Translate this page into:
Unraveling the mystery of a rare neural tube defect: Antenatal sonographic diagnosis with a brief literature review
*Corresponding author: Chandan Kumar Pal, Department of Radio-diagnosis, University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, India. drchandanpal93@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta A, Pal CK, Prakash S, Rathi V. Unraveling the mystery of a rare neural tube defect: Antenatal sonographic diagnosis with a brief literature review. Case Rep Clin Radiol. doi: 10.25259/CRCR_39_2024
Abstract
We present the case of a 42-year-old woman who underwent a level II ultrasound revealing rare and severe fetal anomalies consistent with craniorachischisis. These included absent calvarial bones, exposed cerebral tissue suggestive of acrania-exencephaly, and a spinal defect with diverging laminae and exposed spinal canal indicative of rachischisis. After thorough parental counseling, the mother opted for medical termination of pregnancy. Postnatal confirmation of prenatal sonographic findings underscored the accuracy of the antenatal sonographic diagnosis.
Keywords
Craniospinal rachischisis
Acrania-exencephaly
Rachischisis
Iniencephaly
INTRODUCTION
Craniorachischisis is a rare and severe congenital anomaly characterized by the absence of cranial vault, exposure of cerebral tissue, and an open spinal defect. Prenatal diagnosis of this condition poses significant challenges but is crucial for appropriate parental counseling and management decisions. We report a case of craniorachischisis diagnosed prenatally at our antenatal ultrasound clinic.
CASE REPORT
We report the case of a 42-year-old lady who visited our antenatal ultrasound clinic for a level II ultrasound at a period of gestation of 20 weeks 2 days. The Level 1 ultrasound which was done from an outside center, showed a single live intrauterine pregnancy corresponding to 10 weeks 2 days. No other information was provided. The current pregnancy was spontaneously conceived. The patient was under the care of a polyclinic and reportedly took no medication in the first trimester. She had a healthy girl child of 10 years of age with no reported antenatal and postnatal complications. The patient was a non-smoker, non-alcoholic. Medical and surgical history was insignificant. The second trimester Level II anomaly scan was performed at our outpatient antenatal clinic which revealed the following findings:
The ultrasound showed a live fetus with cardiac activity and a femoral length corresponding to 20 weeks 2 days. The calvarial bones were absent and the cerebral tissue was herniating and exposed to the amniotic fluid suggesting acrania-exencephaly [Figure 1a]. Bilateral orbits appeared prominent and bulging [Figure 1b]. The fetal spine showed an absence of posterior elements and diverging lamina in the contiguous cervical and thoracic regions rendering the spinal canal exposed to the amniotic fluid suggesting rachischisis [Figure 2]. The spinal curvature was also abnormal. Such constellation of findings was highly rare and classical for craniorachischisis. No other associated structural anomaly was found on sonography. After proper parental counseling and discussions about the prognosis, the mother opted for a medical termination of pregnancy. Postnatal images of the fetus confirmed our antenatal sonographic findings [Figure 3].
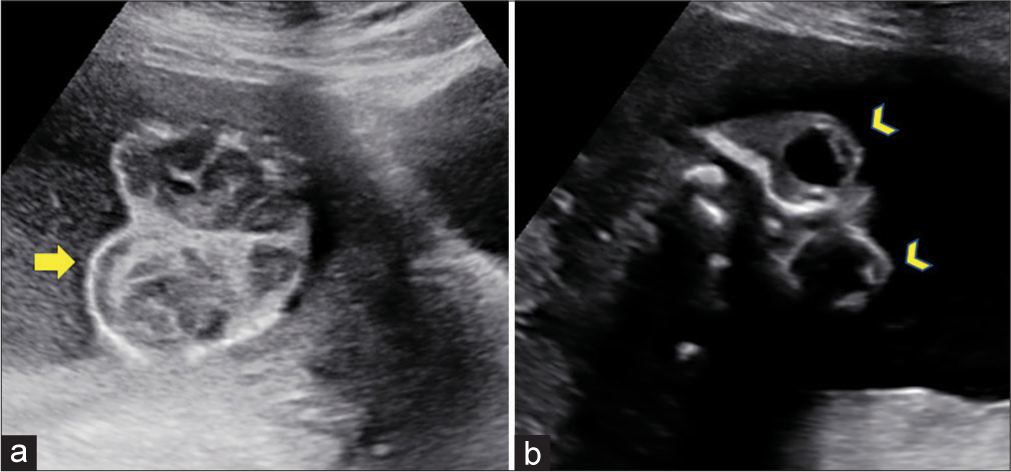
- Antenatal sonographic images of the fetus showing (a) absent calvarium with brain parenchyma freely exposed to the amniotic fluid (yellow arrow) suggesting acrania-exencephaly sequence and (b) bulging eyes with absent calvarium giving the classic “frog-eye” appearance (yellow arrowheads).
