Translate this page into:
A rare case of hepatic hydatid cyst with cystobiliary communication causing obstructive jaundice
*Corresponding author: Veeraputhiran SenthilVelmurugan, Department of Radiodiagnosis, KAP Vishwanatham Government Medical College, Tiruchirapalli, Tamil Nadu, India. drsvmrdkapv@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: SenthilVelmurugan V, Muthupraveen K. A rare case of hepatic hydatid cyst with cystobiliary communication causing obstructive jaundice. Case Rep Clin Radiol. doi: 10.25259/CRCR_85_2024
Abstract
Hepatic hydatid cysts remain common in certain regions, including Southeast Asia. Among the complications, intrabiliary rupture and cystobiliary communication (CBC) are rare and challenging to detect through imaging. These complications are associated with higher post-operative mortality and morbidity. Here, we present a case of a 52-year-old male with acute abdominal pain and jaundice, diagnosed with a ruptured hepatic hydatid cyst with CBC and daughter cysts causing obstructive jaundice. Surgical intervention involved laparotomy, de-roofing, partial capitonnage, omentoplasty, and primary closure of the CBC.
Keywords
Hydatid cyst
Cystobiliary communication
Daughter cyst
Obstructive jaundice
Sphincterotomy
INTRODUCTION
Echinococcosis is a zoonotic disease caused by the larvae of Echinococcus granulosus and Echinococcus multilocularis. Hydatidosis has a global presence, with an annual incidence of 1–200/100,000 people. It is endemic in regions such as the Mediterranean, the Middle East, Eastern Europe, South America, and parts of India, especially Andhra Pradesh and Tamil Nadu. The infection typically results in hydatid cysts, mainly in the liver (60–70%) and lungs (20–30%).[1] Diagnosis is based on epidemiological, clinical factors, chest and abdominal X-ray, ultrasonography, and computed tomography (CT) scan, which should identify cysts characteristics, and the diagnosis is confirmed by detecting specific antibodies (immunodiagnostic test) and confirmed by specific antibody detection. Although generally benign, the disease can have serious complications, including secondary infections and ruptures, making treatment necessary in most cases.
CASE REPORT
A 52-year-old male was referred to us with a complaint of abdominal pain lasting 6 days, which was progressively worsening and radiating to the back, accompanied by nausea and non-bilious vomiting for 3 days. There was no history of fever. The patient had experienced similar pain in the past and had sought native treatment for it. He has no history of comorbidities but has been a known alcoholic for the past 7 years. On physical examination, tenderness and voluntary guarding were noted over the right hypochondrium and epigastric region, with bowel sounds present. Clinically, the patient was diagnosed with acute pancreatitis. Initial blood investigations were within normal limits.
Two days after admission, the patient developed jaundice, with clinical findings consistent with obstructive jaundice. The total bilirubin level increased from 0.5 mg/dL to 5.6 mg/dL within 2 days, accompanied by elevated liver enzymes (serum glutamic oxaloacetic transaminase: 108 U/L, serum glutamate pyruvate transaminase: 83 U/L, and alkaline phosphatase [ALP]: 447 U/L). Retrospective history revealed the patient had kept two dogs at home 7-years-ago. An abdominal ultrasound (USG) SenthilVelmurugan and Muthupraveen: A rare cyst material causing obstructive jaundice [Figure 1] performed on the 2nd day of admission revealed an 18 × 13 cm lesion with multiple daughter cysts along the periphery and a central altered echogenic component in the right liver lobe. The lesion had a thin hyperechoic rim and echogenic walls between the daughter cysts, with mild intrahepatic biliary radicle (IHBR) dilatation, a distended gallbladder (GB) containing echogenic sludge, and a dilated common bile duct (CBD) measuring 10 mm with sludge-like material.
