Translate this page into:
Two rare cases of idiopathic spontaneous extra-axial spinal hematoma
*Corresponding author: K. Nadanasadharam, Department of Radiology, Meenakshi Hospital, Thanjavur, Tamil Nadu, India. nadanasadharam912@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shanmuga Jayanthan S, Rupesh G, Vimalan P, Nadanasadharam K. Two rare cases of idiopathic spontaneous extra-axial spinal hematoma. Case Rep Clin Radiol. 2024;2:3-7. doi: 10.25259/CRCR_81_2023
Abstract
Spinal hematoma is a rare condition but can cause significant spinal injury and resultant morbidity. Magnetic resonance imaging (MRI) is the gold standard of radiological investigation and is often an emergency indication for imaging. Early diagnosis is crucial for treatment and better patient outcome. Herein, we report two cases of rare idiopathic spontaneous extra-axial hematoma highlighting the role of MRI in the diagnosis.
Keywords
Extra-axial spinal hematoma
Laminectomy
Spontaneous spinal epidural hematoma
Spontaneous spinal subdural hematoma
INTRODUCTION
Radiologic evaluation is an essential component for the diagnosis of spinal hematomas, which is often a diagnostic dilemma. The spinal hematomas can be classified based on the anatomical location as follows: Epidural, subdural, subarachnoid, and intramedullary (spinal cord) hematomas.[1] Among these subtypes, spontaneous epidural and subdural spinal hematoma are rare and differentiating them is a diagnostic challenge. Often unique radiologic signs can be used to distinguish these types of spinal hemorrhage. Understanding the imaging anatomy of spinal compartments and imaging characteristics of different stages of spinal compartments is essential for the confident imaging diagnosis of spinal hematomas and to identify the correct location.[1,2] Magnetic resonance imaging (MRI) is preferred imaging modality of choice to correctly diagnose the location and stages of the hematoma.[1]
CASE 1
A 59-year-old male presented to emergency room with chief complaints of weakness and numbness in all limbs for the past 3 days. He had a history of fever a week ago following which he developed sudden weakness. There is no history of recent trauma, weight loss, infection, or neck/back pain and any anticoagulant use or significant past/surgical history. He is recently diagnosed with uncontrolled diabetes mellitus (DM). On examination: Cranial nerves - intact; vitals - stable; temperature - afebrile; neurological examination showed sensory loss below T4 dermatome; and motor examination: Bilateral lower limb - 0/5; right biceps - 3/5 and other muscles - 2/5; and left biceps - 2/5 and other muscles - 0/5; deep tendon reflex: Absent. The laboratory examination of the patient was normal, prothrombin time-international normalized ratio (PT-INR): 1.07, activated partial thromboplastin time (APTT): 25.5, and platelet count: 2,34,000. The patient was referred to MRI for further evaluation.
Imaging findings
T1-weighted (T1W) and T2-weighted (T2W) sagittal sections of cervical spine show a well-defined hyperintense extra-axial lesion at C4-5 vertebral level [Figure 1]. T2/short-tau inversion recovery hyperintensities noted in cervical spinal cord, suggestive of cord edema [Figure 1]. T1 FATSAT (FS) sagittal section of cervical spine shows hyperintense extra-axial lesion of size (0.7 × 0.9 cm) with no demonstrable contrast enhancement on T1FS+c [Figure 1]. T2 gradient axial section shows areas of blooming within the lesion [Figure 1]. From the above imaging findings, the diagnosis of spinal epidural hematoma (SEH) was made. The patient underwent emergency decompression: Laminectomy was done and epidural hematoma was confirmed pre-operatively followed by evacuation.