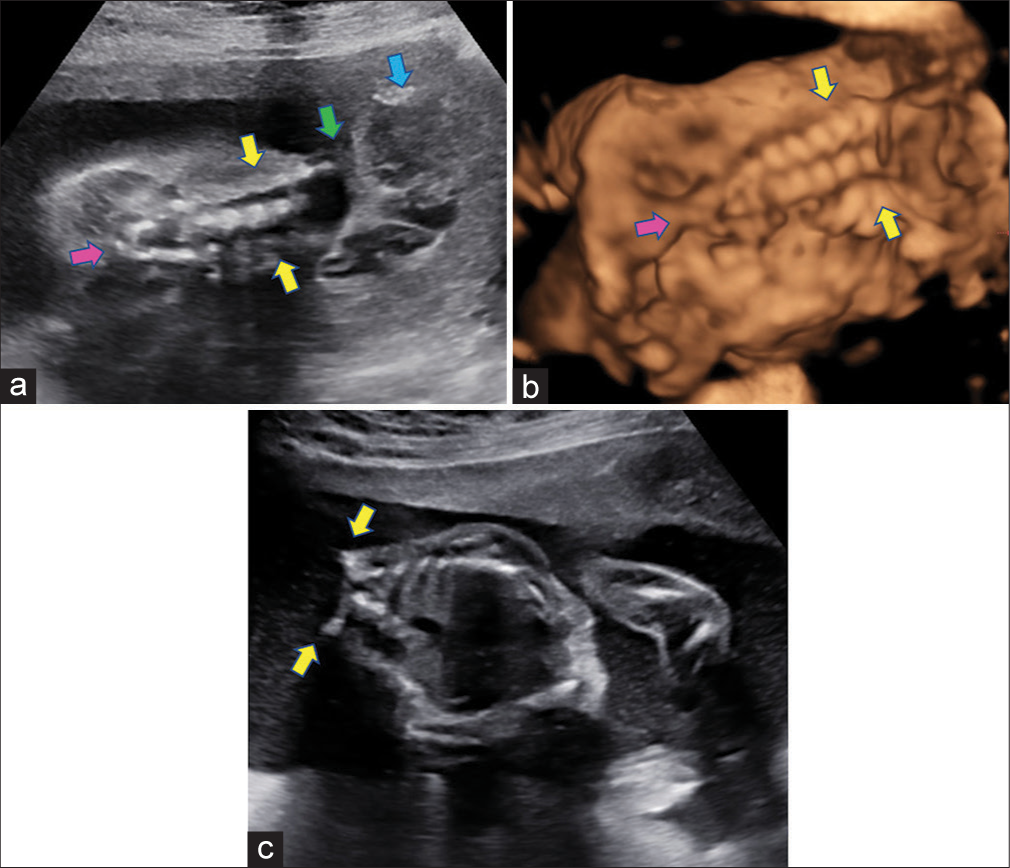
- (a) Antenatal sonographic images of the fetus in the coronal plane of the fetus showing the fetal spine with widely splayed lamina at all levels (yellow arrows) with progressive narrowing and fusion at the caudal aspect (pink arrow). Also depicted is the absence of calvarium and exencephaly of the cerebral tissue (blue arrow) and the contiguity between the cranial and spinal defect (green arrow). (b) Antenatal 3 dimensional surface rendered images of the fetus in coronal plane reaffirming the findings and showing widely splayed lamina (yellow arrows), fusing inferiorly (pink arrow). (c) Antenatal sonographic images of the fetus in the axial/oblique plane showing absence of vertebral posterior elements with widely splayed laminae (yellow arrows), exposing the spinal cord to amniotic cavity suggesting rachischisis.