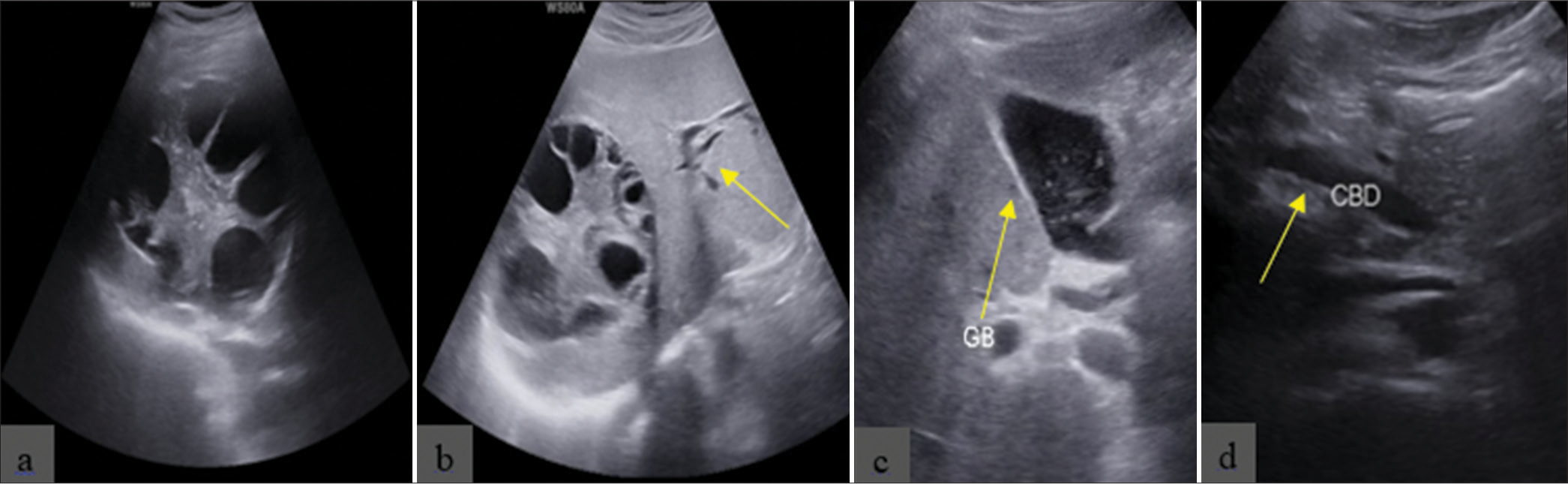
- Ultrasound shows (a) hepatic hydatid cyst with multiple daughter cysts involving the right lobe of the liver predominantly in segment 8, (b) mild intrahepatic biliary radicle dilatation (yellow arrow), (c) gallbladder (GB) with sludge-like material with hyperechoic foci (yellow arrow), and (d) common bile duct dilation (CBD) (yellow arrow) measures 10 mm.
A contrast-enhanced CT (CECT) [Figure 2] scan showed a 19 × 13 cm measuring well-defined, non-enhancing, multilocular cystic lesion in segment 8 of the right liver lobe, with thick-walled daughter cysts lining the periphery and central soft-tissue component. The lesion has a thin rim of peripheral calcification. There was mild IHBR dilatation in both systems, a grossly distended GB with sludge without wall thickening or calculi, and a dilated CBD with sludge-like material measuring 10 mm, with no obvious cystobiliary communication (CBC). Repeat blood tests showed continued elevation of total bilirubin to 13.6 mg/dL, leading to a magnetic resonance cholangiopancreatography (MRCP) being advised.
