Translate this page into:
An extremely rare culprit for a common crime: A case report on gastric duplication cyst associated with accessory pancreatic lobe
*Corresponding author: Kritika Sunil Bhatia, Department of Radiology, Seth G. S. Medical College and KEM Hospital, Mumbai, Maharashtra, India. kritika_bhatia@live.com
-
Received: ,
Accepted: ,
How to cite this article: Khan SA, Thakkar H, Alam Z, Bhatia KS. An extremely rare culprit for a common crime: A case report on gastric duplication cyst associated with accessory pancreatic lobe. Case Rep Clin Radiol. doi: 10.25259/CRCR_38_2024
Abstract
A 19-year-old 4-week postpartum woman came with acute onset pain in the abdomen for 2 days. She had similar complaint in her 7th antepartum month for which she had undergone an magnetic resonance imaging (MRI) examination elsewhere which was reported as pancreatic pseudocyst. Ultrasonogram of epigastric region revealed a cystic lesion with echogenic content and wall showing gut signature. Contrast-enhanced computed tomography scan confirmed the cystic lesion and additionally showed an accessory pancreatic lobe. MRI demonstrated the aberrant duct within accessory pancreatic lobe and its communication with main pancreatic duct.
Keywords
Accessory pancreatic lobe
Aberrant duct
Gastric duplication cyst
INTRODUCTION
The accessory pancreatic lobe is an extremely rare congenital anomaly defined as an accessory lobe of pancreatic tissue originating from main pancreatic gland and containing aberrant duct.[1] This anomaly is usually associated with gastric duplication cyst and the aberrant duct communicates with the main pancreatic duct (PD) and the duplication cyst. The gastric duplication cyst contains ectopic pancreatic tissue or gastric mucosa which is prone to hemorrhage and block aberrant duct leading to pancreatitis.
CASE REPORT
A 19-year-old, 4-week postpartum woman came with acute onset pain in the abdomen for 2 days. She had similar complaint in her 7th antepartum month for which she had undergone an magnetic resonance imaging (MRI) examination elsewhere. Ultrasonography, contrast-enhanced computed tomography (CT) and MRI examination were performed for this patient.
Laboratory findings
Increased levels of serum and ascitic fluid amylase. Ascitic fluid amylase up to 25,000 IU. Thus, confirming the diagnosis of pancreatitis.
Imaging findings
Ultrasonogram of epigastric region reveals a cystic lesion with echogenic content within and wall showing the gut signature. Adjacent to it is the accessory pancreatic lobe with a prominent ductal system [Figure 1].
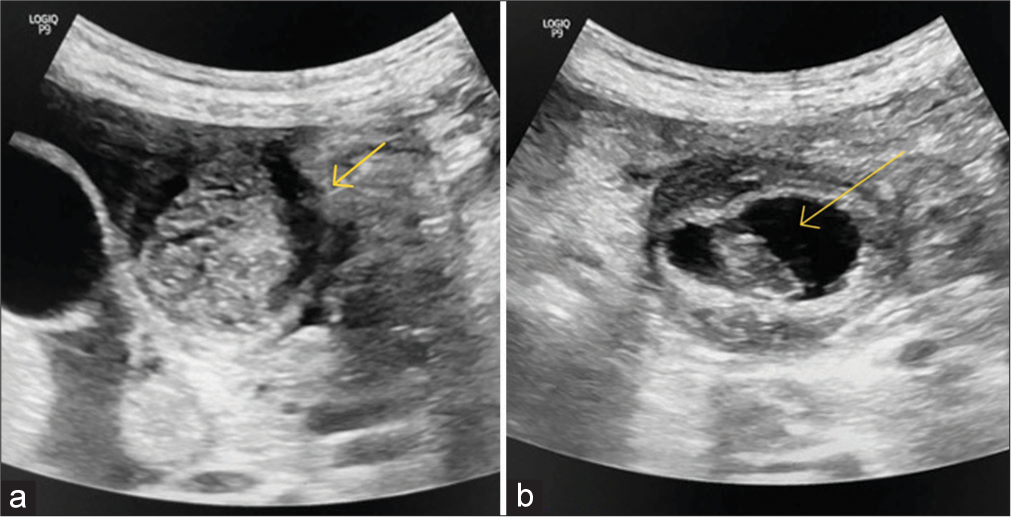
- (a and b) Ultrasonogram of epigastric region reveals a cystic lesion with echogenic content within (yellow arrow in b) and wall showing the gut signature. Adjacent to it is the accessory pancreatic lobe with a prominent ductal system (yellow arrow in a).