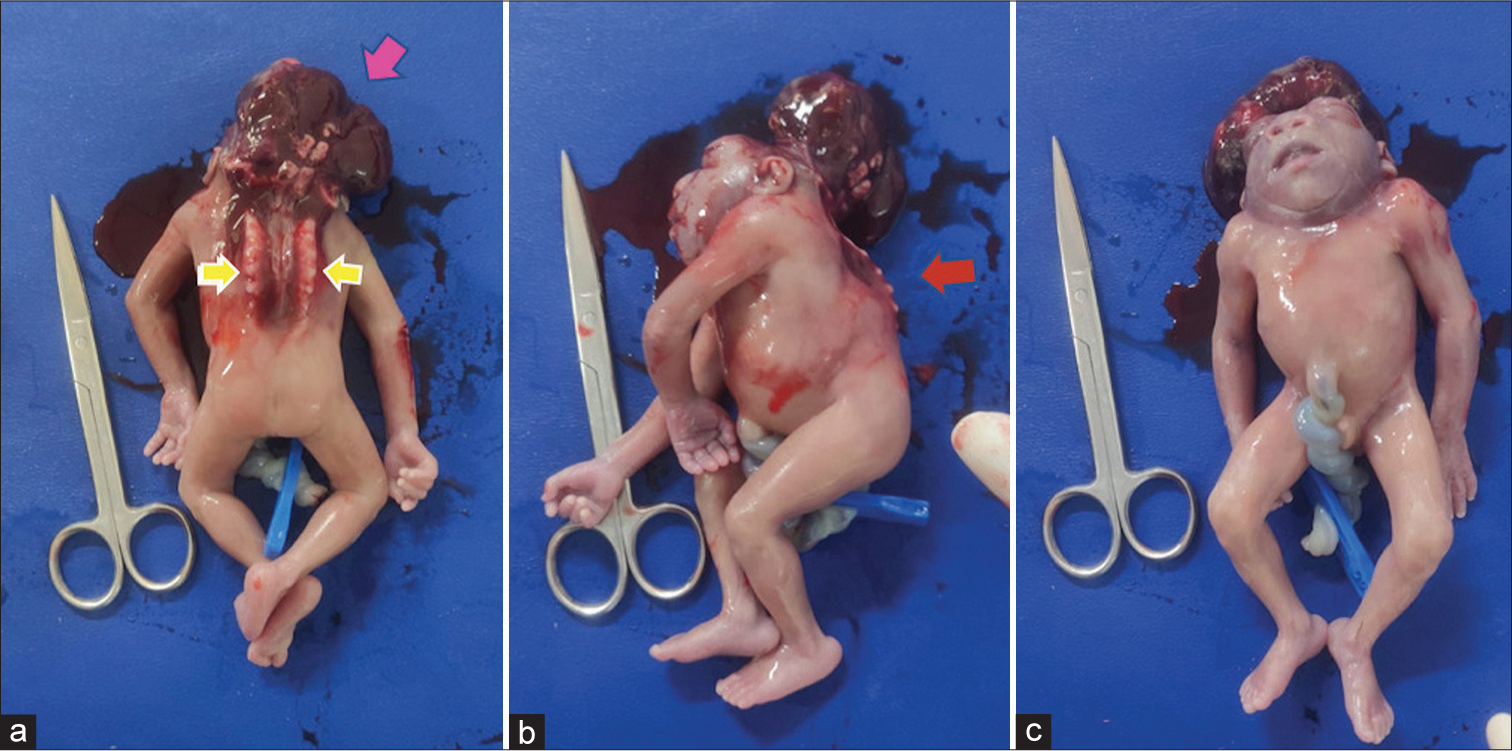
- Postnatal images of the fetus (a) showing absent calvarium with exposed cerebral tissue (pink arrow) and contiguous rachischisis of the cervicothoracic spine (yellow arrows) confirming our antenatal diagnosis of craniospinal rachischisis. (b) Similar findings depicted in the sagittal plane. Note the abnormal spinal curvature (red arrow). Also, note the neutral position of fetal head in relation to the body and absence of thick skin covering the herniated structures which ruled out iniencephaly. (c) Note the prominent orbital structures, broad nose, absence of a distinguished neck structure, and low-set ears.
DISCUSSION
Neural tube defects comprise the most common birth defects in India with the prevalence at birth highest in the northern region at 7.7 cases per 1000 births.[1] While treatment options do exist for spina bifida and encephaloceles, neural tube defects (NTDs) such as acrania–exencephaly–anencephaly sequence, craniorachischisis and iniencephaly are invariably fatal.[2]
Craniospinal rachischisis is a lethal, non-syndromic anomaly, resulting from the failed closure of anterior neuropore during the 3rd – 4th week of gestation.[3] It is characterized by the combination of anencephaly (absence of the brain and cranial vault, without skin covering) with a contiguous bony defect in the spine (also without meninges covering the neural tissue – rachischisis).[4] Associated findings such as bulging eyes, broad nose, folded ears, protruded tongue, and absent neck have been frequently reported.[5,6] Antenatal ultrasound is the mainstay of diagnosis and facilitates early termination of pregnancy. Three-dimensional ultrasound can be used as an adjunct to conventional two-dimensional ultrasound to increase diagnostic confidence.