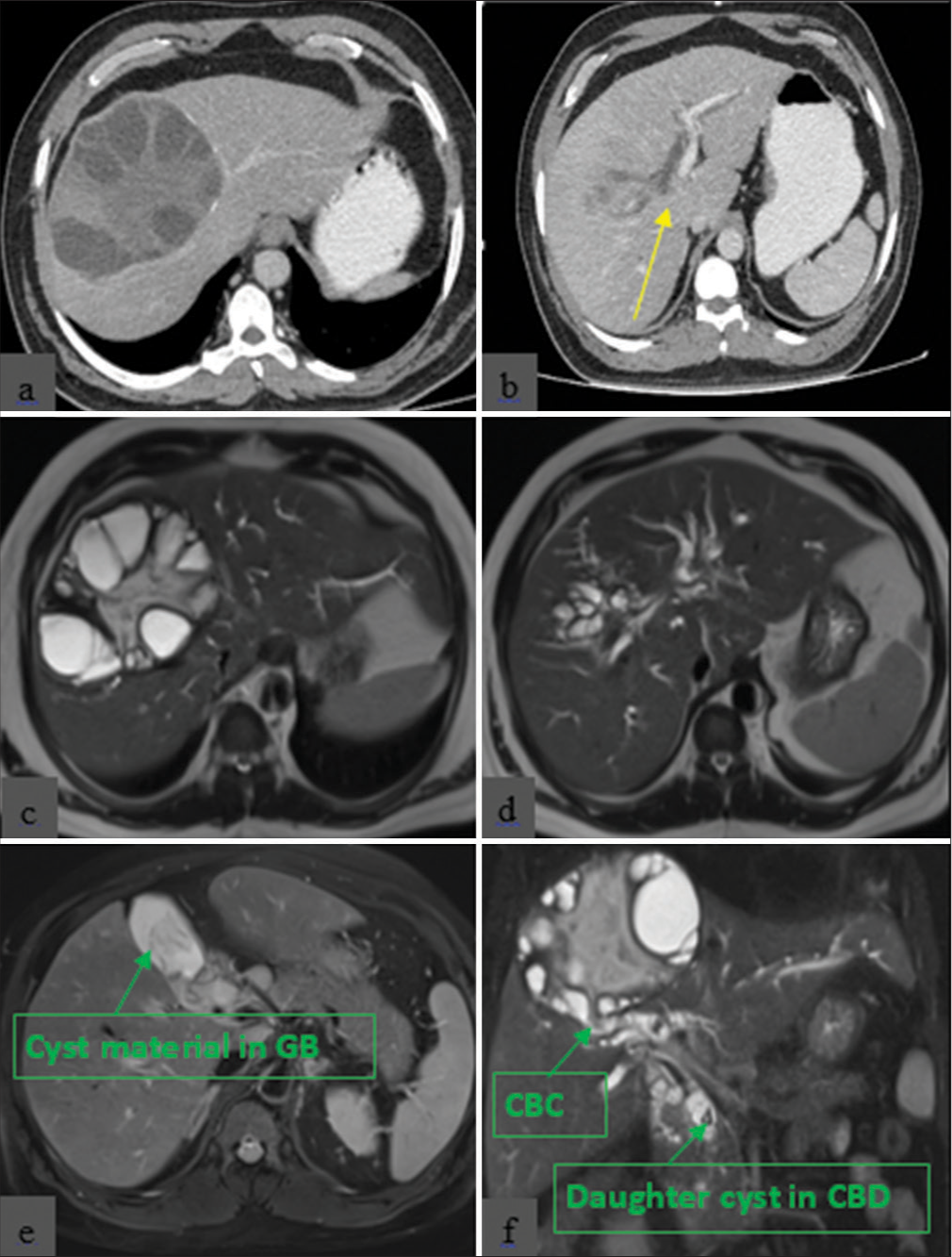
- Contrast-enhanced computed tomography shows (a) hepatic hydatid cyst with multiple daughter cysts, (b) intrahepatic biliary radicle (IHBR) dilatation (yellow arrow) and (c) magnetic resonance cholangiopancreatography shows hepatic hydatid cyst with multiple daughter cysts with (d) IHBR dilatation and (e) distended gallbladder (GB) with daughter cyst material within the GB and (f) cystobiliary communication (CBC) with daughter cysts in the common bile duct (CBD).
The MRCP [Figure 2] revealed a well-defined, thick-walled cystic lesion with daughter cysts communicating with the right anterior sectoral duct, gross IHBR dilatation in both systems, a distended GB with sludge, and a dilated CBD measuring 17 mm with multiple irregular filling defects that appeared hypointense on T1-weighted (T1W) and T2-weighted (T2W) imaging. The largest defect, measuring 10 mm, was present in the distal CBD, representing a daughter cyst. The final impression was a ruptured hepatic hydatid cyst in the right liver lobe with CBC and multiple daughter cysts in the CBD, causing obstructive jaundice.
