Translate this page into:
Blind ectopic hemato-megaureter: A rare association with the rare obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome
*Corresponding author: Jyoti Arora, Department of Radiology, Medanta, The Medicity, Gurugram, Haryana, India. dr.jyotiarora@yahoo.co.uk
-
Received: ,
Accepted: ,
How to cite this article: Garg A, Arora J, Mittal P. Blind ectopic hematomegaureter: A rare association with the rare obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome. Case Rep Clin Radiol. doi: 10.25259/CRCR_89_2024
Abstract
Obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome is a rare complex of structural abnormalities of the female urogenital tract characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal anomaly. In this article, we report a case of an 11-year-old girl who presented with pain in lower abdomen since the onset of menarche 8 months back. Magnetic resonance imaging revealed uterus didelphys, hematometrocolpos, hematosalpinx, obstructed hemivagina, and left renal agenesis. There was an associated dilated, tortuous tubular structure with hemorrhagic contents in the midline in the pouch of douglas, with a proximal blind end in the left paravertebral region and distal ectopic insertion in the cervix (hematocolpos) suggestive of blind ectopic hemato-megaureter. To the best of our knowledge, there are very few reported cases of associated blind hemato-megaureter with ectopic insertion into the cervix in a case of OHVIRA syndrome. Imaging findings were confirmed on diagnostic laparoscopy with vaginoscopy and cystoscopy.
Keywords
Obstructed hemivagina and ipsilateral renal agenesis syndrome
Müllerian duct anomaly
Renal anomaly
Blind ectopic megaureter
Magnetic resonance imaging
INTRODUCTION
Obstructed hemivagina and ipsilateral renal agensis (OHVIRA) syndrome is a rare complex congenital anomaly of Mullerian (paramesonephric) and Wolffian (mesonephric) ducts.[1-3] It was first reported in 1922 and subsequently described in detail by Herlyn, Werner and Wunderlich (HWW), after whom it was named as HWW syndrome. The incidence of OHVIRA syndrome varies from 0.1% to 3.8%.[4] It typically occurs as a triad of uterus didelphys, obstructed hemivagina, and ipsilateral renal anomaly.[5] Although renal agenesis is the most characteristic urological anomaly seen in OHVIRA syndrome, it may be rarely associated with multicystic dysplastic kidneys, duplication of kidneys and ureter, ectopic ureter or vesicovaginal fistula.[6-8] Diagnosing ureteral anomalies can pose challenges due to their infrequent occurrence and imaging characteristics that can resemble an adnexal lesion in female patients. Early magnetic resonance imaging (MRI) helps in the successful diagnosis and timely management of the patient.
CASE REPORT
An 11-year-old girl presented with pain in lower abdomen since the onset of menarche 8 months back, with the recent increase in severity associated with fever. She reported a history of very painful irregular periods lasting 4–5 days with average flow. Local examination revealed normal hymen, external genitalia, and secondary sexual characters.
Trans-abdominal ultrasound of the pelvis revealed a small uterus-like structure. An elongated tubular cystic lesion was posterior to the bladder, from the midline extending into the left adnexal region. Another cystic septated lesion with diffuse internal echoes was also seen medial to the tubular lesion. There was the absence of a left kidney, which raised the suspicion of a complex Mullerian anomaly, warranting contrast enhanced MRI for the patient.
Contrast-enhanced MRI of the pelvis and upper abdomen revealed two uterine cavities and cervices, suggesting didelphys uterus [Figure 1]. The right horn of the uterus [Video 1, AR2], right cervix [Video 1, AR9], and right ovary [Video 1, AR1] appear normal. The left horn of the uterus and left cervix were significantly dilated with hemorrhagic contents within, suggestive of hematometra [Video 1, AR3] and hematocolpos [Video 1, AR4], [Figure 1]. A dilated tortuous tubular structure was seen adjacent to the left ovary with hemorrhagic contents within, suggestive of hematosalpinx [Video 1, AR5]. A cystic lesion showing T2 shadowing was seen in the left ovary, suggestive of a chocolate cyst [Video 1, AR6], with normal peripherally arranged follicles noted [Video 1, AR7], [Figure 1].
