Translate this page into:
A rare case of paralytic rabies presented with acute flaccid transverse myelitis in case of inadequate post-exposure prophylaxis
*Corresponding author: Pavankumar Suraparaju Varaprasadvarma, Department of Radiology, Government Medical College, Aurangabad, Maharashtra, India. svpavank93@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Suraparaju Varaprasadvarma P, Pawar A, Rote Kaginalkar V. A rare case of paralytic rabies presented with acute flaccid transverse myelitis in case of inadequate post-exposure prophylaxis. Case Rep Clin Radiol. doi: 10.25259/CRCR_26_2023
Abstract
Rabies is a fatal infectious disease caused by rabies lyssavirus, mainly transmitted to humans by the bite of rabid mammals. Rabies can present in encephalitic and paralytic types. Paralytic rabies presents with acute flaccid transverse myelitis. We report a rare case of paralytic rabies with inadequate post-exposure prophylaxis (PEP). A 19-year-old male was admitted with paraplegia and associated bladder and bowel incontinence for 2 days. He had history of Category III bite by a street stray dog and received inadequate PEP 3 months back which was revealed later. On imaging of dorsal spinal cord magnetic resonance imaging, there was a long-segment T2 and short-tau inversion recovery (STIR) hyperintense signal in central gray matter of dorsal cord with involvement up to part of conus medullaris. Cerebrospinal fluid analysis showed elevated microprotein with lymphocyte predominance. Clinical and laboratory findings supported diagnosis of rabies induced acute transverse myelitis. Incomplete PEP has been frequently reported in cases developing paralytic rabies. Adequate PEP according can easily prevent this disease.
Keywords
Magnetic resonance imaging
Acute transverse myelitis
Dog bite
Inadequate post-exposure prophylaxis and paralytic rabies
INTRODUCTION
Rabies is a fatal infectious disease, caused by rabies lyssavirus, a neurotropic virus belongs to rhabdoviridae family of RNA virus mainly transmitted to humans and animals through bites by rabid mammals. Rabies can present in two forms – classic encephalitic (80%) and paralytic atypical (dumb-20%) types.[1-3] Paralytic rabies presents with acute flaccid transverse myelitis,[1,3] but when it presents atypically as paralytic form, it may become difficult to distinguish from Guillain–Barré syndrome or acute transverse myelitis ATM of other causes,[2,4] when history is concealed.[1,3,5,6] Paralytic rabies presents with acute flaccid transverse myelitis and is more common in patients who receive post-exposure anti-rabies vaccination without rabies immunoglobulins (RIG). ATM is a clinical syndrome that involves the spinal cord, resulting in varying degrees of sensory alterations, weakness and autonomic dysfunction.[1] Only few cases of paralytic rabies in inadequate post rabies exposure prophylaxis have been reported so far in India.[1,2,5]
CASE REPORT
A 19-year-old male presented with paraplegia since 2 days with associated bladder and bowel incontinence. He had fever for 3 days before the onset of weakness. His power in lower limbs was 0/5, with hypotonia and areflexia. His cranial nerve functions and higher mental status were normal at the time of presentation and scanning. The history of unprovoked stray dog bite on his leg 3 months back followed by single dose of anti-rabies vaccine without anti-RIGs (Incomplete/inadequate post-exposure prophylaxis [PEP]) was given later on provoking after the patient’s neurological status deteriorated. The status of that dog was not known to the patient’s relatives. There was no history of sensory loss or trauma. On clinical examination, his power in both lower limbs was 0/5. Weakness was accompanied with hypotonia, areflexia, and non-elicitable plantar reflexes. Power in both upper limbs was normal. No sensory deficits were noted. His cranial nerve functions and higher mental status were normal at the time of presentation and scanning. There were no signs of meningeal irritation. No altered sensorium/loss of consciousness/delirium/seizure episodes. The patient was advised magnetic resonance imaging (MRI) spine by the physician. On MRI of dorsolumbar spine, long-segment T2 hyperintense signal was noted in central gray matter of spinal cord from D2 to D12 vertebral bodies’ levels with involvement up to part of conus medullaris [Figure 1]. The lesions described on T2w and STIR, MRI images of dorsal spine were showing restriction on diffusion weighted images [Figure 2]. The following laboratories investigations were done. Cerebrospinal fluid (CSF) analysis showed lymphocyte predominance (98%), with cell count–25 white blood cell/mm3 and elevated microprotein–139 mg/dL and normal glucose.
