a rare infection caused by dematiaceous fungi, involving the skin and subcutaneous tissue, paranasal sinuses, eyes, bones, or central nervous system. Skin and subcutaneous tissue involvement is termed subcutaneous phaeohyphomycosis and is characterized by papulonodules, verrucous, hyperkeratotic or ulcerated plaques, cysts, abscesses, pyogranuloma, non-healing ulcers, or sinuses.[1] Subcutaneous infections typically occur over the exposed areas of the body especially the extremities fingers, wrist, knees, or ankles resulting from traumatic inoculation.
CASE REPORT
A 41-year-old male presented with complaints of the left knee swelling with multiple draining sinuses and nodules around left knee for the past 6 months. No history of trauma or any other complaints were reported. The patient was evaluated with ultrasound and magnetic resonance imaging (MRI) of the left lower extremity (MRI).
Ultrasonography of knee revealed [Figure 1] multiloculated hypoechoic collection with mobile internal echoes, increased posterior acoustic enhancement and increased vascularity in the walls.
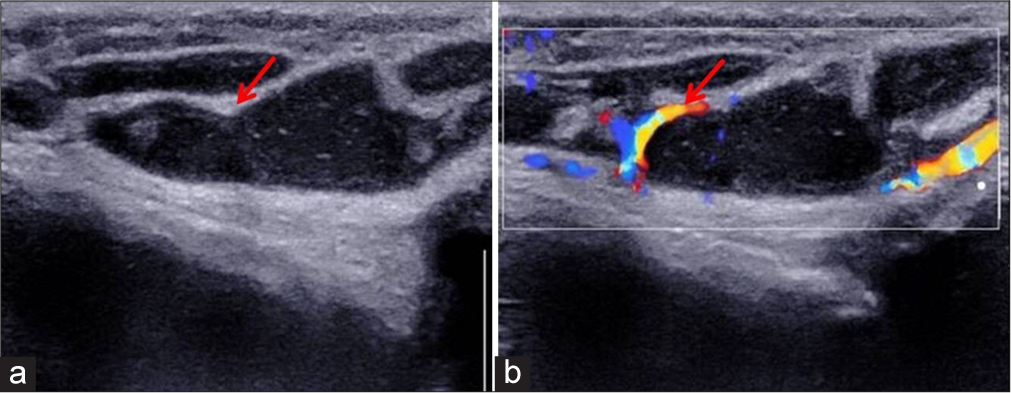
- A 41-year-old male with complaints of the left knee swelling with multiple draining sinuses and nodules for the past 6 months. Ultrasonography of the left knee. (a) Transverse sonogram of the knee showing multiloculated hypoechoic collection with mobile internal echoes and increased posterior acoustic enhancement (red arrow). (b) Color Doppler image showing appreciable vascularity in the walls (red arrow).
MRI of knee revealed [Figure 2] an extensive multiloculated collection in the subcutaneous plane of lower-half of thigh and knee regions. It appears predominantly hyperintense in T2 and hypointense on T2-weighted images and shows significant diffusion restriction on diffusion weighted image (DWI). Post-contrast subtracted images revealed smooth enhancement of the walls. No evidence of deeper extension to bone or joint space was seen. No imaging features of myositis/osteomyelitis/infective arthritis.