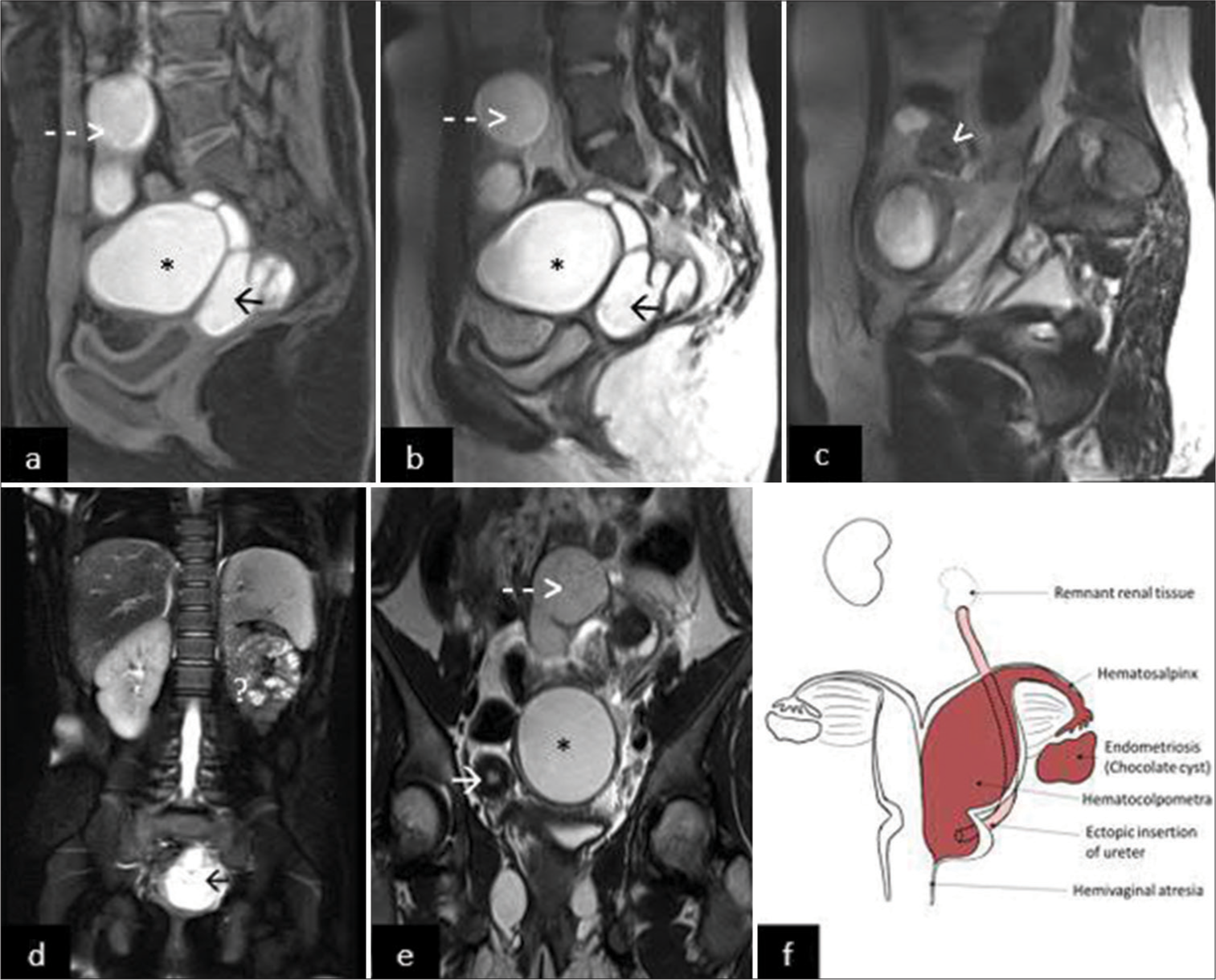
- An 11-year-old girl presented with pain in lower abdomen since the onset of menarche 8 months back. (a) T1-weighted sagittal images showing hematocolpometra (*), hematosalpinx (dashed arrow), and hematomegaureter in pouch of Douglas (black arrow); (b) T2-weighted (T2w) sagittal images showing hematocolpometra (*), hematosalpinx (dashed arrow), and hematomegaureter in pouch of Douglas (black arrow); (c) T2w sagittal images showing chocolate cyst (white arrowhead) with peripherally arranged follicles; (d) T2 fat-saturated images showing empty left renal fossa (?) with dilated hematomegaureter in the pelvis (black arrow); (e) T2w coronal images showing uterus didelphys with normal right horn (white arrow) with hematocolpometra (*) and hematosalpinx (dashed arrow); (f) A simplified diagram showing didelphys uterus with left hematocolpometra, hematosalpinx, and endometriotic chocolate cyst in the left adnexa. Left blind hematomegaureter with distal insertion into the cervix. Obstructed hemi vagina with transverse septum. The left kidney is not identified in the renal fossa, with atrophic remnant renal tissue at the blind end of the ureter in the left hemipelvis. The right horn of the uterus, right cervix, and right ovary is normal. Normal morphology solitary right kidney was noted.