Contrast-enhanced CT scan of the abdomen reveals a well-defined cystic lesion with a multi-layered wall in the greater omentum [Figure 2a]. It has an intensely enhancing inner wall with the breech in its superolateral aspect [Figure 2b]. On a plain scan, there is a hyperdense blood clot within the cystic lesion [Figure 2c]. The cyst is sharing a wall with the greater curvature of the stomach [Figure 2d]. The pancreatic body and tail are bulky with prominent main PD and ascites. Accessory pancreatic lobe is seen communicating with the main pancreas. It contains an aberrant duct which communicates with the main PD and cystic lesion [Figure 2e].
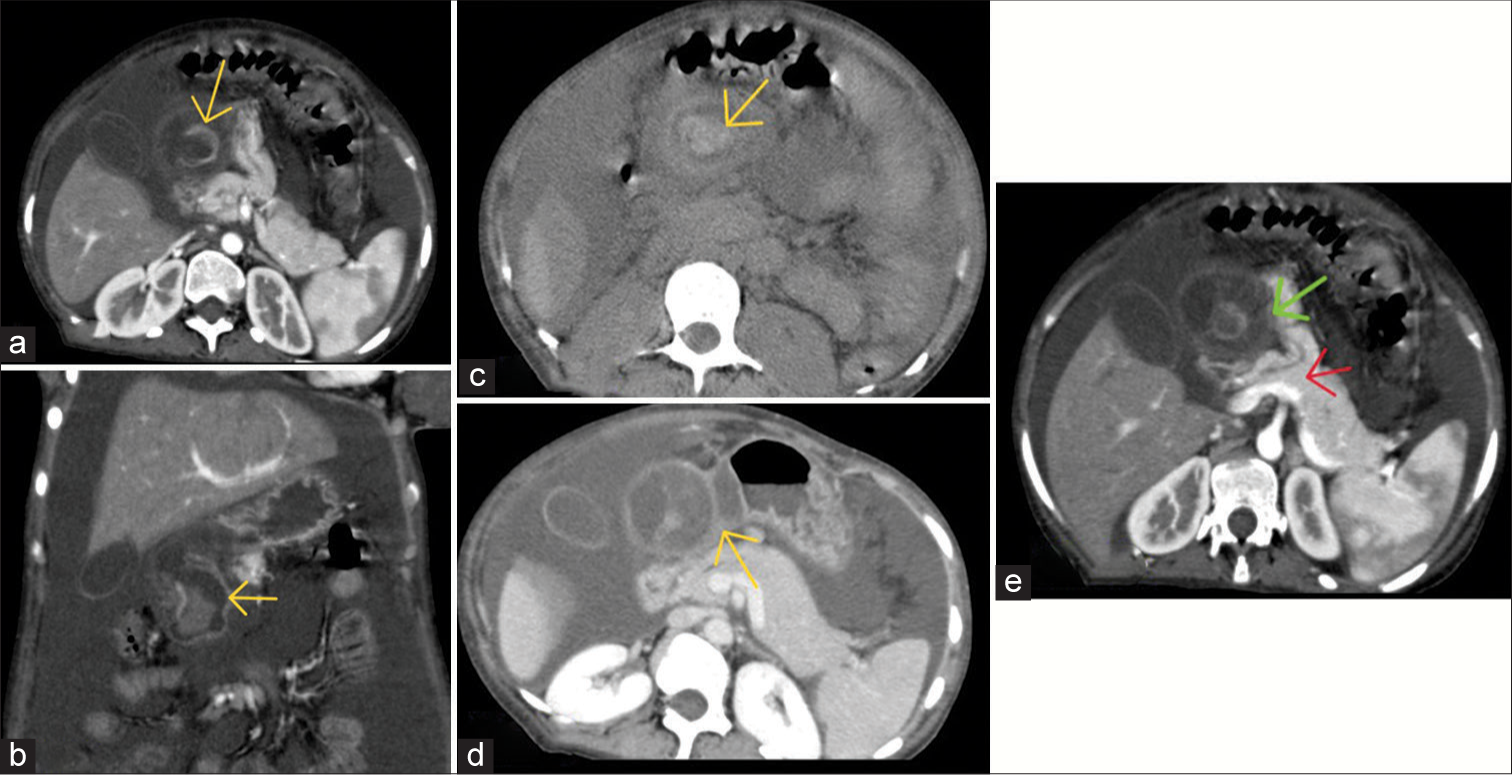
- (a and b) Contrast-enhanced computed tomography scan of the abdomen reveals a well-defined cystic lesion with a multi-layered wall in the greater omentum. It has an intensely enhancing inner wall (yellow arrows) with the breech in its superolateral aspect. (c) On a plain scan, there is a hyperdense blood clot (yellow arrow) within the cystic lesion. (d) The cyst is sharing wall (yellow arrow) with the greater curvature of the stomach. (e) Accessory pancreatic lobe is seen communicating with the main pancreas. It contains an aberrant duct which communicates with the main pancreatic duct (red arrow) and cystic lesion (green arrow).
