Translate this page into:
Cystic hemorrhagic intracranial metastasis in prostatic carcinoma
*Corresponding author: Vaibhav Gulati, Department of Diagnostic Radiology, Mercy Catholic Medical Center, Trinity Health Mid-Atlantic, Darby, Pennsylvania, United States. vaibhav-gulati@outlook.com
-
Received: ,
Accepted: ,
How to cite this article: Gulati V, Honarmand AR, Stachelek GC. Cystic hemorrhagic intracranial metastasis in prostatic carcinoma. Case Rep Clin Radiol. doi: 10.25259/CRCR_56_2024
Abstract
Several patterns have been identified related to intracranial metastasis presentation of prostate cancers; however, their pattern of presentation remains controversial, and a broad consensus remains to be established. Cystic, hemorrhagic lesions, although rare, are an important identity for radiologists to be aware of. We present the case of a 59-year-old male with prostatic carcinoma who developed extra-axial hemorrhagic intracranial metastasis along with a brief review of literature.
Keywords
Prostate carcinoma metastasis
Intracranial metastasis
Cystic
prostate
INTRODUCTION
Prostate cancer is the second leading cause of cancer-related deaths in males, after lung cancer. Advancements in treatment options and improving imaging techniques have led to early detection of intracranial metastatic lesions. Several patterns have been identified related to the presentation of intracranial metastasis in prostate cancers; however, controversy surrounds the pattern of presentation of intracranial metastasis, and a broad consensus remains to be established. We present an instance of cystic, extra-axial hemorrhagic intracranial metastasis in the setting of prostatic carcinoma, a presentation which has only been seen in a handful of cases.[1]
CASE REPORT
A 59-year-old male initially came to oncologic attention when he presented with progressive lower back pain. Computed tomography (CT) imaging of the abdomen and pelvis revealed extensive pelvic and retroperitoneal adenopathy with numerous osseous lesions. Prostate-specific antigen (PSA) level was 1420 ng/mL. Biopsy of an iliac lesion revealed metastatic prostate adenocarcinoma. Spinal magnetic resonance (MR) imaging demonstrated extensive osseous metastatic disease with cord impingement at the T3 level due to epidural extension of the metastatic disease. Androgen deprivation and enzalutamide therapy were initiated. Additional treatment included spinal palliative radiotherapy to the thoracic and lumbar spine due to spinal canal compromise secondary to metastatic disease. Follow-up evaluation demonstrated improvement in the clinical symptoms and PSA level. However, the patient presented 4 weeks later with complaints of back pain, numbness, and headaches. CT head imaging revealed two extra-axial parafalcine hemorrhagic lesions bilaterally concerning metastatic lesions. Subsequent MR brain imaging allowed for better visualization of intralesional hemorrhagic products, surrounding parenchymal edema, and mass effect related to the two lobulated parafalcine extra-axial lesions [Figures 1 and 2].
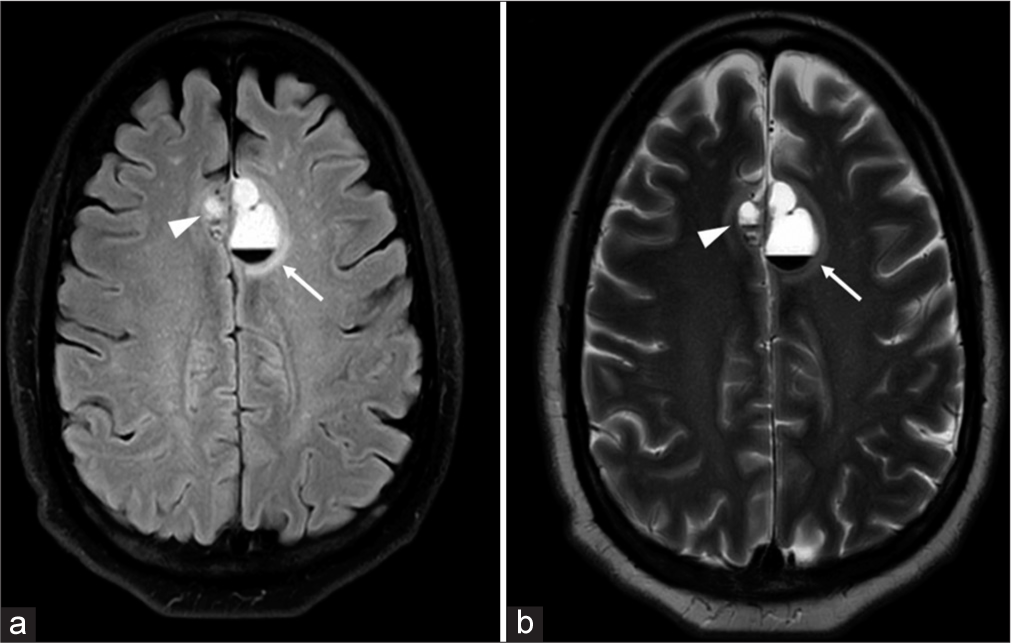
- (a) Axial FLAIR and (b) T2 weighted images showing lobulated cystic lesions (white arrowheads in both images) demonstrating predominantly T2 hyperintense/fluid appearance and a small amount of layering T2 hypointense hemorrhage. There is also mild surrounding T2/fluid attenuated inversion recovery (FLAIR) hyperintense edema. The larger lesion (white arrow in both images) measures 2.8 x 1.7 x 2.2, with mild mass effect upon the roof of the frontal horn of the left lateral ventricle and causes a 2 mm left to right midline shift. The smaller lesion in the right paramedian frontal lobe measures 1.2 x 0.8 x 1.2 cm.