Normal morphology solitary right kidney was seen. The left kidney could not be identified in the renal fossa [Figure 1]. There was a dilated, tortuous tubular structure in the midline in the pouch of douglas [Video 1, AR10], [Figure 1d] with a proximal blind end in the left para vertebral region [Video 1, AR8], up to the level of L4–L5 vertebrae and distal ectopic insertion into the cervix [Video 1, AR11], showing hemorrhagic contents within due to backflow from the hematocolpos, suggestive of blind ectopic hematomegaureter. Atrophic renal tissue was noted at its blind end in the left hemi pelvis. Vagina was compressed due to the aforementioned dilated structures, and it was difficult to comment on the presence of a septum; however, obstructed hemi vagina due to a transverse septum was suspected.
Findings were suggestive of obstructed hemivagina (causing hematocolpos, hematometra and hematosalpinx) and ipsilateral renal agenesis (OHVIRA syndrome) with a blind ectopic hemato-megaureter.
Imaging findings were confirmed on diagnostic laproscopy with cystoscopy and vaginoscopy. Two uterine horns were seen [Figure 2a]. The right uterine horn, fallopian tube, and ovary were normal. The left uterus and tube were distended, consistent with hematometrocolpos and hematosalpinx. Multiple endometriotic deposits were seen in the pouch of douglas and the lateral pelvic wall, with an endometriotic cyst seen in the left ovary. A blind ending thin tubular structure was seen entering from the left uterosacral ligament to the left cervix [Figure 2b]. The left trigone was not developed with non-visualization of the left ureteric orifice. Decompression of left hematometrocolpos, hematosalpinx, and hemato megaureter with left ovarian cyst drainage was done. The creation of a drainage tract from the vaginal end was not possible due to complete non-communication and atresia.
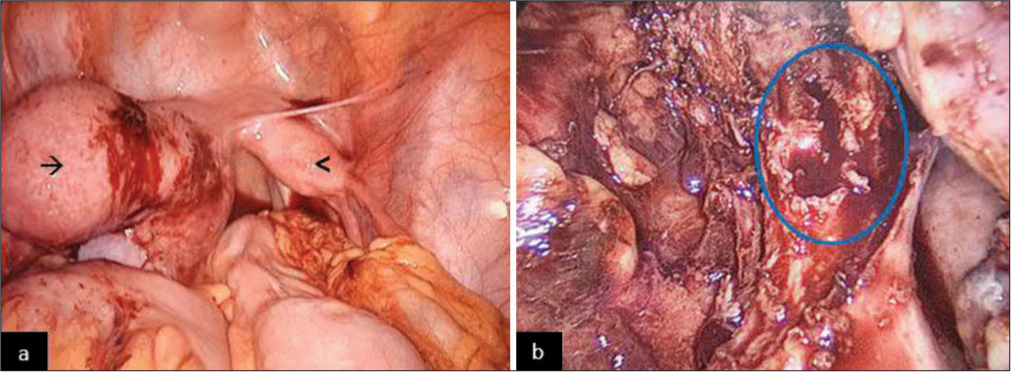
- An 11-year-old girl presented with pain in lower abdomen since the onset of menarche 8 months back. Diagnostic laproscopy revealed (a) two uterine horns with normal right uterine horn (arrow head). The left uterus was distended consistent with hematometrocolpos (arrow). (b) After the removal of cervix and uterine horn, a cut megaureter (blue outlined) was seen with chocolate fluid oozing from within.
Definitive treatment by hemihysterectomy (removal of hemiuterus, cervix, and fallopian tube) was done after an interval of 12 weeks, after suppressing the periods to reduce inflammation and post-operative bleeding. The ectopic megaureter was left in situ after ligation of the distal end communicating with the left cervix to limit the surgical morbidity for the patient.
DISCUSSION
OHVIRA syndrome is a rare congenital anomaly with a characteristic triad of uterus didelphys, obstructed hemivagina, and ipsilateral renal anomaly.[1-4] While renal agenesis is the most common urological anomaly in OHVIRA syndrome, other rare associations include multicystic dysplastic kidneys, duplicated kidneys and ureter, ectopic ureter, or vesicovaginal fistula.[6-8] Blind hemato-megaureter with ectopic insertion into the cervix is one of the rarest association with OHVIRA syndrome, as seen in our case, with only a couple of cases reported in the literature.[9] Renal anomalies typically occur on the same side as the obstructed hemivagina, with the right side being affected approximately twice as frequently as the left side.[10-12]
The spectrum of abnormalities prompts us to consider the etiopathogenesis of the syndrome. It is considered to be a developmental anomaly of Mullerian and Wolfian ducts.
