Translate this page into:
Brunn’s cyst presenting as a rare cause of lower urinary tract symptoms – A case report
*Corresponding author: Chandraditya Lamba, Department of Radiology, NIMS University, Jaipur, Rajasthan, India. chandradityalamba24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bansal RP, Tomar V, Yadav R, Verma SK, Lamba C. Brunn’s cyst presenting as a rare cause of lower urinary tract symptoms – A case report. Case Rep Clin Radiol. doi: 10.25259/CRCR_76_2024
Abstract
Brunn’s cyst in the region of the bladder neck is a rare cause of lower urinary tract obstruction. This case describes the ultrasonography and computed tomography urography findings of Brunn’s cyst as causing lower urinary tract symptoms and urinary retention.
Keywords
Brunn’s cyst
Lower urinary tract obstruction
Bladder neck
Computed tomography urography
Case report
INTRODUCTION
The most common causes of bladder outlet obstruction in adults are benign prostatic hyperplasia and urethral strictures. Brunn’s cyst is one of the rare causes of lower urinary tract symptoms. It results from inflammation and benign proliferation of cells in the Brunn’s nest, leading to cyst formation. This creates a ball valve[1] mechanism when located in the bladder neck and causes difficulty in voiding and an increase in post-void residual urine.
CASE REPORT
A 27-year-old male patient with complaints of urinary hesitancy and sensation of incomplete voiding followed by retention of urine presented in the urology outpatient clinic. The patient also had complaints of decreased urine flow, straining while voiding for 6 months, and was not on any medications.
On clinical examination, there was suprapubic fullness. The patient was catheterized and the retention volume was 800cc. He was advised to undergo a urine routine examination, ultrasound (USG) kidney, ureter, bladder (KUB), computed tomography (CT) urography, and cystoscopy.
Urine examination was normal, no significant findings were noted. USG of KUB showed a small, well-defined anechoic cystic lesion arising from the bladder neck, just above the prostate, anteriorly with no vascularity on color Doppler suggestive of Brunn’s cyst [Figure 1]. It measured about 1 cm in size. Mild diffuse wall thickening of the bladder was also noted. On CT urography, a well-defined cystic lesion measuring 1.2 cm × 0.8 cm was seen in the midline just anterior to the urethral opening, consistent with Brunn’s cyst. There was mild diffuse bladder wall thickening, suggestive of chronic cystitis changes [Figure 2]. Biopsy revealed von Brunn nests in lamina propria, consistent with diagnosis of Brunn’s cyst. Cystoscopy showed a 1.5 cm size smooth surfaced cyst in the bladder neck at 11–1 O’clock position, obstructing the bladder outlet. Mild trabeculations were seen in the bladder wall [Figure 3]. Complete resection of bladder cyst was done. Post-operative period was uneventful. The patient is currently asymptomatic.
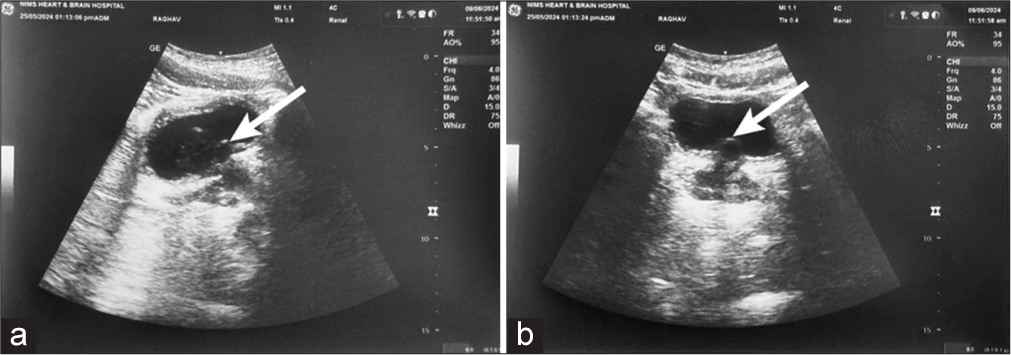
- (a-b) The above figure shows two ultrasound (USG) images. Both images show a small anechoic cystic lesion in the bladder base in midline, anterior to the bladder neck (white arrows) (a) transverse USG image, and (b) coronal USG image.