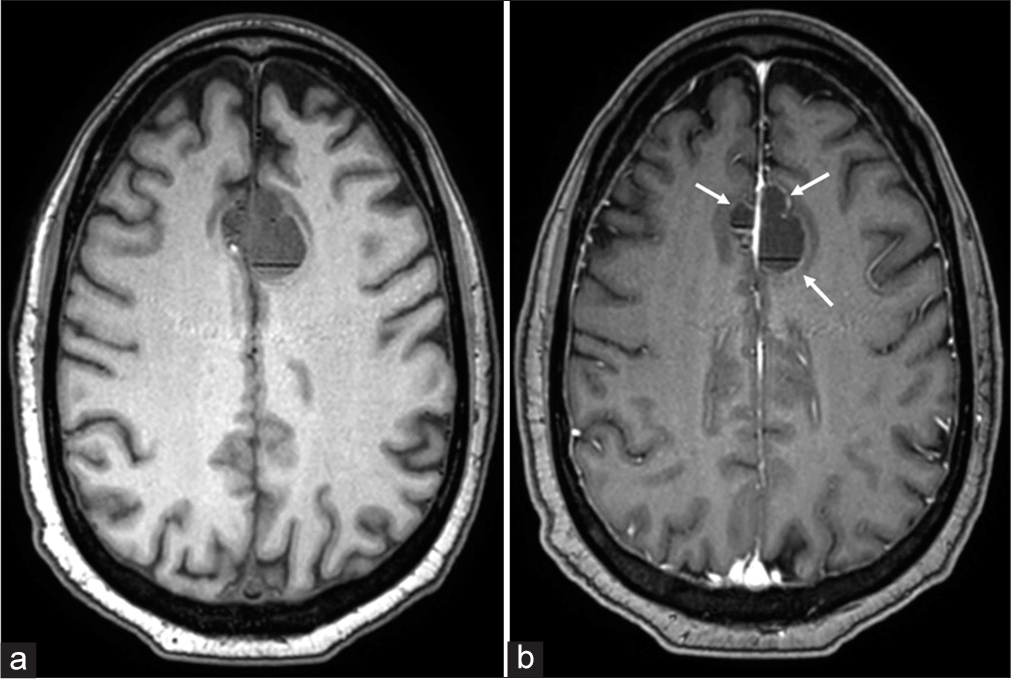
- (a) Pre-contrast and (b) post-contrast axial T1-weighted images demonstrating subtle rim enhancement (white arrows) of the cystic lesions.
The patient subsequently underwent a prostate-specific membrane antigen positron emission tomography imaging (not shown), which revealed tracer uptake throughout the known skeletal and nodal metastatic lesions, as well as described intracranial lesions.
A follow-up scan after 3 months of therapy showed a decrease in the size of the left parafalcine lesion and the right parafalcine lesions showed near-complete resolution [Figure 3a]. This provided additional confirmation that the lesions were metastases from prostatic adenocarcinoma. A later scan performed 3 months after completion of fractionated stereotactic radiotherapy (2700 cGy in 3 fractions) showed no evidence of the parafalcine lesions, and a complete response to therapy [Figure 3b].