T2-weighted MRI images of the abdomen confirmed the presence of a T2 hyperintense cystic lesion with a multilayered wall. A breach is seen in its superolateral aspect. 3D image shows the aberrant duct. There is a T2 hypointense content within the cyst suggestive of a blood clot [Figure 3]. As compared to MRI performed in the 7th antenatal month, there is no change in the size of the cyst and no T2 hypointense blood clot within.
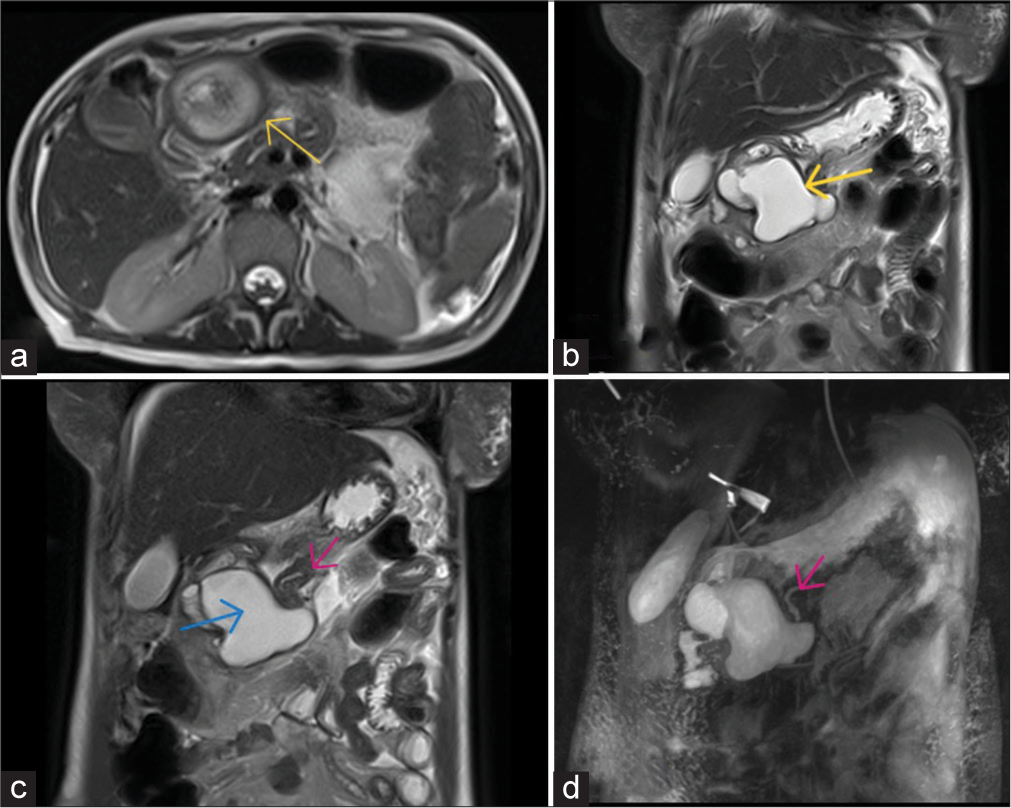
- (a) Axial section of T2-weighted image of magnetic resonance imaging of the abdomen confirms the presence of T2 hyperintense cystic lesion with multilayered (T2 hyperintensehypointense-hyperintense) wall (yellow arrow). (b) Coronal T2-weighted section shows that the cyst is sharing wall with the greater curvature of stomach (yellow arrow). A breech is seen in its superolateral aspect. (c) Coronal T2-weighted section shows the accessory pancreatic lobe with the aberrant duct (pink arrow). There is T2 hypointense content within the cyst suggestive of blood clot (blue arrow). (d) Coronal 3D image shows the aberrant duct (pink arrow).
