Translate this page into:
Pathological laughter as an initial presentation of bilateral internal carotid artery agenesis
*Corresponding author: Anitha Jasper, Department of Radiology, Christian Medical College, Vellore, Tamil Nadu, India. anithapjp@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Eapen KC, Selvaganesan S, Jasper A, Prabhakar AT. Pathological laughter as an initial presentation of bilateral internal carotid artery agenesis. Case Rep Clin Radiol. doi: 10.25259/CRCR_59_2024
Abstract
In this case report, we describe a rare case of bilateral internal carotid artery (ICA) agenesis, with a peculiar symptom of inappropriate laughter preceding neurological manifestations. The patient’s atypical presentation included episodes of premature laughter, preceding symptoms of headache, numbness, and jerky movements in the upper limbs. Imaging studies revealed multiple acute infarcts in the anterior cerebral circulation territories bilaterally, along with non-visualization of bilateral ICAs. The absence of bilateral carotid canals further confirmed the diagnosis. Hypertrophied posterior communicating arteries and collaterals from the left external carotid artery were identified, contributing to compensatory circulation. The primary focus of treatment was on the conservative management of acute stroke symptoms, including regular monitoring to identify potential complications, especially the development of intracranial aneurysms. This case highlights the importance of multi-disciplinary collaborative efforts among radiologists, neurologists, and vascular surgeons for accurate diagnosis and effective treatment of rare vascular anomalies.
Keywords
Carotid agenesis
Internal carotid artery agenesis
Congenital vascular anomaly
INTRODUCTION
Bilateral internal carotid artery (ICA) agenesis is a rare congenital anomaly characterized by the absence of both ICAs, frequently accompanied by additional vascular anomalies. This has been found to occur in <0.01% of the population and can present with a range of neurological deficits stemming from compromised cerebral perfusion.[1] This case report depicts a 24-year-old lady with bilateral ICA agenesis who presented with episodes of premature laughter just before the manifestation of neurological symptoms. Our objective is to highlight the very unusual clinical presentation in our patient and to provide an overview of the imaging findings in bilateral ICA agenesis.
CASE REPORT
Brief history
A 24-year-old lady presented with complaints of headache and episodes of numbness involving the right side of her face and body for 1 month, and episodes of jerky movements of her upper limbs for 1 week, which were present only in the upright position and disappeared upon lying down. These episodes were often preceded by inappropriate laughter, with one episode of continuous laughter lasting for as long as 10 min. She did not have any relevant past history or family history of a similar illness.
Imaging
Magnetic resonance imaging (MRI) of the brain showed evidence of multiple acute infarcts involving the territories of the anterior circulation bilaterally [Figure 1]. Magnetic resonance angiogram showed non-visualization of bilateral ICAs. The posterior communicating arteries (PCOM) were hypertrophied, and a small saccular aneurysm (9 × 4 mm) was identified arising from the right PCOM, indenting the right medial temporal lobe, as seen in Figure 2. The ICAs were not visualized on a subsequent computed tomography (CT) angiogram [Figure 3]. The right middle cerebral artery (MCA) and anterior cerebral artery were reformed through the right PCOM. The cavernous segment of the left ICA was reformed from the accessory meningeal artery, a branch of the left external carotid artery (ECA) [Figure 2]. There were also extensive calcifications along the developed compensatory circulation, as seen in Figure 2. CT sections through the skull base showed the absence of bilateral carotid canals [Figure 3].