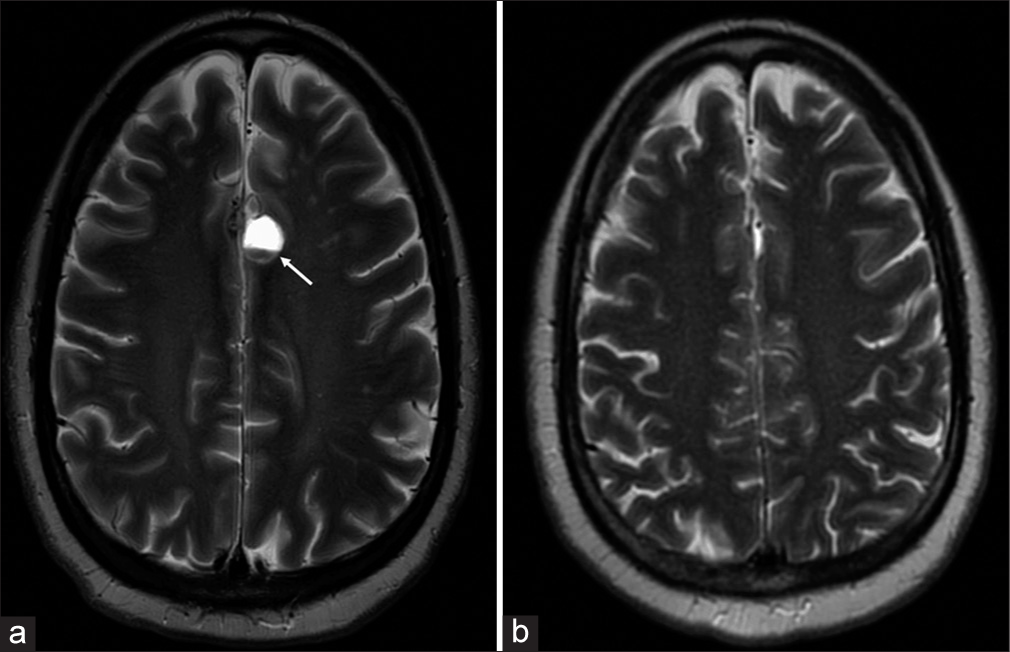
- (a) T2-weighted image acquired after 3 months of treatment showing the anterior parafalcine lesions containing hemorrhagic products measuring up to 2.1 x 1.1 cm predominantly along the left parafalcine region (white arrow). The previously seen smaller right parafalcine hemorrhagic lesion is almost completely resolved. (b) T2-weighted image acquired 3 months after Fractionated stereotactic radiation therapy (FSRT) to the cranial lesions showing complete interval resolution of previously seen layering cystic lesions.
DISCUSSION
Metastatic lesions to the brain from primary prostate cancer are rare with a reported incidence of 0.16 – 0.63%. Postmortem studies, however, report the incidence to be higher and around 1 – 6%.[2] Brain metastasis is usually seen with non-adenocarcinoma varieties such as small-cell, transitional cell, and neuroendocrine prostate cancer, which are uncommon subtypes and account for only 5 – 10% of all prostate carcinomas.[3,4] This low incidence, which may also be secondary to the fact that central nervous system imaging is not a standard part of staging for these patients, has been seen to be rising with the advent of newer therapies such as docetaxel and improving imaging techniques.[5,6]
Prostate metastases are mostly seen in patients with a Gleason score of 6 or more.[2,3] These lesions may be intraparenchymal, dural, or leptomeningeal, in decreasing order of incidence.[7] Metastatic lesions can reach the brain either through direct extension of skull metastatic lesions, leading to extradural lesions, or through the hematogenous route, giving rise to leptomeningeal and parenchymal lesions.[5] It is highly unlikely for a patient to have metastatic lesions in the brain without at least one additional site of extraprostatic tumor.[3] Their morphology can be variable, as can their presentation. Symptomatology depends on the location and extent of the lesions. Patients may present with symptoms of raised intracranial pressure such as papilledema, headache, as in our case, or may be asymptomatic.