Due to rising total bilirubin levels (16.5 mg/dL total and 9.6 mg/dL direct on day 12 since admission) and to confirm the diagnosis and to remove cyst materials from the biliary system, the patient underwent endoscopic retrograde cholangiopancreatography (ERCP) [Figure 3]. An endoscopic sphincterotomy was performed, and a large amount of membranes and daughter cysts were removed. The patient was then started on albendazole 400 mg once daily. Within 4 days, the total bilirubin level dropped to 5 mg/dL.
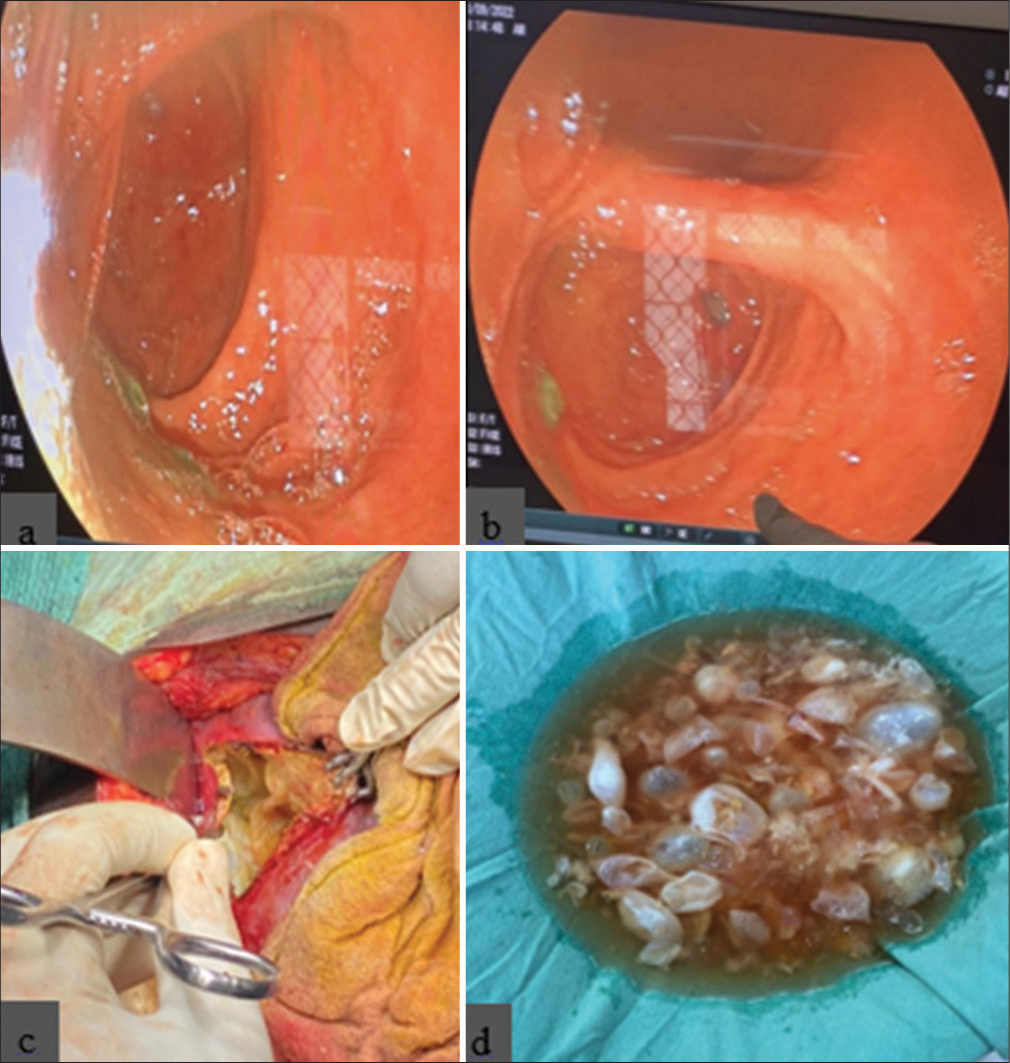
- Endoscopic retrograde cholangiopancreatography shows (a and b) daughter cysts in the second part of the duodenum and (c) deroofing, evacuation of cyst content, and (d) removed hydatid cyst during surgery.