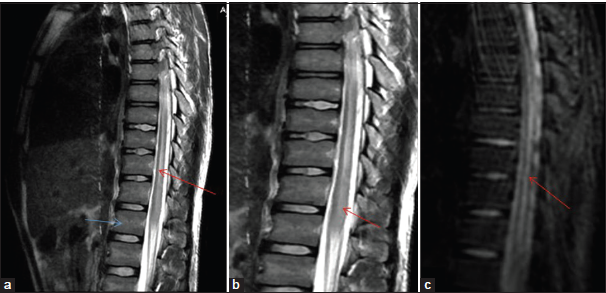
- (a) MRI dorsal spine saggital showing long segment T2 hyperintense signal (red arrow) in central gray matter of dorsal cord from D2 to D12 vertebral bodies (blue arrow). (b) Zoomed image showing involvement upto part of conus medullaris (red arrow) and (c) STIR dorsal spine image showing hyperintense signal in cord (red arrow). MRI: Magnetic resonance imaging, STIR: Short-tau inversion recovery.
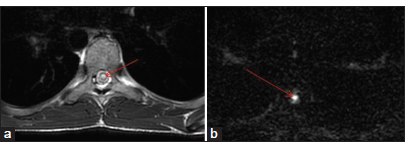
- (a) Axial T2W showing hyperintense signal (red arrow) in central grey matter of dorsal cord. (b) Corresponding DWI image showing restriction hyperintense signal marked by red arrow. DWI: Diffusion-weighted imaging.
The imaging diagnosis given was ATM with suggested evaluation for CSF antibodies. On the next day, patient developed encephalitic features (Hydrophobia, altered sensorium) of rabies and expired. Then, on provoking the relatives, history of being bitten by dog 3 months ago in his leg (Category III) for which he had received one dose of rabies vaccine (cell culture-derived vaccines [CCDV]) was given but did not take further doses due to lack of awareness. Retrospectively, diagnosis of paralytic rabies presenting as ATM – in case of inadequate PEP was made as no encephalitis features were present at time of scanning.
DISCUSSION
Paralytic rabies presents with paralysis of limbs, bladder, and bowel incontinence. It may become difficult to diagnose particularly when history is concealed.[2] In this case, the patient presented as atypical paralytic form, since features of encephalitis were absent at the time of presentation. Paralytic rabies presents with acute flaccid transverse myelitis and is more common in patients who received PEP anti-rabies vaccination without RIGs. Das et al.[6] reported that etiologies of transverse myelitis or myelopathy are the following:-29.26% post-infectious, 19.51% demyelination, 3.65% vascular and vasculitis (multisystemic disease-systemic lupus erythematosus (SLE)/Behcet’s),[4] and 1.21% (toxic etiology). The close differentials of paralytic rabies are Guillian-Bare syndrome or myelitis of other causes as mentioned in Das et al. The factor that helps to distinguish guillian-Barre syndrome (GBS) and ATM due to other causes is the rapidity with which the rabies illness progresses and proves fatal in 5–10 days.[2] In humans, the incubation period of rabies from infection to clinical disease averages between 15 and 90 days. Thus, it is possible to prevent clinical rabies in humans, even after exposure occurs, through prompt and effective PEP including: Effective washing of all wounds that occurred during exposure, administrating modern purified CCDV and embryonated egg based rabies vaccines and administration of RIG in case of category III bite is indicated according to country guidelines and World Health Organization recommendations.[7,8] The 5 dose, 2-1-1 dose, and 4 dose regimens are followed in PEP. Existing vaccine regimens for rabies PEP are close to 100% effective.[8,9] The expected number of rabies deaths in patients receiving PEP after a confirmed rabies exposure is fortunately extremely low.[7] In our case, a single dose of PEP rabies vaccine (CCDV) was only given after category III dog bite without RIG, which is incomplete and inadequate PEP. In our case, the patient was not aware of the full dose regimen that leads to incomplete prophylaxis. In paralytic rabies, MRI shows T2w hyperintense signal in spinal cord and medulla is more pronounced than other etiologies.[1,2,4,5] Computed tomography shows bilateral symmetric, non-enhancing hypodense lesions involving the basal ganglia but not sensitive for other regions of the brain such as brainstem and hypothalamus. MRI findings in both encephalitic and paralytic forms show ill-defined T2w hyperintense lesions involving the dorsal aspect of the medulla, tegmentum of pons, periaqueductal gray matter, collicular plate, central white matter of the midbrain, deep and subcortical white matter, hippocampi, medial aspects of the thalami, and in the hypothalamus on both sides of midline.