Translate this page into:
Exposing the culprit: Triquetrohamate impaction syndrome as a cause of refractory ulnar-sided wrist pain
*Corresponding author: Ebinesh Arulnathan, Department of Imaging and Interventional Radiology, Meenakshi Mission Hospital and Research Centre, Madurai, Tamil Nadu, India. ebineshjezreel@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arulnathan E. Exposing the culprit: Triquetrohamate impaction syndrome as a cause of refractory ulnar-sided wrist pain. Case Rep Clin Radiol. doi: 10.25259/CRCR_24_2025
Abstract
Ulnar-sided wrist pain is a common presentation with complex diagnostic challenges. The diagnostic challenges are due to the complexity of anatomical organization and the histological diversity within a small anatomical region. In this case report, we present a case of triquetrohamate impaction syndrome, an uncommon cause of ulnar-sided wrist pain with an emphasis on the role of imaging. The case involves a 27-year-old female clerk with persistent wrist pain, revealing significant findings on magnetic resonance imaging, including reduced triquetrohamate joint space, associated bone marrow edema, and degenerative changes. Our patient had a good clinical response to conservative management. It is essential that the clinicians and radiologists possess adequate knowledge and awareness regarding triquetrohamate impaction syndrome for early diagnosis and treatment.
Keywords
Magnetic resonance imaging
Triquetrohamate articulation
Triquetrohamate impaction syndrome
Ulnar-sided wrist pain
INTRODUCTION
Ulnar-sided wrist pain is a common presentation with complex diagnostic challenges. The diagnostic challenges are due to the complexity of anatomical organization and the anatomical tissue diversity within a small anatomical region. The various types of tissues include cartilage (triangular fibrocartilage complex [TFCC]), bones (ulnar styloid and carpal bones such as hamate, triquetrum, lunate, and pisiform), ligament (lunotriquetral ligament), tendons (extensor carpi ulnaris [ECU] and flexor carpi ulnaris), and nerve (ulnar nerve).[1]
Moreover, the cause of ulnar sided wrist pain can be multifactorial where in the primary cause can co-exist with the associated complications, further worsening the pain. Therefore, the motive of management is based on recognizing and addressing the primary cause to prevent recurrence or further clinical worsening. Knowledge of relevant anatomy, causes, their clinical presentation, and their radiological features are significant in driving clinical decisions and outcomes.
We present a brief overview on triquetrohamate impaction syndrome, an underdiagnosed refractory cause of ulnar-sided wrist pain and emphasize the role of imaging with a case illustration.
CASE REPORT
A 27-year-old female, a clerk by occupation presented with persistent, unexplained ulnar-sided wrist pain since the past 2–3 years. The pain was gradually progressive and notably intensified over the past couple of months. Despite conservative treatment with long-term non-steroidal anti-inflammatory drugs (NSAIDs), at a local GP clinic, the pain persisted and worsened. Consequently, she was referred to our facility for further management. Magnetic resonance imaging (MRI) was performed [Figure 1], which revealed significant reduction in the triquetrohamate joint space, predominantly involving the ulnar aspect and associated bone marrow edema in triquetrum and hamate. In addition, triquetral osteophyte and subchondral cystic changes were also seen, representative of resultant degeneration. Carpometacarpal joint effusion was also noted. Therefore, a diagnosis of triquetrohamate impaction syndrome with secondary degenerative arthropathy was made. The patient was initially treated with immobilization with splint and lifestyle modifications which led to partial response. Later, the patient required local corticosteroid infiltration following which there was complete regression of symptoms.