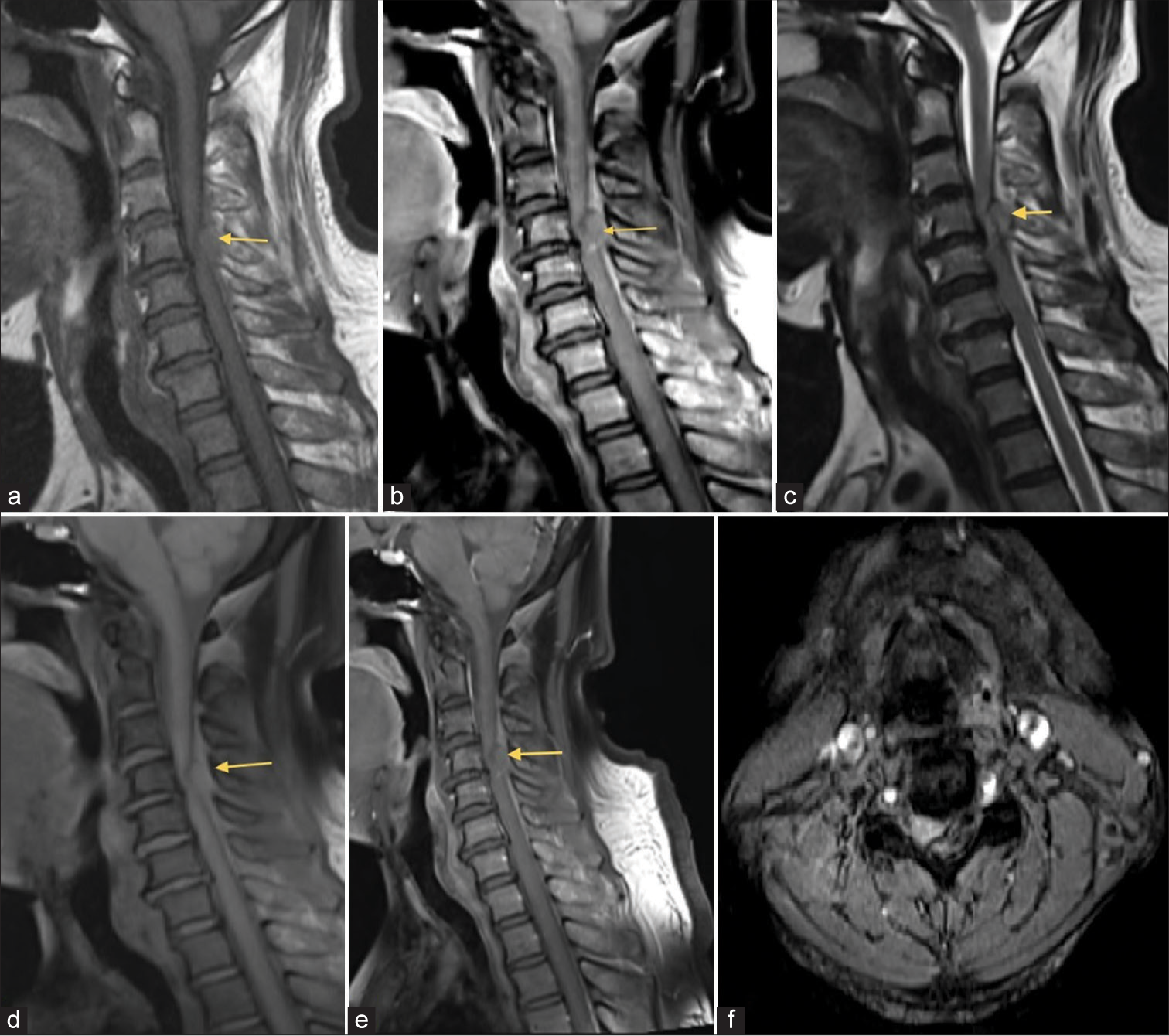
- T1-weighted (T1W) (a) and T2-weighted (T2W) (b) sagittal sections of cervical spine show a well-defined hyperintense extra-axial lesion at C4-5 vertebral level. T2W (c) sagittal section shows hyperintensities in cervical spinal cord suggestive of cord edema. T1 FAT-SAT (d) sagittal section of cervical spine shows hyperintense extra-axial lesion of size (0.7 × 0.9 cm). T1FS+c (e) shows no demonstrable post contrast enhancement. T2 gradient (f) axial shows areas of blooming within the lesion.
