Translate this page into:
Bone within the endometrium: An uncommon cause of secondary infertility
*Corresponding author: Rama Anand, Department of Radiodiagnosis, Lady Hardinge Medical College, New Delhi, Delhi, India. rama_home@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Meena N, Chopra K, Anand R, Gaur K, Osama MA. Bone within the endometrium: An uncommon cause of secondary infertility. Case Rep Clin Radiol. doi: 10.25259/CRCR_185_2023
Abstract
Endometrial osseous metaplasia is an uncommon non-neoplastic gynecological condition, resulting in formation of mature or immature bone within the endometrial stroma. Most cases present with secondary infertility following an abortion. Although hysteroscopy is considered gold standard for the diagnosis of this rare entity, ultrasound (USG) plays an important role in its initial diagnosis. It is a challenging diagnosis due to its infrequency and similarity to other uterine pathologies. The characteristic USG appearance showing multiple bone fragments within the endometrium suggests the diagnosis. The current case report aims to highlight the role of USG in the detection and evaluation of the endometrial osseous metaplasia in patients presenting with secondary infertility.
Keywords
Osseous metaplasia
Abortion
Secondary infertility
Ultrasound
Hysteroscopy
INTRODUCTION
Endometrial osseous metaplasia is an uncommon non-neoplastic gynecological condition, causing mature or immature bone formation within the endometrial stroma.[1]
Approximately 80% patients present with a history of the previous spontaneous abortion or termination of pregnancy followed by secondary infertility.[2] However, some of the patients present with non-specific complaints including abnormal uterine bleeding, vaginal discharge, pelvic pain, and dyspareunia while others are asymptomatic.[3]
The diagnosis of endometrial osseous metaplasia should be considered in all patients presenting with secondary infertility preceded by previous history of abortion, where ultrasound (USG) reveals markedly echogenic bone fragments within the endometrium.[2]
In this case report, we present one such case in a 30-year-old female patient, who presented with secondary infertility, and was diagnosed on transvaginal ultrasound (TVS) as endometrial osseous metaplasia, proven on histopathology.
CASE REPORT
A 30-year-old female, married for 10 years, Para 1 Live 1 Abortion 1 was referred from a private facility to the tertiary care hospital in view of investigation of secondary infertility. She had a spontaneous abortion 3 years back, subsequent to which she underwent dilatation and curettage at 3rd month of gestation in view of missed abortion. She did not conceive after this event and had now presented with secondary amenorrhea for almost 2.5 years, with history of menstrual bleeding only on progesterone withdrawal.
Her physical and pelvic examination was normal. The hematological parameters and hormonal profile including luteinizing hormone and follicle-stimulating hormone levels, thyroid-stimulating hormone levels, and serum prolactin levels of the patient were within normal limits. Her husband’s spermiogram was also normal.
TVS was performed on GE Voluson USG machine using a 4–12 MHz Transvaginal probe. Longitudinal and transverse scans [Figure 1a and b] revealed multiple thick variable-sized, irregular linear, markedly echogenic structures with posterior acoustic shadow suggestive of osseous fragments filling the entire endometrial cavity. The anterior uterine myometrium showed normal echo pattern; however, the posterior myometrium could not be assessed in entirety due to strong posterior acoustic shadow due to the bony fragments within the endometrium. The cervical canal was unremarkable. Bilateral ovaries and adnexa were unremarkable. A presumptive diagnosis of osseous metaplasia of endometrium was made based on USG findings. Patient’s biochemical investigations were reviewed to rule out any metabolic cause and her serum calcium levels were within normal limits.

- Transvaginal ultrasound scan of uterus. (a) Sagittal image shows multiple hyperechogenic structures in the endometrium (yellow arrow) suggestive of bone fragments with posterior acoustic shadow. (b) Axial image shows aggregation of bone fragments (yellow arrow) in the endometrium with posterior acoustic shadow.
Subsequently, an operative hysteroscopy was performed which confirmed the USG findings. Multiple bony spicules were removed piece by piece from the endometrial cavity [Figure 2]. Some of the bony fragments were deeply embedded in the endometrium, hence could not be removed considering the high possibility of damage to the endometrium or even uterine perforation. Endometrial biopsy was obtained during the procedure and was sent for histopathological examination and Ziehl-Neelsen (ZN) staining for mycobacteria.