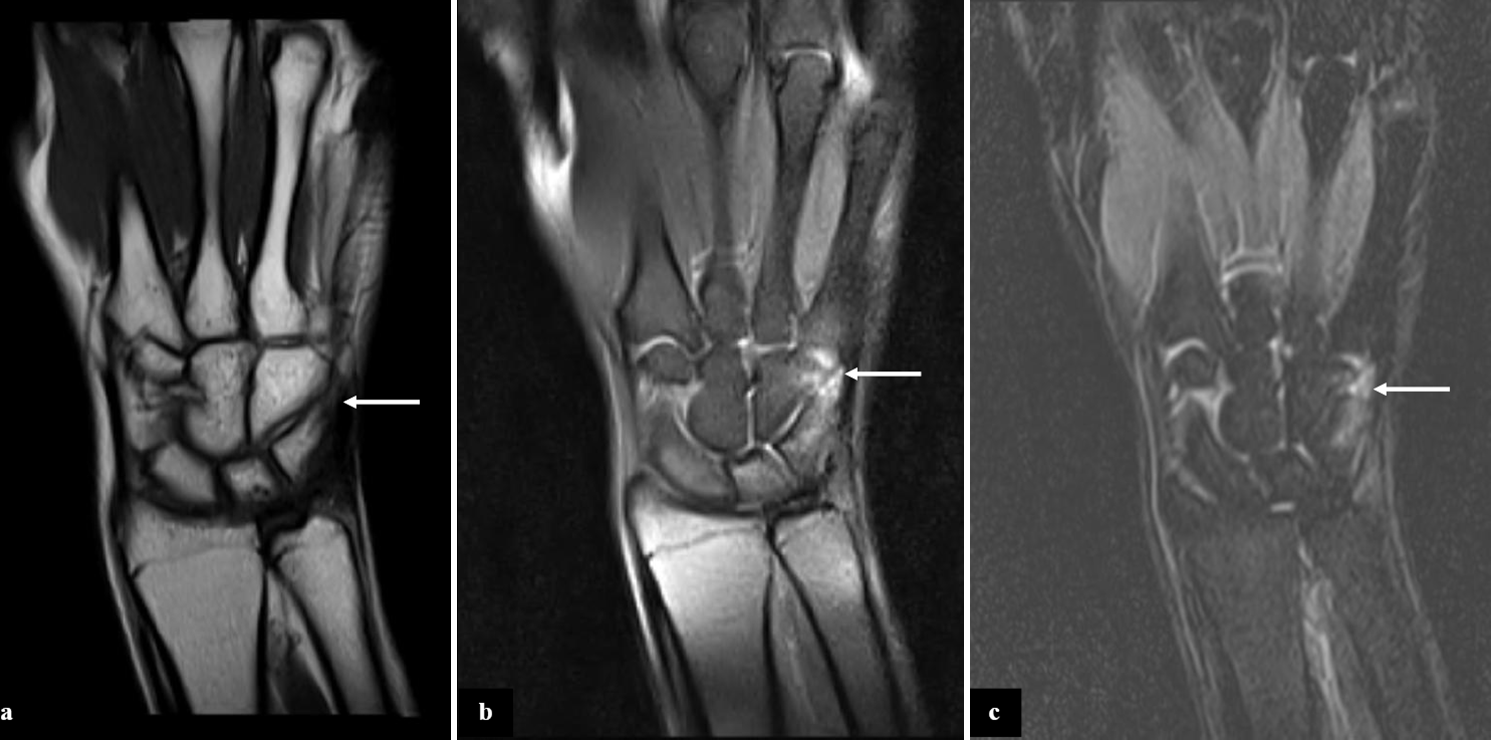
- Coronal (a) T1 TSE, (b) PD FS, and (c) short-tau inversion recovery images show features of triquetrohamate impaction (white arrows) characterized by reduced triquetrohamate joint space with subchondral marrow edema in triquetrum and hamate bones, triquetral osteophyte, and subchondral cystic changes. TSE: Turbo spin echo; PD: Proton density; FS: Fat saturated.
DISCUSSION
Triquetrohamate impaction syndrome is a frequently overlooked etiology of ulnar-sided wrist pain, often resulting in delayed diagnosis, with an average reported delay of 7.4 months.[2] It is prevalent among individuals engaged in activities requiring ulnar deviation and dorsiflexion. The pathogenesis of this condition can be explained by the dynamics of triquetrum hamate articulation.[3] During ulnar deviation and dorsiflexion, the triquetrum translates medially and dorsally over the helicoid slope of the hamate bone, accentuating triquetrohamate contact. Repetitive motion with resultant repetitive micro injury of the opposing articular surfaces leads to pathological impaction.
The presence of localized tenderness on the dorsal ulnar aspect of the triquetrohamate joint, exacerbated during forced dorsiflexion and ulnar deviation should raise a suspicion of triquetrohamate impaction syndrome.[4] Radiological evaluation, including radiographs and MRI, play a pivotal role in diagnosis. Pertinent radiological findings are triquetrohamate joint space narrowing, bone marrow edema, osseous changes, and synovitis.[5] Features of degeneration, such as osteophytes, loose bodies, subchondral cysts, and chondral loss can be demonstrated in patients with prolonged course of disease.[2] The osseous changes are better appreciated on computed tomography (CT) images. Radial deviation view on fluoroscopic arthrogram following contrast injection can be used for confirmation of the diagnosis in case of ambiguity.[2] Differential diagnoses include ECU tenosynovitis, TFCC tear, lunotriquetral ligament injury, and ulnocarpal impaction. Imaging plays an indispensable role in differentiating various causes, each of which possesses characteristic imaging features. ECU tendinopathy is characterized by increased proton density (PD) fat saturated (FS)/short-tau inversion recovery signal of the tendon with peritendinous fluid. Fluid signal extending along the medial aspect of ulna with distal radioulnar joint effusion and marrow edema in the ulnar styloid process are representative of TFCC tear. Injury to the lunotriquetral ligament presents as volar intercalated segment instability (VISI). Ulnocarpal impaction is associated with positive ulnar variance and usually follows distal radial fracture, eventually resulting in central TFCC or lunotriquetral tear.