The development and closure of the neural tube are normally completed within 28 days after conception before many women are aware that they are pregnant. Hence, it is recommended that women capable of becoming pregnant should consume 400 mcg of folic acid per day.[7,8]
The acrania-exencephaly sequence in association with a contiguous spinal rachischisis in our case helped us reach a diagnosis of craniospinal rachischisis with certainty. In addition, the neutral position of fetal head with relation to spine, floating cerebral tissue exposed to amniotic fluid without a superficial skin covering and absence of other structural anomalies helped us rule out Iniencephaly in this case, which is a close differential of the former [Table 1].[9,10]
| Classical features | Differentiating features | |
|---|---|---|
| Craniospinal rachischisis | Presence of: Anencephaly with a contiguous bony defect of the spine | No skin covering and no meningeal covering No associated systemic anomalies (non-syndromic) |
| Iniencephaly apertus | 3 major diagnostic criteria: - Deficiency of occiput in the region of foramen magnum (with the presence of encephalocele in iniencephaly apertus) - Spina bifida with rachischisis of cervical and thoracic spine - Fixed retroflexion of the head |
Presence of uninterrupted thick skin covering the retroflexed head Associated with systemic anomalies “Star-gazing” appearance of fetus |
It is imperative for radiologists to be familiar with these entities for early diagnosis and timely counseling of the patient so that the patient can make an informed decision.
CONCLUSION
This case highlights the importance of detailed ultrasound evaluation in detecting rare fetal anomalies and facilitating informed decision-making regarding pregnancy management.
TEACHING POINTS
Craniospinal rachischisis is a rare fatal NTD with the presence of anencephaly and a contiguous spinal rachischisis. The absence of meningeal and skin covering is the hallmark
It is a non-syndromic anomaly with reported associated occurrence of bulging eyes, broad nose, folded ears, and absent neck
Antenatal ultrasound facilitates early diagnosis of this fatal entity and timely termination of pregnancy.
MCQs
-
Which of the following is associated with a star-gazing fetus?
Anencephaly
Spina bifida
Craniorachischisis
Iniencephaly
Answer Key: d
-
Which of the following is not seen in craniospinal rachischisis?
Acrania–exencephaly–anencephaly sequence
Thick skin covering the retroflexed head
Contiguous cranial and spinal defect
Rachischisis
Answer: b
-
Which of the following is not true about craniospinal rachischisis?
It is a non-syndromic NTD
Perinatal folic acid supplementation is preventive
Overgrowth of upper limbs is reported
Bulging of eyes is seen
Answer: c
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Birth prevalence of neural tube defects and orofacial clefts in India: A systematic review and meta-analysis. PLoS One. 2015;10:e0118961.
- [CrossRef] [PubMed] [Google Scholar]
- Neural tube defects. 2019. Radiology key. Available from: https://radiologykey.com/neural-tube-defects-2 [Last accessed on 2024 Mar 21]
- [Google Scholar]
- Two cases of craniospinal rachischisis totalis: Role of magnetic resonance imaging in diagnosis and review of neural tube defects in the Indian context with implications for folate fortification. J Pediatr Neurosci. 2017;12:32-5.
- [CrossRef] [PubMed] [Google Scholar]
- Lethal neural tube defects: Reports of anencephaly and craniorachischisis cases and literature review. Case Rep Obstet Gynecol. 2023;2023:4017625.
- [CrossRef] [PubMed] [Google Scholar]
- Folic acid In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554487 [Last accessed on 2024 Mar 21]
- [Google Scholar]
- Craniorachischisis totalis. J Neurosci Rural Pract. 2010;1:54-5.
- [CrossRef] [PubMed] [Google Scholar]
- Iniencephaly: Radiologic and pathomorphologic perinatal observation. Radiol Case Rep. 2020;16:201-4.
- [CrossRef] [PubMed] [Google Scholar]
- Iniencephaly: Radiological and pathological features of a series of three cases. J Neurosci Rural Pract. 2014;5:389-93.
- [CrossRef] [PubMed] [Google Scholar]