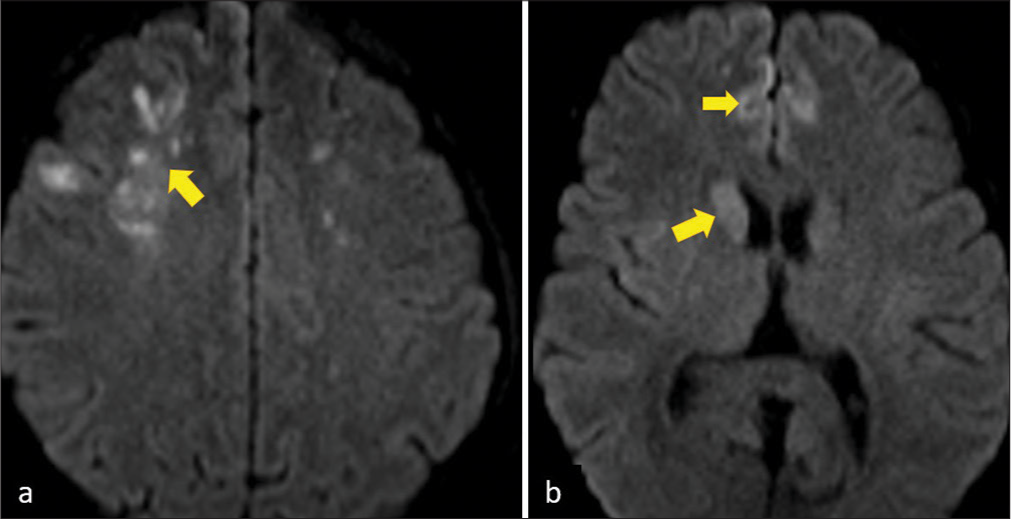
- Magnetic resonance imaging - Diffusion-weighted scans reveal multiple acute infarcts in (a) the frontal lobes and (b) right basal ganglia involving the anterior circulation of bilateral cerebral hemispheres (yellow arrows).
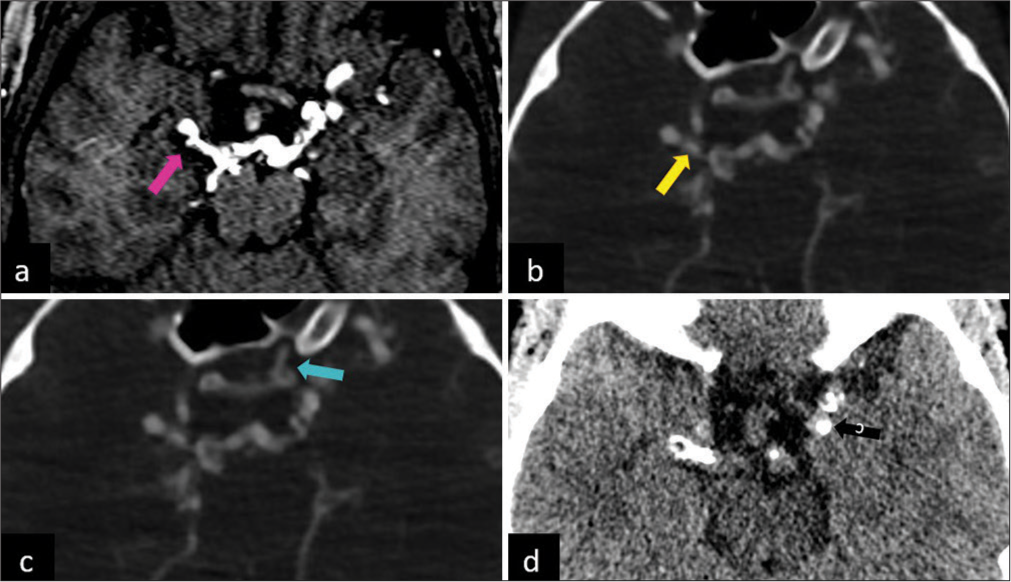
- (a) Magnetic resonance angiogram reveals an aneurysm arising from the right posterior communicating artery (magenta arrow). (b and c) Computed tomography (CT) angiogram study reveals the right posterior communicating artery reforming the right middle cerebral artery and anterior cerebral artery (yellow arrow) and a branch from the left external carotid artery reforming the cavernous segment of the left internal carotid artery (cyan arrow). (d) CT non-contrast study shows extensive calcifications along the compensatory circulation developed from the posterior circulation and the left external carotid artery (black arrow).