CASE 2
A 65-year-old male presented with chief complaints of bilateral lower limb weakness and difficulty in walking with pain for 3 days. There is no history of trauma or fever. This is not a known case of DM or hypertension. On examination: Conscious and oriented and cranial nerves – intact, vitals – stable, and temperature - afebrile; neurological examination: Bilateral lower limbs - 3/5 and plantar and extensor refluxes - absent; it is worth to mention that he had a history of bilateral spontaneous intracranial non-traumatic idiopathic subdural hemorrhage for which craniotomy was done, 1 year back. The laboratory examination of the patient was normal, PT-INR: 1.08, APTT: 30.3, platelet count: 3,05,000. The patient was referred to MRI for further evaluation.
Imaging findings
T1W and T2W sagittal sections of whole spine show long segment extra-axial hyperintensity extending from D6 to L5 vertebral levels [Figure 2]. T1 FS sagittal section of whole spine shows no demonstrable signal suppression [Figure 2]. T2 gradient sagittal section shows peripheral hypointense hemosiderin rim [Figure 2]. There is no suspicious lesion or abnormal signal intensity in spinal cord. The diagnosis of spinal extra-axial subdural hematoma was made. The patient underwent emergency decompressive surgery: Laminectomy and durotomy were done with evacuation of the subdural hematoma.

- T1-weighted (a) and T2-weighted (b) sagittal sections of whole spine show long segment extra-axial hyperintensity extending from D6 to L5 vertebral levels. T1 FAT-SAT (c) sagittal section of whole spine shows no demonstrable signal suppression. T2 gradient (d) sagittal section shows peripheral hypointense hemosiderin rim.
DISCUSSION
The spinal cord is covered by three layers of meninges and the extra-axial anatomical spaces are divided into subarachnoid, subdural, and epidural compartments.[1] The three layers of meninges are pia, arachnoid, and dura from inner to outer aspect of spinal cord.[1] There are no bridging veins in subdural space unlike epidural space, and hence, hemorrhage in the later compartment is more common and it is the reversal in case of brain.[1]
Spontaneous SEH is a rare condition (0.1/100,000 patients/year) and spinal subdural hematoma (SSH) is still more uncommon.[2,3] The first case of epidural hematoma was reported in 1869 by Jackson, and he termed it as a “case of spinal apoplexy.” Although various causes of SEH include, anticoagulant therapy, coagulopathies, vascular malformations, tumors, pregnancy, and Paget’s disease; more than 40–50% cases are idiopathic and commonly seen at cervicothoracic region.[3]
Spontaneous SSH is extremely rare, representing only ~4.1% of all intraspinal hematomas.[4] Most cases are idiopathic like SEH and more common in lower thoracic region.[4] The clinical manifestation is common for either condition, which is progressive motor weakness. In addition, 50% of patients will refer an intense spear-like pain in SSH at the site of hemorrhage.[4] MRI is the imaging modality of choice in the diagnosis of spinal hematomas.[2,4]
Ageing of hematoma can be classified as follows: Hyper acute (<12 h), acute (12–72 h), subacute (3 days–2 weeks), and chronic (>2 weeks).[4] Accordingly, the signal intensity varies in MRI with respect to different stages of hematoma.[4-6] At hyper-acute stage, the hematoma is isointense on T1- and hyperintense on T2-weighted images (T2-WI), compared to spinal cord. In acute early subacute stages, the hematoma shows heterogeneous signal intensity with hyperintense areas on T1- and T2-WI. At late subacute stage, the hemorrhage is hyperintense on both T1- and T2-WI. In chronic phase, the hematoma is hypointense on both T1- and T2-WI.[5]
In addition, MR can localize the compartment of the hemorrhage by identification of the dura.[7-9] The “inverted Mercedes-Benz sign” is a very useful sign, if present, to differentiate SSH from SEH. It is seen on the axial image at the level of the denticulate ligaments, with a pair of denticulate ligaments and the dorsal septum constitutes the three radiating spikes of the sign, while the SSH expands and fills the three loculations in-between.[8,9] The SEH causes ventral displacement of dura, which is seen as hypointense curvilinear rim on sagittal T1- and T2-WI. The “cup sign” caused by epidural fat displacement is another characteristic finding, useful in differentiating SEH from SSH.[10]
DIFFERENTIATING FEATURES
Subdural vs epidural spinal hematoma - Differentiating features [Table 1].