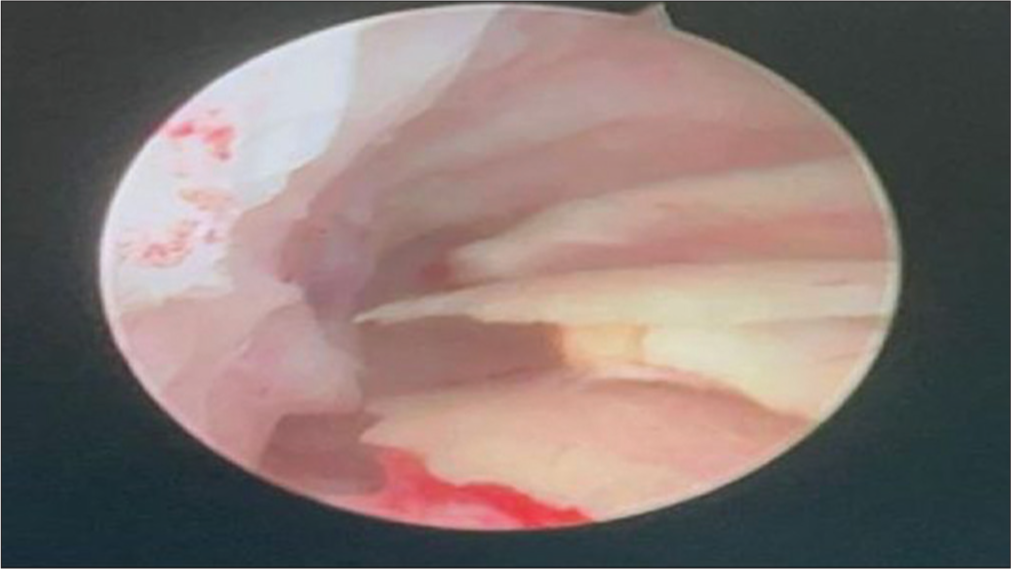
- Diagnostic hysteroscopic examination reveals multiple bony spicules in the endometrial cavity directed to the posterior uterine wall.
Diagnosis of endometrial osseous metaplasia was confirmed based on the histopathological examination. The H- and E-stained high-power view microphotographs [Figure 3] revealed irregular woven bone undergoing ossification surrounded by occasional endometrial glands and stromal tissue. ZN staining for mycobacteria was negative for any acid-fast bacilli.

- High-power view shows irregular woven bone undergoing ossification (green arrow) with surrounding occasional endometrial stromal tissue (black arrow). Histopathological examination ×400.
A repeat TVS 2 weeks post-hysteroscopic intervention revealed few bony fragments in the lower part of endometrial cavity and the rest of endometrial cavity was free. The patient was given estrogen-progesterone regimen for 2 months for endometrial regeneration. Following the regimen, the patient resumed her normal menstrual cycles and was asked to undergo ovulation induction with intra-uterine insemination for three cycles. It was decided by the treating gynecology team, that a second look hysteroscopy and removal of remaining fragments can be planned after proper counseling of the patient in case she fails to conceive.
DISCUSSION
Endometrial osseous metaplasia is a rare gynecological condition with an incidence of 3 in 10,000 women. This Magudapathi et al.[4] in their case report quoted that in year 2000, Sorinala et al.[5] suggested the differentiation of multipotential stromal cells to osteoblasts due to chronic inflammation as the cause for development of bone in the endometrium. Despite such a high prevalence of abortions worldwide, there is sparse literature on osseous metaplasia, likely due to misdiagnosis of the patients.[6] With increasing use of USG for the evaluation of infertility, this condition is being diagnosed more frequently.