Intracranial prostatic lesions can be evaluated using gadolinium-enhanced magnetic resonance imaging, which remains the gold standard for assessing the number, location, extension, and characterization of masses.[2] CSF PSA levels and/or tissue sampling may be most useful in cases which are difficult to characterize, in the setting of multiple primary cancers.[8] In their review of intracranial metastasis from prostate cancer, McBean et al., reported that the lesions had no characteristic imaging features, but they all showed enhancement, and most had perilesional edema. None of the cases reviewed in their study showed hemorrhagic or necrotic change.[9] In their study, Hatzoglou et al., found that seven out of the 21 cases demonstrated at least one hemorrhagic intraparenchymal lesion, a presentation that is more commonly reported in metastatic lesions secondary to lung cancer, renal cell carcinoma, melanoma, choriocarcinoma, and thyroid carcinoma. They also reported that enhancement patterns for the lesions vary from solid, mixed cystic-solid, or ring-like.[3] Solitary lesions are rare, and most cases have multiple lesions which may be supratentorial, infratentorial, craniospinal, or combination of these locations.[2] Our case also demonstrated two lesions, both showing rim enhancement and perilesional edema.
Intracranial metastatic lesions usually portend a poor prognosis for patient, with a reported survival period of up to 13 months with treatment options including corticosteroids, radiotherapy, surgery, and newer techniques such as stereotactic radiosurgery.[8] Prompt characterization plays a pivotal role in optimal and efficient treatment planning for a better prognosis.
CONCLUSION
Prostatic brain metastasis can have a highly variable presentation. With the advancements in therapeutic and imaging techniques, it is imperative to be aware of the myriad of imaging appearances or prostatic metastatic lesions. Cystic, hemorrhagic lesions, although rare, are an important identity for radiologists to be aware of.
TEACHING POINTS
Prostatic brain metastases are usually seen with nonadenocarcinoma varieties and can have a highly variable presentation. Solitary lesions are rare, and most cases have multiple lesions which may be supratentorial, infratentorial, craniospinal, or a combination of these locations
Prostate metastases are mostly seen in patients with a Gleason score of 6 or more. It is highly unlikely for a patient to have metastatic lesions in the brain without at least one additional site of extraprostatic tumor.
MCQs
-
Which of the following statements about metastatic prostatic carcinoma is true?
Most intracranial metastatic lesions are solitary
Intracranial metastases never show enhancement on gadolinium-enhanced MR imaging
Prostate metastases are usually seen in patients with a Gleason score of 6 or more
All of the above
Answer: c
-
The enhancement patterns for intracranial prostatic metastasis on gadolinium-enhanced MR imaging may be
Solid
Mixed solid-cystic
Ring-like
All of the above
Answer: d
-
Intracranial metastatic lesions from prostate carcinoma are most reported in what location?
Intra-parenchymal
Meningeal
Dural-based
Equally in all the above
Answer: a
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Metastatic prostatic adenocarcinoma to the brain and spinal cord: A contemporary clinicopathologic analysis of 30 cases. Int J Clin Exp Pathol. 2021;14:45-53.
- [Google Scholar]
- Brain metastases from prostate cancer: A single-center experience. Türk Ürol Der/Turk J Urol. 2019;45:279-83.
- [CrossRef] [PubMed] [Google Scholar]
- Brain metastases from prostate cancer: An 11-year analysis in the MRI era with emphasis on imaging characteristics, incidence, and prognosis. J Neuroimaging. 2014;24:161-6.
- [CrossRef] [PubMed] [Google Scholar]
- The clinical, diagnostic, therapeutic, and prognostic characteristics of brain metastases in prostate cancer: A systematic review. Prostate Cancer. 2022;2022:5324600.
- [CrossRef] [PubMed] [Google Scholar]
- Central nervous system metastases from castration-resistant prostate cancer in the docetaxel era. J Neurooncol. 2012;107:191-6.
- [CrossRef] [PubMed] [Google Scholar]
- Trial design and objectives for castration-resistant prostate cancer: Updated recommendations from the prostate cancer clinical trials working group 3. J Clin Oncol. 2016;34:1402-18.
- [CrossRef] [PubMed] [Google Scholar]
- Prostate cancer brain metastasis: Review of a rare complication with limited treatment options and poor prognosis. J Clin Med. 2022;11:4165.
- [CrossRef] [PubMed] [Google Scholar]
- Brain metastasis from prostate cancer: A review of the literature with an illustrative case. Int J Surg Open. 2021;37:100419.
- [CrossRef] [Google Scholar]
- Intracranial metastasis from prostate cancer: Investigation, incidence, and imaging findings in a large cohort of Australian men. J Clin Imaging Sci. 2021;11:24.
- [CrossRef] [PubMed] [Google Scholar]