[10] MRI findings in paralytic rabies shows T2w hyperintense signal in medulla extending to spinal cord associated with cord expansion. Early phase of disease does not reveal enhancement on MRI, while mild-to-moderate enhancement of the hypothalamus, brainstem, and gray matter of the cord may be seen as the patient neurological status deteriorates. The brachial plexus is an exception and can show enhancement in the early prodromal phase of the disease, which we can look for in case of suspicion.[10] The delayed presentation of weakness is explained by which spinal cord anterior horn motoneuron resists to cytolysis and apoptosis with rabies virus infection suggesting an escape phenomenon.[11] In paralytic rabies, limb weakness is predominantly due to peripheral nerve inflammation and demyelination but not due to anterior horn cell dysfunction.[11-13] CSF analysis shows lymphocytes predominance with elevated microproteins and rise in rabies virus neutralizing antibody titer.[4] Paralytic rabies may become difficult to diagnose particularly when history is concealed.[2] The causes of incomplete PEP in our country are illiteracy, decreased accessibility, and availability of RIG and cost factor.[9] Incomplete post-exposure prophylaxis fails to protect against rabies and may clinically mimic as Guillain–Barre syndrome.[14] If the patient had received adequate PEP, the onset of paralytic rabies could have been prevented.
CONCLUSION
In a flaccid paralytic patient who progresses rapidly to encephalitis with transverse myelitis evident on imaging, rabies should be strongly considered and history should be provoked accordingly. Incomplete PEP has been frequently reported in cases developing paralytic rabies which has preventable factors. Early diagnosis of rabies does not have any impact on patient’s prognosis, but it enables prompt institution of public health measures.
TEACHING POINT
In an ATM, the patient with paralytic features who progresses rapidly to encephalitis rabies should be strongly considered and history should be provoked accordingly.
MCQs
-
Rabies virus belongs to which family of virus
Rhabdoviridiae
Metaviridae
Retroviridae
Hepadnaviridae
Answer Key: a
-
Etiologies of transverse myelitis is/are the following
Post-infectious
Both a and c
Vasculitis (multisystemic disease-SLE/Behcet’s)
None
Answer Key: b
-
In paralytic rabies MRI imaging findings are
T2 hyperintense signal in cord
Diffusion restriction of lesions
STIR hyperintensity
All of the above
Answer Key: d
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Paralytic rabies: An acute flaccid myelitis after inadequate post exposure prophylaxis. Trop Doct. 2019;49:301-2.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical rabies with MRI findings: Clue to the diagnosis. BMJ Case Rep. 2011;2011:bcr0520114234.
- [CrossRef] [PubMed] [Google Scholar]
- Acute transverse myelitis at the conus medullaris level after rabies vaccination in a patient with behcet's disease. J Spinal Cord Med. 2007;30:294-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Transverse Myelitis in Post Rabies Vaccination. :1385-1387. Available from: https://edupediapublications.org/journals [Last accessed on 2023 Feb 21]
- [Google Scholar]
- Profile of non-compressive myelopathy in eastern India: A 2-year study. Acta Neurol Scand. 1999;99:100-5.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating new rabies post-exposure prophylaxis (PEP) regimens or vaccines. Vaccine. 2019;37:A88-93.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.coemed.org/files/stanags/02_AJMEDP/AJMedP-4-11_SRD_EDA_V1_E_2561.pdf [Last accessed on 2024 Nov 13]
- Death from rabies: The reason being poor compliance to vaccination or it's failure. J Family Med Prim Care. 2020;9:4437-0.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging in rabies encephalitis: A rare entity. Ann Indian Acad Neurol. 2016;19:125-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of escape phenomenon of spinal cord and brainstem in human rabies. BMC Infect Dis. 2005;5:104.
- [CrossRef] [PubMed] [Google Scholar]
- Paralytic rabies: A clinic-pathological study. Brain. 1980;103:789-802.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiology of human paralytic rabies. J Neurovirol. 2005;11:93-100.
- [CrossRef] [PubMed] [Google Scholar]
- Paralytic rabies: A guillainbarre syndrome mimic-N. QJM. 2019;112:365-6.
- [CrossRef] [PubMed] [Google Scholar]