It is a benign pathological condition affecting the uterine endometrium, characteristically affecting women in the reproductive age group. Most of the patients present with secondary infertility following a history of the previous abortion which was seen in our case as well. The etiopathogenesis of this condition is still debatable and the multiple theories postulated include the reparative response of the endometrium to chronic inflammation, de novo differentiation of mesenchymal cells into bone, direct implantation of the retained fetal parts into the endometrium.[4,5,7] Two hypotheses which have gained wide acceptance include the spontaneous differentiation of multi-potent endometrial fibroblast cells into osteoblasts in conditions of long-term estrogenic stimulation or chronic endometrial inflammatory conditions. Another hypothesis supports the implantation of the fetal bony parts into the endometrium which induces osseous metaplasia.[6-8] Retained fetal parts post-abortion, which, however, does not explain the presence of bone within endometrium in the first trimester as fetal bone ossification, or osteogenesis starts between 6th and 7th week of embryonic life and the hemopoietic marrow does not develop until the third trimester.[2] In addition, another study found similarity between the DNA of the mother and the DNA of endometrial bony fragments.[8] Endometrial ossification can also be seen in metabolic and endometrial disorders, in events of excessive calcium and Vitamin D consumption and after prolonged estrogenic stimulation of endometrium.[1] In India, due to its high prevalence, tuberculosis also needs to be ruled out as it can cause endometrial calcification due to chronic inflammation.[6,7] The time interval between the past abortion and the osseous metaplasia can range from 8 weeks to 15 years.[7] In our reported case, the time interval was 3 years. Over 80% patients present with secondary infertility. The proposed mechanism explains that the presence of the foreign body (osteoblasts) within the endometrium acts as an intrauterine contraceptive device (IUCD) preventing implantation of the blastocyst, resulting in infertility in such patients.[2]
Hysteroscopy is considered the gold standard for the diagnosis as well as treatment for endometrial osseous metaplasia. However, pelvic USG is gaining wider acceptance for its initial diagnosis due to its ease of availability and non-invasive nature. The characteristic presence of multiple markedly echogenic linear structures with posterior acoustic shadow in the endometrial cavity strongly favor the diagnosis of osseous tissue within the endometrium. Involvement of the cervix along with endometrium is also seen in some cases.[2,4] It is important for a radiologist to be aware of important differentials for this condition which include IUCD, chronic endometritis, pelvic tuberculosis, Asherman’s syndrome, and mixed Mullerian tumor.[2,4,6]
CONCLUSION
Endometrial osseous metaplasia is a rare yet treatable cause of secondary infertility which is frequently overlooked. Radiologists should be aware of this infrequent condition and familiarize themselves with its distinctive appearance on USG. This proactive approach can potentially reduce instances of misdiagnosis, thereby facilitating more precise patient management.
TEACHING POINTS
Endometrial osseous metaplasia is a rare but treatable cause of secondary infertility.
USG plays a crucial role in the initial detection of endometrial osseous metaplasia.
Hysteroscopic removal of the bony fragments in endometrium can result in restoration of fertility in the patient.
MCQs
-
True about endometrial osseous metaplasia are all except-
Corresponds to bony fragments within the endometrial cavity
Treatable cause of infertility
Neoplastic condition
Can involve the uterus and cervix
Answer Key: c
-
Differential diagnosis for endometrial osseous metaplasia include all except-
IUCD
Genital tuberculosis
Calcified submucosal fibroids
Adenomyosis
Answer Key: d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Endometrial osseous metaplasia: An unusual cause of infertility. BMJ Case Rep. 2015;2015:bcr2015209523.
- [CrossRef] [PubMed] [Google Scholar]
- Endometrial osseous metaplasia in a patient with secondary infertility referred for hysterosalpingogram with ultrasound. J Med Imaging Radiat Oncol. 2021;65:909-10.
- [CrossRef] [PubMed] [Google Scholar]
- Osseous metaplasia of the endometrium: A rare entity. J Obstet Gynecol India. 2015;65:342-5.
- [CrossRef] [PubMed] [Google Scholar]
- Subfertility due to osseous metaplasia of the endometrium treated by hysteroscopic resection. Curr Obstet Gynaecol. 2000;1:42-3.
- [CrossRef] [Google Scholar]
- Imaging of endometrial osseous metaplasia-an uncommon but treatable cause of infertility. Middle East Fertil Soc J. 2020;25:35.
- [CrossRef] [Google Scholar]
- Endometrial osseous metaplasia: Case report with literature review. Ann Med Health Sci Res. 2013;3:10-2.
- [CrossRef] [PubMed] [Google Scholar]
- True osseous metaplasia of the endometrium: The bone is not from a fetus. Fertil Steril. 2009;91:1293.e1-4.
- [CrossRef] [PubMed] [Google Scholar]