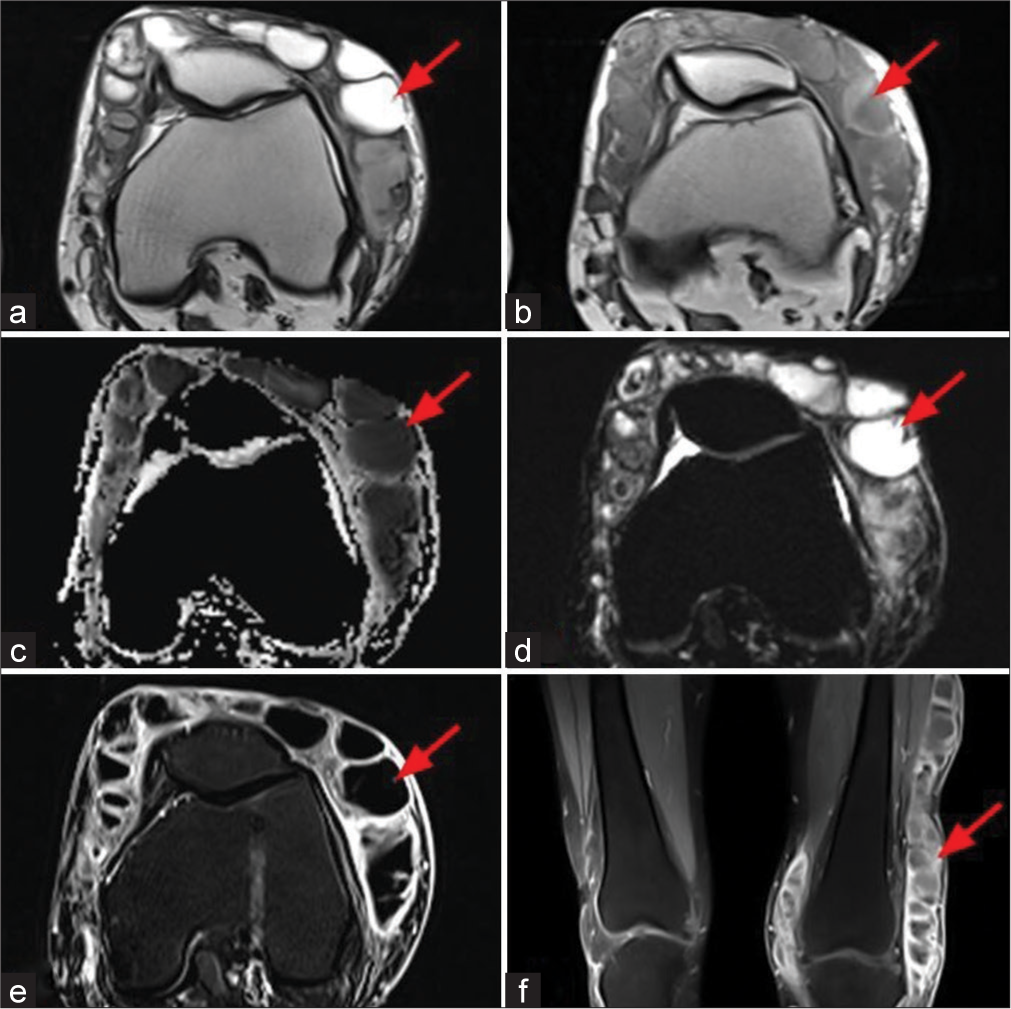
- A 41-year-old male with complaints of the left knee swelling with multiple draining sinuses and nodules for the past 6 months, (a and b) T2-weighted axial and T1-weighted axial MR images show an extensive T2 hyperintense/hypointense and T1 hypointense multiloculated collections in subcutaneous plane of lower thigh and knee regions (red arrows), (c and d) Apparent diffusion coefficient and diffusion-weighted image shows significant diffusion restriction (red arrows) (e and f) subtracted and post contrast T1 fat-saturated images show smooth thin peripheral enhancement (red arrows).
Based on these imaging features, chronic infective etiology with differential diagnosis of cutaneous actinomycosis/nocardiosis/tuberculosis was made. The patient was evaluated further with excision biopsy from the skin and knee lesion. Histopathological examination (HPE) images [Figure 3] revealed features of subcutaneous abscess cavity lined by granulation tissue, special stain for fungus showed thin septate fungal hyphae consistent with subcutaneous mycosis - phaeohyphomycosis.
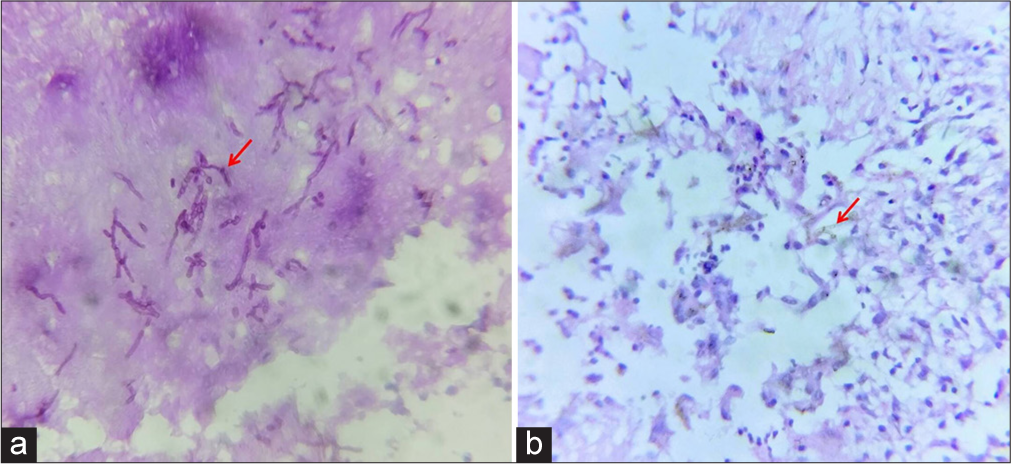
- Histopathology image (a) periodic acid Schiff stain shows thin septate fungal hyphae (red arrow) and (b) high-power view shows brown pigmented thin septate fungal hyphae (red arrow).