| Epidural spinal hematoma | Subdural spinal hematoma |
|---|---|
| Relatively more common (0.1/100,000 patients per year) | Extremely rare (4.1% of all intraspinal hematomas) |
| Site: Occurs outside the dura with inward displacement of dura | Site: Occurs within the dura with outward displacement of dura |
| The inner contour of epidural hematoma is usually smooth | The inner contour of a subdural hematoma is irregular |
| Epidural fat displacement | Epidural fat is preserved |
| Cup sign | Inverted Mercedes-Benz sign |
CONCLUSION
Early decompressive surgery results in favorable prognosis. The neurologic recovery after surgery varies with the severity of the pre-operative impairment and the interval between presentation and operation. Hence, the accurate diagnosis and timely intervention are crucial.[11] Laminectomy with evacuation of hematoma would be sufficient in epidural hematoma, while additional durotomy is required in subdural hemorrhage.
TEACHING POINTS
MRI plays an important role in the diagnosis and differentiation of extra-axial spinal hematoma.
Early diagnosis is crucial as it requires immediate surgical intervention to avoid permanent neurological deficits.
MCQs
-
Cup sign is present in which of the spinal hematoma’s
Epidural hematoma
Subdural hematoma
Subarachnoid hematoma
None of the above
Answer Key: a
-
Inverted Mercedes-Benz sign is present in which of the spinal hematoma’s
Epidural hematoma
Subdural hematoma
Subarachnoid hematoma
None of the above
Answer Key: b
-
All are features of epidural spinal hematoma except
Outward displacement of dura
Smooth inner contour
Cup sign
Preserved epidural fat
Answer Key: d
Acknowledgments
Dr. M. Karthikeyan MS, DNB, Consultant Orthopaedic and Spine Surgeon - Meenakshi Hopital, Tanjore. Dr. S. Shanumga Hariharan DNB, Consultant Orthopaedic and Spine Surgeon - Meenakshi Hopital, Tanjore. Dr. N. Arun Kumar MCh, Consultant Neurosurgeon - Meenakshi Hopital, Tanjore.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- MR imaging of spinal haematoma: A pictorial review. Br J Radiol. 2019;92:20180532.
- [CrossRef] [PubMed] [Google Scholar]
- Acute spinal extradural hematoma and cord compression: Case report and a literature review. Cureus. 2020;12:e11603.
- [CrossRef] [Google Scholar]
- Spinal hematoma: A literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003;26:1-49.
- [CrossRef] [PubMed] [Google Scholar]
- MRI findings in spinal subdural and epidural hematomas. Eur J Radiol. 2007;64:119-25.
- [CrossRef] [PubMed] [Google Scholar]
- Nonsurgical treatment of an upper thoracic spinal subdural hemorrhage. Spinal Cord. 2001;39:657-61.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal subdural hematoma: A rare case of spinal subdural hematoma complicating routine, minimally invasive lumbar discectomy and decompression and relevant literature review. J Spine Surg. 2017;3:112-8.
- [CrossRef] [PubMed] [Google Scholar]
- Inverted Mercedes Benz sign in lumbar spinal subdural hematoma. J Emerg Med. 2014;47:692-3.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal hematomas: What a radiologist needs to know. Radiographics. 2018;38:1516-35.
- [CrossRef] [PubMed] [Google Scholar]
- Contrast enhancement patterns of acute spinal epidural hematomas: A report of two cases. AJNR Am J Neuroradiol. 2003;24:366-9.
- [Google Scholar]
- A rare case of spontaneous spinal epidural hematoma in a 43-year-oldman. JACEP Open. 2021;2:e12532.
- [CrossRef] [Google Scholar]