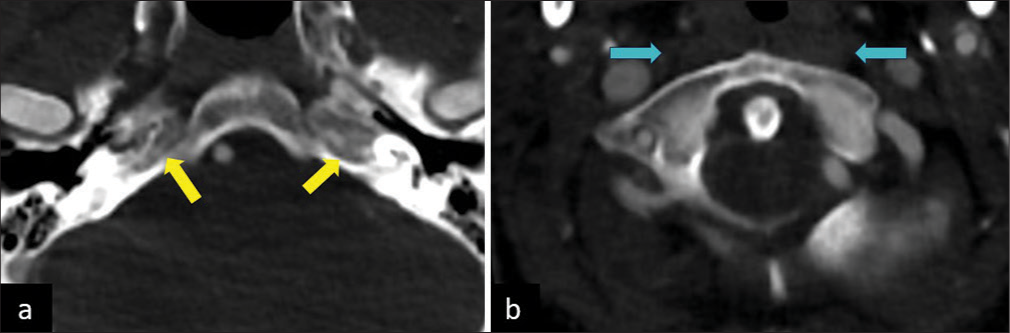
- (a) Axial computed tomography (CT) sections in the bone window reveal the absence of bilateral carotid canals (yellow arrows). (b) CT angiogram study reveals the absence of bilateral internal carotid arteries (ICAs) (cyan arrows indicate the expected location of ICAs).
Treatment and follow-up
The patient was managed conservatively for her acute stroke symptoms. As the CT angiogram showed adequate collateral circulation to the brain, no further interventional or neurosurgical options were considered at this point. She was planned for further follow-up with annual CT angiogram studies as a review of the literature showed a risk of development of new intracranial aneurysms.[1] She was reviewed in the outpatient department after 2 months and was doing well with no new neurological deficits.
DISCUSSION
Embryology
The ICAs are formed from the 3rd branchial arch arteries and the distal segments of the paired dorsal aortae and are fully formed by around 6 weeks of gestation.[2,3] The embryonic development of the ICA precedes the development of the skull base, which is formed during 5–6 weeks of gestation.[4] In cases of ICA agenesis, the carotid canal is absent, thereby helping to confirm the diagnosis.[5] Any insult or disruption to the normal embryonic development of the arteries of the brain during this time will result in the development of primitive collateral formation, which is supplied from the circle of Willis, persistent fetal circulation, or through skull base collaterals from the ECA.[6]
ICA agenesis
A review of literature conducted by Zhang et al. in 2018 showed 54 cases of ICA agenesis, of which 12 had bilateral ICA agenesis (22.2%). The common clinical manifestations included developmental delay (24.1%), subarachnoid hemorrhage (SAH) (22.2%), and transient ischemic attacks (TIAs) (20.4%). They were found to be asymptomatic in seven out of 54 cases (12.9%), likely due to maintenance of normal cerebral blood flow by collateral circulation. Associated aneurysms were seen in the cerebral circulation in 12 cases (22.2%).[7] SAH is a common presentation in patients with associated intracranial aneurysms which have ruptured. The increased incidence of intracranial aneurysms in patients with ICA agenesis may be related to intracranial hemodynamic changes as a result of the development of collateral circulation. In our case, the patient presented with abnormal movement of the upper limbs, which may be attributed to limb shaking TIA caused by a low flow state.
Pathological laughter can be observed in a range of neuro-psychiatric disorders, including stroke. Several theories suggest that pathological laughter in the setting of a vascular event, such as a left MCA stroke, may be connected to the involvement of the dominant hemisphere because of the critical role of the motor speech area in the processing of laughter.[8] It has also been suggested that the appearance of pathological laughter in stroke patients may be linked to the impact on brainstem structures such as the midbrain and pons, considering the involvement of cortical projections from these regions in the processing of laughter.[9] In our review of the literature, we found no evidence of pathological laughter being observed as a manifestation of carotid agenesis.
There were extensive calcifications seen along the collaterals developed from the vessels of the Circle of Willis. These may represent the chronic course of the disease and are probably secondary to altered hemodynamics.