A radiological diagnosis of accessory pancreatic lobe with gastric duplication cyst with mucosal breach and intracystic hemorrhage leading to pancreatitis was made.
Follow-up
The patient had a poor nutritional built and unstable hemodynamics, so surgery was deferred. Instead, she was taken up for endoscopic retrograde cholangiopancreatography and PD stenting during which she succumbed. She was taken up for post-mortem examination which revealed the ruptured duplication cyst with accessory pancreatic lobe. Postmortem and, therefore, histopathology images are not available as the patient’s relative was not consenting.
DISCUSSION
Duplications of gastrointestinal organs are very rare congenital abnormalities.[2] This gastric anomaly in association with accessory pancreas and pancreatic duplications is rarely reported.[3] The hypothesis for its development states that there is failure of endodermalectodermal separation in 3rd fetal week.[4] This leads to adhesions between them that persist as neurenteric band. This band causes traction along dorsal part of foregut which leads to formation of duplication cyst. As pancreas as well develops from the bud of foregut, traction along the bud due to neurenteric band causes extension of pancreatic tissue and gives rise to an accessory pancreatic lobe.
The gastric duplication cyst usually arises from the greater curvature or posterior wall of stomach. The accessory pancreatic lobe usually stems from neck or body of pancreas and follows ventral direction toward the gastric duplication.[5]
The gastric duplication cyst comprises the inner epithelial lining and outer smooth muscle coat, blood supply originating from gastric vessels, and continuity with gastric wall (luminal continuity may or may not be present).[1]
The cyst mucosa can be gastric mucosa or ectopic pancreatic tissue. This makes it prone to ulceration and bleeding.
Recurrent acute pancreatitis at a younger age is the typical presentation, precipitated by –
Obstruction of PD by the blood of intracystic hemorrhage with subsequent hemoductal pancreatitis.[6]
Mucoid secretions from the cyst with subsequent stasis of pancreatic juice.[7]
Surgical resection of cyst with accessory pancreatic tissue is the treatment of choice.
DIFFERENTIAL DIAGNOSIS
The most common differential diagnosis for a cystic lesion in and around pancreas in a case of pancreatitis is pseudocyst, hence, Table 1 provides points with help differentiate pseudocyst from duplication cyst.
| Pancreatitis with pseudocyst | Gastric duplication cyst |
|---|---|
| Wall of the pseudocyst will show delayed enhancement as it is made of fibrous tissue | Inner mucosal wall shows hyperenhancement |
| Size will decrease on follow-up scan | Size remains constant |
CONCLUSION
This case teaches us the possibility of rare congenital causes of pancreatitis. However, such rare causes are to be considered after ruling out the common causes such as history of alcoholism and gall stones. The ductal system evaluation is extremely important in pancreatitis using magnetic resonance cholangiopancreatography to loom for congenital anomalies of the ductal system.
TEACHING POINTS
Ectopic pancreatic tissue in duplication cysts.
Walls of gastric and intestinal duplication cysts show gut signature.
MCQs
-
Arterial hyperenhancement of cyst wall suggest the diagnosis of
Pancreatic pseudocyst
Duplication cyst
Both
None
Answer Key: b
-
Decrease in size on follow-up scan suggest the diagnosis of
Pancreatic pseudocyst
Duplication cyst
Both
None
Answer Key: a
-
The presence of multi-layered wall is seen in pseudocyst
True
False
Answer Key: b
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Gastric duplication cyst communicating to accessory pancreatic lobe: A case report and review of the literature. World J Clin Cases. 2018;6:1182-8.
- [CrossRef] [PubMed] [Google Scholar]
- Successful laparoscopic resection for gastric duplication cyst: A case report. J Med Case Rep. 2019;13:240.
- [CrossRef] [PubMed] [Google Scholar]
- Gastric, pancreatic, and ureteric duplication. J Indian Assoc Pediatr Surg. 2010;15:25-7.
- [CrossRef] [PubMed] [Google Scholar]
- Rudolf Virchows lecture on general pathological anatomy and general pathology in the year 1852; in commemoration of Virchow's death 50 years ago (5 Sept 1902); comments on the true history of disease] Virchows Arch Pathol Anat Physiol Klin Med. 1952;322:233-9.
- [CrossRef] [PubMed] [Google Scholar]
- Duplicate pancreas meets gastric duplication cyst: A tale of two anomalies. Int J Surg Case Rep. 2013;4:735-9.
- [CrossRef] [PubMed] [Google Scholar]