The patient was treated with extensive debridement of the left thigh and knee.
DISCUSSION
Phaeohyphomycosis is caused by dematiaceous (pigmented) fungi which contain melanin in their cell walls and grows in tissues in the form of dark-walled septate mycelium. Melanin is the virulence factor in these fungi, it acts by inhibiting phagocytosis.[2] The infections due to dematiaceous fungi are classified into two groups based on the morphology in tissues, chromoblastomycosis (which present as muriform bodies in tissues), and phaeohyphomycosis (which present as hyphae or yeast cells or both without any muriform body in tissues).[3] They are sometimes indistinguishable from a condition called mycetoma also known as “Madura foot.” Mycetoma is a localized chronic, suppurative infection affecting skin, subcutaneous tissue, and bones caused by either bacteria (actinomycetoma) or fungi (eumycetoma).
The etiological agents of phaeohyphomycosis include various dematiaceous hyphomycetes belonging to different orders such as Chaetothyriales (Exophiala, Phialophora, and Cladophialophora) and Pleosporales (Bipolaris, Exserohilum, Curvularia, and Alternaria).[4] Identifying the specific agent has therapeutic importance as different species may have tropism for different organs with varying response to antifungals.
The clinical presentation ranges from solitary cutaneous nodules to deep subcutaneous abscess. The subcutaneous infections typically occur on the exposed areas of the body, especially the extremities, fingers, wrists, knees, or ankles, resulting from traumatic inoculation.[5]
It is essential to distinguish this from conditions such as chromoblastomycosis, mycetoma, ganglion cysts, epidermal inclusion cysts, Baker’s cysts, erythema nodosum, and lipomas. This distinction can be achieved through evaluating clinical presentation, followed by histopathology and culture sensitivity.[6]
Subcutaneous abscess are usually diagnosed clinically and do not routinely require any imaging. In complex cases where possible radical surgical treatment is being considered, imaging may be undertaken to determine the extent of soft-tissue involvement. MRI is the preferred modality for the evaluation of more deep soft-tissue abscesses.
Ultrasound is useful for differentiating cellulitis with cutaneous and subcutaneous swelling from a true abscess. Predominantly hypoechoic fluid collection with mobile internal echoes on sonopalpation, echogenic capsule, and increased posterior through-transmission are characteristic findings of an abscess on ultrasound. However, ultrasound cannot assess the deeper extension of the abscess into the joint space or bone.
MRI is the preferred modality for soft-tissue abscess. On MRI, subcutaneous abscess demonstrate single or multiloculated well-circumscribed area of T1-weighted (T1W) isointense or hypointense signal, hyperintense (fluid-like) signal on fluid-sensitive sequences, with T1W post-contrast rim enhancement. However, subacute, chronic, or acute on chronic abscesses may demonstrate a peripheral rim of hyperintense signal relative to the low-signal abscess cavity on T1W pre-contrast images, referred to as the “penumbra sign,” with sensitivity and specificity of 54% and 98%, respectively, for differentiation of soft-tissue infection from neoplasm.[7] Like cerebral fungal abscess, on DWI, subcutaneous fungal abscess may show low apparent-diffusion-coefficient (ADC) of the walls and high ADC of the central contents. The center or periphery of the abscess may show susceptibility artifacts in susceptibility-weighted imaging, indicating toward its fungal composition. Characteristic magnetic resonance spectroscopy includes multiple signals between 3.6 and 3.8 ppm assigned to Trehalose, a fungal wall disaccharide.