After 3 months of medical management, the patient underwent deroofing, pericystectomy with evacuation of cyst contents, primary repair of the CBC, and omental patch closure. During surgery, communication with the right anterior sectoral hepatic duct was confirmed.
DISCUSSION
CBC occurs when the cyst’s size gradually increases, leading to a rise in intracystic pressure. When this pressure surpasses the ductal pressure, the cyst wall and duct weaken at the point of contact, resulting in CBC and allowing bile to enter the cyst. These communications are typically small and asymptomatic. In our patient, multiple daughter cysts caused distal CBD obstruction, leading to obstructive jaundice.[2]
Abdominal USG can reveal features such as anechoic cysts, multiseptate cysts, floating membranes, daughter cysts, and calcifications. Based on USG appearance, hydatid cysts are classified into five categories, with the World Health Organization Informal Working Group on Echinococcosis categorizing them into six types.[1,2]
CT scans of the abdomen help determine the cyst’s location, wall thickness, presence of daughter cysts, floating membranes, and any calcifications. Magnetic resonance imaging (MRI) is particularly useful for visualizing the pericyst, hydatid matrix (or hydatid sand, which is debris consisting of freed scolices), and daughter cysts.[3] The pericyst usually appears with low-signal intensity on T1W- and T2W images due to its fibrous composition. The hydatid matrix is hypointense on T1W images and hyperintense on T2W images. Daughter cysts, when present, appear hypointense relative to the matrix on both T1W- and T2W images, while floating membranes show low signal intensities on both.[2,3]
ERCP is an essential management tool for hydatid cysts in the extra-biliary tree, whether primary or as a complications of liver hydatid cysts. It aids in clearing the biliary tree, closing fistulas, and managing biliary leaks, often followed by laparoscopic cholecystectomy when the hydatid cyst involves the GB.[2] Sphincterotomy is frequently necessary in patients with obstructive jaundice.
CONCLUSION
Early diagnosis of CBC and intrabiliary rupture is crucial to reducing complications and morbidity. Ultrasonography and computed tomography (CT) are key diagnostic tools that help identify complications and guide treatment planning. CECT and MRCP are the preferred investigations for diagnosing complicated liver hydatid cysts, including CBC, cysto-enteric fistula, and spread to the lungs or pleura. ERCP has become the primary diagnostic and therapeutic approach for managing primary hydatid cysts in the biliary tree.
TEACHING POINTS
Diagnosis of the hydatid cyst is usually by clinical history imaging. Liver function tests may be normal, or there may be an increase in ALP or gamma-glutamyl transferase in a few patients, which are suggestive of CBC.[1,2]
The presence of CBC can be suggested by the presence of fat-fluid level within hepatic hydatid cysts, which have been described on CT and MRI as represented lipid material within the bile.[3]
Suspecting the presence of CBC begins with pre-operative factors detected in the history, examination, laboratory, and imaging findings. Obstructive jaundice and cholangitis are sensitive indicators of the presence of a frank CBC in more than 60% of the cases.[2,3]
MCQs
-
Predictor of CBC which of the following is true?
Cyst size >10 cm
Clinical jaundice
Elevated liver enzymes
All of the above
Answer Key: d
-
Which segment of the liver has the highest chance of CBC?
Segment 7 and 8
Segment 5 and 6
Segment 4 and 5
Segment 5 and 8
Answer Key: c
-
Investigation of choice for confirming CBC?
USG
CECT
MRCP
ERCP
Answer Key: d
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hydatid disease: Radiologic and pathologic features and complications. Radiographics. 2000;20:795-817.
- [CrossRef] [Google Scholar]
- Hepatic hydatid cyst with cystobiliary communication and cystoduodenal fistula. Cureus. 2021;13:e17473.
- [CrossRef] [Google Scholar]
- Liver hydatid cyst with cystobiliary communication: Laparoscopic surgery remains an effective option. J Minim Access Surg. 2018;14:230-5.
- [CrossRef] [Google Scholar]