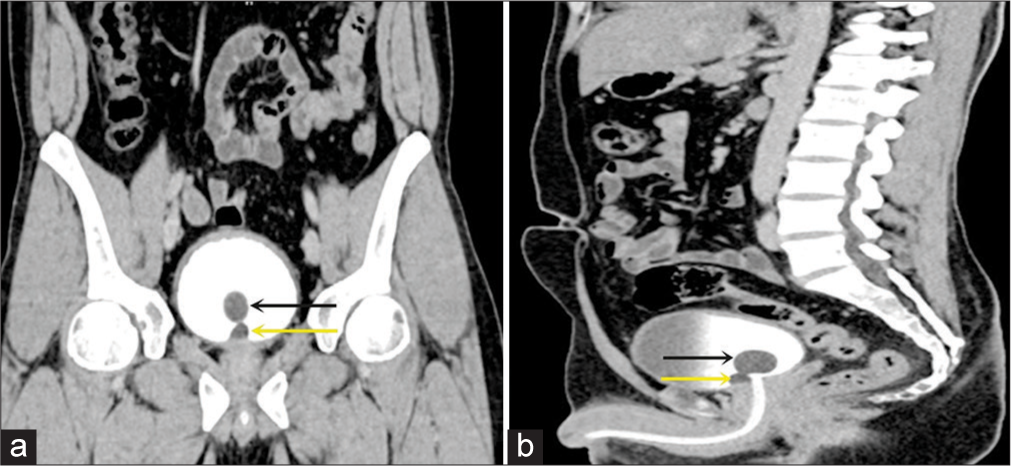
- (a) Coronal and (b) Sagittal CT urography images reveal a small Brunn’s cyst located in the midline anterior to the bladder neck, as indicated by the arrows (black arrows- Folley’s Bulb and yellow arrows- Brunn’s cyst). CT: Computed tomography.
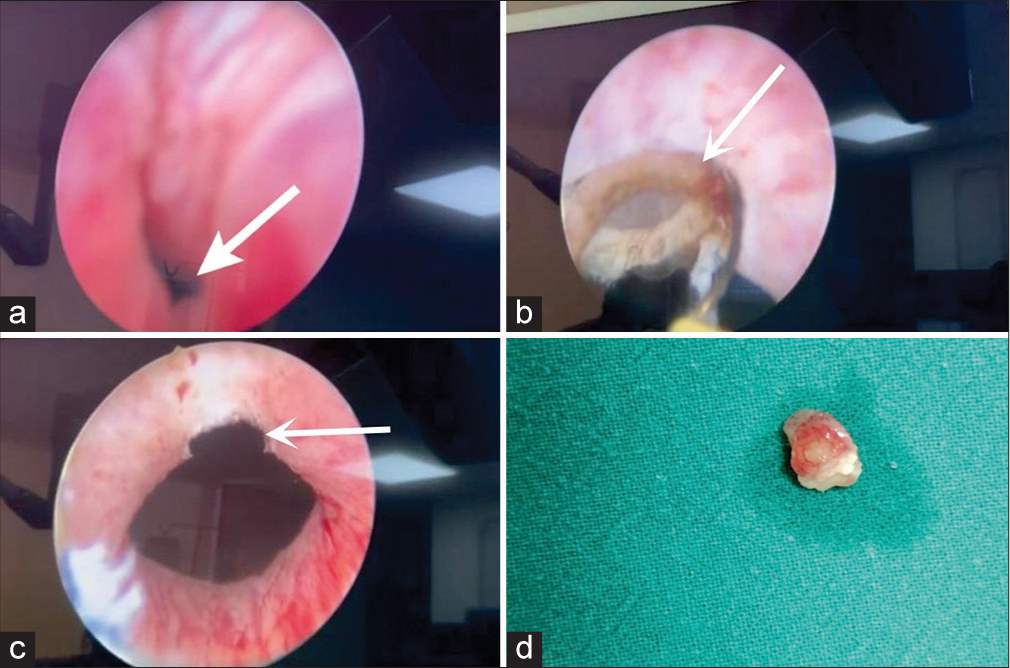
- (a and b) Cystoscopic images illustrate Brunn’s cyst, marked with arrows from various angles. (c) After cystoscopic resection, as indicated by the white arrow, the (d) resected specimen of Brunn’s cyst is shown. The postoperative image reveals the cyst that has been resected through cystoscopy and transurethral resection.