Although MRI results lack specificity, imaging plays a crucial role in determining the extent of the infectious process, involvement of bone, and guiding surgical drainage of purulent collections.
HPE and culture plays the most important role in the diagnosis of phaeohyphomycosis.
The treatment of choice is surgical excision, but additional antifungal therapy is recommended for recurrent cases and immunocompromised patients. Itraconazole, voriconazole, posaconazole, and caspofungin have shown good results.[8] A number of other treatment modalities including amphotericin B, flucytosine, terbinafine, and griseofulvin, as well as physical treatment methods such as heat and cryosurgery have been utilized in patients with cutaneous phaeohyphomycosis.[9]
DIFFERENTIAL DIAGNOSIS
Common differential diagnosis of subcutaneous mycosis includes synovial cysts, mycetoma, chromoblastomycosis, and cutaneous nocardiosis [Table 1].
| Synovial cysts |
|
| Mycetoma (Maduramycosis) |
|
| Chromoblastomycosis |
|
| Cutaneous nocardiosis |
|
MRI: Magnetic resonance imaging, USG: Ultrasonography
CONCLUSION
The diagnosis of subcutaneous phaeohyphomycosis is difficult due to the clinical polymorphism of the lesion. Clinical presentation along with the findings from multimodal diagnostic tools including radiological, microbiological, and histological should direct toward diagnosis of phaeohyphomycosis. Since these fungal infections are subclinical in presentation, the importance of imaging and histology should be emphasized to achieve appropriate treatment, prevent recurrence, and avoid functional and mutilating sequelae.
TEACHING POINTS
Our case report highlights the fact that a subcutaneous abscess must also be considered under differential diagnosis for fungal infections even in immunocompetent individuals.
Although MRI findings of subcutaneous mycosis may be nonspecific and mimic many other conditions, it is not only helpful in delineating soft tissues and bone involvement but also differentiating it from deeper neoplastic growth.
MCQs
-
Which one of the following sentences is false regarding phaeohyphomycosis?
It is caused by dematiaceous fungi.
Melanin is the virulence factor.
Phaeohyphomycosis affects only skin and subcutaneous tissue.
Subcutaneous infections typically occur over the exposed areas of the body.
Answer Key: c
-
What is the standard modality for diagnosis of phaeohyphomycosis?
Ultrasound
Histopathology and culture
Gram stain
MRI
Answer Key: b
-
Which one of the following is false regarding subcutaneous phaeohyphomycosis?
Mycetoma is one of the close differential diagnoses.
HPE and culture plays an important role in the diagnosis.
Subcutaneous abscesses are treated with surgical excision.
Dot-in-circle sign is a characteristic MRI sign of phaeohyphomycosis
Answer Key: d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Subcutaneous phaeohyphomycosis caused by Cladophialophora boppii. Indian J Dermatol Venereol Leprol. 2010;76:695-8.
- [CrossRef] [PubMed] [Google Scholar]
- Phaeohyphomycosis of the face masquerading as basal cell carcinoma in an immunocompetent patient. Indian Dermatol Online J. 2017;8:271-3.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic disfiguring facial lesions in an immunocompetent patient due to Exophiala spinifera A case report and review of literature. Mycopathologia. 2012;174:293-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hyalohyphomycosis and phaeohyphomycosis: Two global disease entities of public health importance. Eur J Epidemiol. 1986;2:243-51.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous phaeohyphomycosis in an immunocompetent Individual: A case report. Indian Dermatol Online J. 2017;8:29-31.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous phaeohyphomycosis: A clinicopathological study. Int Surg J. 2014;1:140-3.
- [CrossRef] [Google Scholar]
- MRI nomenclature for musculoskeletal infection. Skeletal Radiol. 2021;50:2319-47.
- [CrossRef] [PubMed] [Google Scholar]
- Use of itraconazole for treating subcutaneous phaeohyphomycosis caused by Exophiala jeanselmei. Arch Clin Infect Dis. 1995;21:1068.
- [CrossRef] [PubMed] [Google Scholar]
- In vitro activity of amphotericin B, itraconazole, terbinafine and 5-fluocytosine against Exophiala spinifera and evaluation of post-antifungal effects. Med Mycol. 2003;41:301-7.
- [CrossRef] [PubMed] [Google Scholar]