Two pairs of Müllerian ducts merge from craniocaudally to form the uterus, cervix, and upper two-thirds of the vagina.[10-13] In addition, these fused Müllerian ducts extend into the urogenital sinus, from which the lower third of the vagina originates. The Wolffian ducts not only develop into the ureter and kidneys but also play a role in ensuring proper fusion of the Müllerian ducts. Abnormal development of the Wolffian duct can lead to improper differentiation of the ureter and kidneys, as well as lateral displacement of the Müllerian duct on the same side. This displaced Müllerian duct fails to merge with the opposite duct, resulting in uterine didelphys.[7,10-12]
In our case, a blind ectopic megaureter was seen communicating with the cervix with non-development of left hemitrigone in the bladder. The absence of the hemitrigone, along with the presence of an ectopic ureter in the cervix, indicates that the wolfian ducts beyond the point where the ureteric bud originates are absorbed into the Mullerian ducts rather than developing into the expected bladder structure.[13-16] This anomalous absorption prevents the solid tip of the fused Mullerian duct on the affected side from reaching the urogenital sinus and sinovaginal bulbs. As a result, the hemivagina on that side becomes obstructed, while the contralateral hemivagina develops normally. The unusual ascent and positioning of the kidney can be attributed to the abnormal ureteric bud and the abnormal fusion of the wolfian duct, which obstructs its normal ascent.
The subject of embryonic development of the vagina has sparked intense debate following Acien’s proposal of a new theory regarding its origin.[17] Acien proposed that the vagina originates entirely from Wolffian (mesonephric) tissue – a concept validated in experiments on female rats by Sánchez-Ferrer et al.[18] Anomalies in wolfian (mesonephric) duct development prevent the induction of the metanephric blastema, which leads to the failure of kidney formation. In addition, since the vagina derives from Wolffian tissue, its development is also affected. Furthermore, the absence of growth factors from the mesonephros disrupts the proper positioning and fusion of the paired Mullerian ducts, resulting in their non-fusion (uterus didelphys). Consequently, this constellation of factors gives rise to OHVIRA syndrome.
OHVIRA syndrome typically manifests shortly after menarche, and patients commonly experience pelvic pain or dysmenorrhea, sometimes accompanied by a palpable mass due to hematocolpos or hematometra.[10] In cases of incomplete obstruction, symptoms may be delayed because one hemivagina remains patent, allowing menstrual blood to exit.[8,9] However, in cases of complete obstruction, there is early presentation as there is no exit of the menstrual blood, as seen in our patient. As time progresses, the risk of complications such as endometriosis, menstrual irregularities, infertility, and other obstetric issues increases, necessitating an early and accurate diagnosis.[10-12] Lecka Ambroziak et al. summarized the large series of patients with OHVIRA syndrome along with the associated complications and anomalies as tabulated in Table 1.[19]
| Associations and complications of OHVIRA syndrome |
|---|
| Urologic |
| Agenesis |
| Multicystic dysplastic kidney |
| Duplicated kidney and ureter |
| Urinary tract infections |
| Vesicovaginal fistula |
| Ectopic insertion of ureter |
| Genital |
| Infertility |
| Menstrual irregularities |
| Endometriosis |
| Adenosis of vaginal septum |
| Cervical agenesis |
OHVIRA: Obstructed hemivagina and ipsilateral renal agensis
Ultrasound and MRI are the most commonly used modalities for imaging Mullerian duct anomalies. Ultrasound is a noninvasive, radiation free and widely available modality, hence the most commonly used initial investigation. The absence of a kidney in the renal fossa with hematometrocolpos should raise suspicion of complex Mullarian anomalies, warrantying contrast-enhanced MRI for demonstration of detailed anatomy. MRI is the imaging modality of choice for the evaluation of pelvic pathologies. It provides a detailed evaluation of the urogenital anatomy as well as helps in further characterisation of the lesions. It helps in the detection of associated findings such as endometriosis, pelvic infections, and other associated urologic anomalies.
Resection of the obstructed vaginal septum or the creation of drainage tract from the vaginal end is the treatment of choice.[16] Hemihysterectomy is used only in cases with complete non-communication or vaginal atresia, as in our case.
CONCLUSION
Diagnosing these intricate anomalies has seen a rise over the years, thanks to heightened awareness and the accessibility of advanced MRI techniques that effectively detect these lesions. MRI stands out as the most effective diagnostic tool for identifying Müllerian duct anomalies and associated conditions compared to other imaging modalities. In pubertal females, symptoms such as cyclical abdominal pain accompanied by a lower abdominal lump and renal anomaly should raise suspicion of OHVIRA syndrome. A high index of suspicion is essential for promptly diagnosing and managing these complex conditions.