Histopathology of resected specimen showed a few von Brunn nests within lamina propria showing central cystic dilation with spaces lined by transitional. Lamina propria shows very mild inflammation, congestion, and hemorrhage – features consistent with Brunn’s cyst.
DISCUSSION
Brunn’s cyst or mucus cyst of the urinary bladder originates from von Brunn’s nest, which results from pinching off the epithelial nest[2] from urothelial buds. Common locations of Brunn’s cysts are ureters[3] and bladder floor. If present in the vicinity of the bladder neck, they may produce lower urinary tract symptoms and cause bladder neck, they may produce lower urinary tract symptoms and cause bladder neck obstruction by way of ball-valve mechanism.
Cystoscopy plays a diagnostic and therapeutic role. It reveals a cystic lesion at the neck and can be managed by transurethral deroofing or resection of the cyst.[4]
DIFFERENTIAL DIAGNOSIS
Differential diagnosis of Brunn’s cyst includes prostate cyst, cystitis cystica, ureterocele in ectopic ureter, intravesical ureterocele and other lesions [Table 1].
| Lesion | Location | Appearance | Salient features |
|---|---|---|---|
| Ureterocele | Ureteroceles are classified by location. (a) Intravesicle (Simple/ orthoptic):- Normal UVJ position - Situated at ureteric orifice. (b) Extravesical (ectopic) - Ectopic location, near bladder neck/posterior urethra. b. (1) Cecoureterocele Subtype of extravesicular ureterocele. |
IVP - Cobra head appearance at the ureteric orifice. USG - Cystic structure projecting into bladder near the VUJ. IVP - Cobra head sign - Radiolucent halo defect MCUG - Round oval lucency near trigone. - Inferior extension of ectopic ureterocele into urethra. |
- 25% cases. - CONGENiTAL prolapse of the dilated distal ureter into bladder lumen. - Always confined to adult population (pediatric cases show symptoms) - 75% cases - Almost always associated with duplication of collecting system due to abnormal embryogenesis. - 80% of the cases are unilateral. - Filling defect near bladder neck and posterior urethra. |
| Cystitis cystica and cystitis glandularis. | Cysts are in wall of UB and there is diffuse thickening of UB wall. When large may protrude in bladder lumen and may cause bladder outlet obstruction, if located near the bladder neck. | IVP - Lobulated outline of the UB with a nodular filling defect. CT Urogram - Hyper vascular polypoidal masses within the UB (best in delayed phase). MRI - T1-low-signal polypoidal lesion - T2-central hyperintensity and vascular stalk seen. |
Common benign condition with reactive inflammatory change of bladder mucosa. Cystitis cystica is caused due to degeneration of the urothelial cells in the lumen of von Brunn nests. Cystica glandularis is the proliferation of CC caused by glandular metaplasia of urothelium and goblet cells. |
| Prostatic cyst | Posterior part of prostate. | MRI-Midline prostatic cyst. | Often detected in 1st and 2nd decades of life. Associated with hypospadias and intersex anomalies. |
| Seminal vesical cyst | Placed in paramedian location in seminal vesicles | Best visualised on transrectal USG. Cysts are anechoic with internal debris. CT- Cysts appear well defined, low attenuation with hyperdense contents in cases of hemorrhage/ infection. MRI – both T1 and T2 sequences show high intensity due to proteinaceous contents. | Early distension of seminal vesicles noted. Associated with renal dysgenesis, ductus deferens agenesis and Zinner syndrome. |