Treatment options
Management strategies for bilateral ICA agenesis depend on the particular clinical characteristics, associated anomalies, and clinical presentation of the individual patient. Given the rarity of this condition, there is no universally accepted therapeutic regimen. The primary objective focuses on averting potential complications and improving cerebral perfusion. Surgical options such as superficial temporal artery-MCA bypass graft have been described as treatment options.[10] Patients with ICA agenesis have to be kept on follow-up, in particular, to screen for the development of any intracranial aneurysms, which may be treated by surgical or interventional treatment options.[4]
DIFFERENTIAL DIAGNOSIS
The various differential diagnosis to consider upon nonvisualisation of the carotid artery on CT or MRI imaging are listed in Table 1, along with specific imaging findings which may help differentiate between them.
| Differential diagnosis | Imaging findings |
|---|---|
| Carotid agenesis | Both the ICA and carotid canal are absent |
| Carotid aplasia | ICA may be absent, or a remnant of the ICA may persist Carotid canal is present |
| Carotid hypoplasia | ICA may be small, but regular Carotid canal is present |
| Carotid occlusion | It is a much more common entity Carotid canal is present Calcifications may be present to suggest atherosclerotic disease Extracranial ICA may show flow |
ICA: Internal carotid artery.
CONCLUSION
The very unusual clinical presentation in our patient, along with the concomitant absence of both ICAs, is very rare. Imaging modalities such as CT angiography and MRI have been instrumental in accurately identifying this anomaly and guiding appropriate treatment strategies. Considering the probability of concurrent vascular abnormalities and neurological deficits, an interdisciplinary approach involving radiologists, neurologists, and vascular surgeons is imperative for providing optimal care to affected individuals.
MCQs
-
Which of these is an essential finding to help distinguish carotid agenesis from aplasia?
Non-visualization of carotid artery
Absence of bony carotid canal
Presence of collateral circulation from contralateral ICA, vertebral artery, or ECA
None of the above
Answer: b.
-
What is the most common presentation of patients diagnosed with carotid agenesis?
Cerebral ischemia
Subarachnoid hemorrhage
Asymptomatic
None of the above
Answer: c.
-
An individual with carotid agenesis is prone to develop which of the following abnormalities?
Intracranial aneurysm
Intracranial bleed
Brain tumors
All of the above
Answer: a.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Congenital absence of the internal carotid artery: Case reports and review of the collateral circulation. AJNR Am J Neuroradiol. 2001;22:1953-9.
- [Google Scholar]
- A functional perspective on the embryology and anatomy of the cerebral blood supply. J Stroke. 2015;17:144-58.
- [CrossRef] [Google Scholar]
- Congenital absence of internal carotid artery with intercavernous anastomosis: Case report and systematic review of the literature. Interv Neuroradiol. 2016;22:473-80.
- [CrossRef] [Google Scholar]
- Internal carotid artery agenesis: A rare entity. Cureus. 2023;15:e36640.
- [CrossRef] [Google Scholar]
- Internal carotid artery agenesis with an intercavernous anastomosis: A rare case. J Stroke Cerebrovasc Dis. 2017;26:2442-5.
- [CrossRef] [Google Scholar]
- Congenital anomalies of the carotid arteries. Plast Reconstr Surg. 1968;42:283.
- [CrossRef] [Google Scholar]
- The clinical presentation and collateral pathway development of congenital absence of the internal carotid artery. J Vasc Surg. 2018;68:1054-61.
- [CrossRef] [Google Scholar]
- Pathological laughter as heralding manifestation of left middle cerebral artery territory infarct : Case report and review of literature. Neurol India. 2000;48:388.
- [Google Scholar]
- Pathological laughter as a symptom of midbrain infarction. Behav Neurol. 2004;15:73-6.
- [CrossRef] [Google Scholar]
- Pediatric moyamoya disease associated with ipsilateral internal carotid artery agenesis: Illustrative case. J Neurosurg Case Lessons. 2022;3:CASE22119.
- [CrossRef] [Google Scholar]