TEACHING POINTS
OHVIRA syndrome is a rare congenital anomaly with a characteristic triad of uterus didelphys, obstructed hemivagina, and ipsilateral renal anomaly.
Blind hemato-megaureter with ectopic insertion into the cervix is one of the rare associations with OHVIRA syndrome.
In pubertal females, symptoms such as cyclical abdominal pain accompanied by a lower abdominal lump and renal anomaly should raise suspicion of OHVIRA syndrome.
MCQs
-
OHVIRA syndrome is a rare complex congenital anomaly involving?
Mullerian (paramesonephric) ducts
Wolfian (mesonephric) ducts
Both of the above
None of the above
Answer Key: c
-
Which of the following is not associated with OHVIRA syndrome?
Duplicated kidneys and ureter
Cardiac anomalies
Blind ectopic ureter
Vesicovaginal fistula
Answer Key: b
-
Which is the most common age of presentation of OHVIRA syndrome?
Menarche
Pregnancy
Adulthood
Menopause
Answer Key: a
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The Herlyn-Werner-Wunderlich triad (OHVIRA syndrome) with good pregnancy outcome-two cases and literature review. Rom J Morphol Embryol. 2018;59:1253-62.
- [Google Scholar]
- Screening for Mullerian anomalies in patients with unilateral renal agenesis: Leveraging early detection to prevent complications. J Pediatr Urol. 2018;14:144-9.
- [CrossRef] [Google Scholar]
- Diagnosis, management, and outcome of obstructed hemivagina and ipsilateral renal agenesis (OHVIRA syndrome): Is there a correlation between MRI findings and outcome? Clin Imaging. 2020;59:172-8.
- [CrossRef] [Google Scholar]
- Multiple variants of obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome-One clinical center case series and the systematic review of 734 cases. J Pediatr Urol. 2021;17:653.e1-9.
- [CrossRef] [Google Scholar]
- Obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome should be redefined as ipsilateral renal anomalies: Cases of symptomatic atrophic and dysplastic kidney with ectopic ureter to obstructed hemivagina. J Pediatr Urol. 2015;11:77.e1-6.
- [CrossRef] [Google Scholar]
- Urological anomalies associated with obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome, a case series. J Pediatr Surg Case Rep. 2020;52:101358.
- [CrossRef] [Google Scholar]
- Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: Management and follow-up. Fertil Steril. 2007;87:918-22.
- [CrossRef] [Google Scholar]
- MRI findings of obstructed hemivagina and ipsilateral renal agenesis (OHVIRA syndrome) with a blind megaureter: Case report. Investig Magn Reson Imaging. 2015;19:196-9.
- [CrossRef] [Google Scholar]
- Herlyn-Werner-Wunderlich syndrome: Preand post-surgical MRI and US findings. Abdom Imaging. 2015;40:2667-82.
- [CrossRef] [Google Scholar]
- Herlyn-Werner-Wunderlich syndrome: Uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol. 2007;37:657-65.
- [CrossRef] [Google Scholar]
- Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. 2012;12:4.
- [CrossRef] [Google Scholar]
- Ectopic blind ureter with ipsilateral renal agenesis: A case report. Eur J Radiol. 1995;20:77-9.
- [CrossRef] [Google Scholar]
- Blind megaureter with ipsilateral renal agenesis and mullerian anomaly: MR findings in a case. Clin Imaging. 1999;23:184-6.
- [CrossRef] [Google Scholar]
- Herlyn-Weber-Wunderlich syndrome with ectopic ureter in prepubertal female. J Indian Assoc Pediatr Surg. 2014;19:103-5.
- [CrossRef] [Google Scholar]
- Didelphic uterus and obstructed hemivagina: Recurrent hematometra in spite of appropriate classic surgical treatment. Gynecol Obstet Invest. 2007;63:98-101.
- [CrossRef] [Google Scholar]
- Embryological observations on the female genital tract. Hum Reprod. 1992;7:437-45.
- [CrossRef] [Google Scholar]
- Experimental contributions to the study of the embryology of the vagina. Hum Reprod. 2006;21:1623-8.
- [CrossRef] [Google Scholar]
- The need for earlier diagnosis of obstructed hemivagina and ipsilateral renal agenesis/anomaly (OHVIRA) syndrome in case of renal agenesis in girls-case report and review of the literature. J Clin Med. 2023;12:7284.
- [CrossRef] [Google Scholar]