Initial conservative therapy involves NSAIDs, immobilization, and avoidance of exacerbating activities. Corticosteroid injections may prove beneficial for non-responsive cases. Surgical intervention is reserved for refractory cases and includes arthroscopic synovectomy, removal of loose bodies, microfracture, and partial or total carpal excision.[2,6] Recognizing triquetrohamate impaction syndrome as an underreported cause of ulnar-sided wrist pain and general awareness of the associated clinical and radiological diagnostic features are imperative, as early diagnosis and therapy can mitigate significant morbidity.
DIFFERENTIAL DIAGNOSES
ECU tendinopathy: Peritendinous fluid and increased PD FS/STIR signal in the ECU tendon
TFCC Tear: Fluid signal along the medial ulna with distal radioulnar joint effusion
Lunotriquetral ligament injury: Associated with volar intercalated segment instability
Ulnocarpal impaction: Positive ulnar variance with lunotriquetral or central TFCC tear.
CONCLUSION
Triquetrohamate impaction syndrome is an under recognized cause of ulnar-sided wrist pain and is associated with significant morbidity if not recognized early in the course. Radiological investigations including radiograph and MRI are indispensable for diagnosing this condition. The radiological findings include reduced triquetrohamate joint space, bone marrow edema, and synovitis which can coexist with features of degenerative arthropathy. Failure to initial conservative therapy with NSAIDs and lifestyle modification will necessitate surgical intervention.
TEACHING POINTS
Triquetrohamate impaction syndrome is an underdiagnosed yet impairing cause of ulnar-sided wrist pain
MRI is the primary imaging modality for diagnosing triquetrohamate impaction syndrome, with characteristic imaging features including reduced joint space predominantly involving the ulnar aspect, subchondral bone marrow edema, osteophytes, and cystic changes
CT can help in better evaluation of bone changes such as subchondral sclerosis, osteophytes, and cortical irregularity
-
Dynamic imaging, such as fluoroscopic arthrography with radial deviation, can confirm impingement
Differential diagnoses include TFCC tears, lunotriquetral ligament injury, and ECU tendinopathy.
MCQs
-
Which of the following is the most characteristic imaging finding of triquetrohamate impaction syndrome on MRI?
Increased PD FS/STIR signal of the ECU tendon
Fluid signal extending along the medial aspect of the ulna with distal radioulnar joint effusion
Reduced triquetrohamate joint space with subchondral bone marrow edema and cystic changes
Positive ulnar variance with central TFCC tear
Answer Key: c
-
Which anatomical motion is primarily responsible for the pathogenesis of triquetrohamate impaction syndrome?
Radial deviation and palmar flexion
Ulnar deviation and dorsiflexion
Pronation and supination
Extension and flexion of the metacarpophalangeal joints
Answer Key: b
-
Which of the following is NOT a primary differential diagnosis of triquetrohamate impaction syndrome?
ECU tendinopathy
Ulnocarpal impaction
Scapholunate dissociation
Lunotriquetral ligament injury
Answer Key: c
Ethical approval
All procedures performed in this study involving a human participant were in accordance with the ethical standards of the institutional ethics committee at Sri Narayani Hospital and Research Centre, Vellore and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that Generative AI (ChatGPT4) was used for language improvement only.
Financial support and sponsorship: Nil.
References
- Imaging of ulnar-sided wrist pain. Can Assoc Radiol J. 2012;63:18-29.
- [CrossRef] [PubMed] [Google Scholar]
- Triquetrohamate impaction syndrome: An unrecognized cause of ulnar-sided wrist pain; its presentation further defined. Hand. 2017;12:382-8.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo triquetrum-hamate kinematics through a simulated hammering task wrist motion. J Bone Joint Surg Am. 2012;94:e85.
- [CrossRef] [PubMed] [Google Scholar]
- Triquetrohamate impaction syndrome: A case report. J Hand Surg Am. 1996;21:778-80.
- [CrossRef] [PubMed] [Google Scholar]
- Ulnar-sided wrist pain: Evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2012;37:1489-500.
- [CrossRef] [PubMed] [Google Scholar]
- Ulnar-sided wrist pain. Diagnosis and treatment. J Bone Joint Surg Am. 2004;86:1560-74.
- [CrossRef] [Google Scholar]