| UB cysts | a) Urachal cyst – Lies along urachus, in the dome and anterior UB wall. May communicate with the bladder, if the urachal tract is open. b) Cloacal cyst – Posterior UB wall, seen in females only c) Simple cysts – In the wall of the UB |
Extremely rare. | |
| Dermoid cyst | Various anatomic locations are intracranial, orbital, spinal and ovarian. | Contains calcification and fat. Sack of marbles sign –- Orbital dermoid cyst - Spinal dermoid cyst - Hyperechoic on USG, fat attenuation on CT, and high signal in both T1 and T2 MRI. Floating balls sign- - Ovarian dermoid cyst- Inguinal dermoid cyst. USG - Echogenic balls giving no color flow on Doppler with anechoic/ hypoechoic fluid. CT - Balls vary from fat to soft-tissue density. MRI On T1 hyperintense rim noted. On T2 hypointense rim noted. |
Ectodermal inclusion cysts, lined by squamous epithelium. |
| Epidermoid | Intracranial, intradiploic, splenic, spinal, and testicular | Lesions contain soft tissue and calcification. T1-FS hyperintense and T2 hypointense showed diffusion restriction on MRI. | Non-neoplastic inclusion cysts derived from ectoderm lined solely by squamous epithelium. |
| Hydatid cyst | Hepatic, pulmonary, splenic, cerebral, spinal retroperitoneal, mediastinal (rare), musculoskeletal. | Multicystic/ spoke wheel pattern on T2-weighted or post-contrast images and angiography. | Worldwide geographic distribution. Caused by Echinococcus tapeworm. |
CT: Computed tomography, MRI: Magnetic resonance imaging, USG: Ultrasound, UB: Urinary bladder, UVJ: Ureterovesical junction, CC: Cystitis cystica, IVP: Intravenous pyelogram, VUJ: Vesico-ureteric junction, MCUG: Micturating cystourethrogram
CONCLUSION
Presence of Brunn’s cyst at bladder neck though rare but should be kept in mind, especially in young and otherwise healthy patient, who presents with persistent LUTS. Transurethral deroofing or excision of cyst results in resolution of the obstructive symptoms and resumption of normal voiding.
TEACHING POINTS
Brunn’s cyst is one of the rarest causes of bladder outlet obstruction.
Cystoscopy plays both diagnostic and therapeutic roles.
MCQs
-
What is a Brunn’s cyst?
A type of renal cyst commonly found in adults
A benign cyst found in the prostate gland
A fluid-filled cyst within the thyroid gland
A benign cystic lesion originating from the urothelium in the urinary bladder
Answer Key: d
-
Which of the following is a common characteristic of Brunn’s cysts?
They are always symptomatic and require immediate treatment.
They often contain malignant cells.
They are typically asymptomatic and discovered incidentally but may cause symptoms when present in vicinity of the bladder neck.
They frequently cause hematuria and dysuria.
Answer Key: c
-
How are Brunn’s cysts usually diagnosed?
Through blood tests
Through ultrasound and other imaging modalities
By cystoscopy
By identifying symptoms like severe abdominal pain and fever
Answer Key: b and c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Bladder neck obstruction secondary to brunn's cyst. J Urol. 1988;139:126-7.
- [CrossRef] [PubMed] [Google Scholar]
- New concepts on formation of Brunn's nests and cysts in urinary tract mucosa. Urology. 1978;11:513-7.
- [CrossRef] [PubMed] [Google Scholar]
- Brunn's cyst: A rare cause of lower urinary tract symptoms. Indian J Urol. 2018;34:231-2.
- [CrossRef] [PubMed] [Google Scholar]
- Brunn's cyst inducing persistent lower urinary tract symptoms in a young man: A case report. J Endourol Case Rep. 2019;5:171-3.
- [CrossRef] [PubMed] [Google Scholar]







